Ann Dermatol.
2013 Aug;25(3):327-334. 10.5021/ad.2013.25.3.327.
Onychomycosis in Children: An Experience of 59 Cases
- Affiliations
-
- 1Department of Dermatology, Dongguk University College of Medicine, Gyeongju, Korea. smg@dongguk.ac.kr
- 2Department of Laboratory Medicine, Dongguk University College of Medicine, Gyeongju, Korea.
- KMID: 2265873
- DOI: http://doi.org/10.5021/ad.2013.25.3.327
Abstract
- BACKGROUND
Although tinea unguium in children has been studied in the past, no specific etiological agents of onychomycosis in children has been reported in Korea.
OBJECTIVE
The purpose of this study was to investigate onychomycosis in Korean children.
METHODS
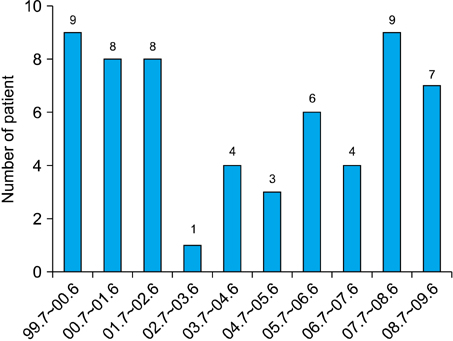
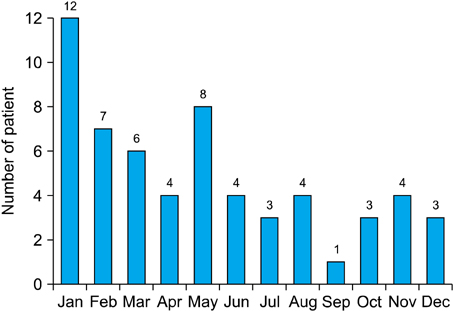
We reviewed fifty nine patients with onychomycosis in children (0~18 years of age) who presented during the ten-year period between 1999 and 2009. Etiological agents were identified by cultures on Sabouraud's dextrose agar with and without cycloheximide. An isolated colony of yeasts was considered as pathogens if the same fungal element was identified at initial direct microscopy and in specimen-yielding cultures at a follow-up visit.
RESULTS
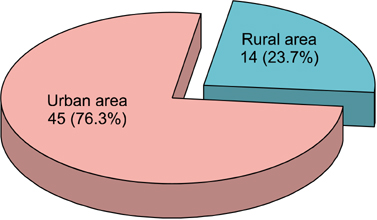
Onychomycosis in children represented 2.3% of all onychomycosis. Of the 59 pediatric patients with onychomycosis, 66.1% had toenail onychomycosis with the rest (33.9%) having fingernail onychomycosis. The male-to-female ratio was 1.95:1. Fourteen (23.7%) children had concomitant tinea pedis infection, and tinea pedis or onychomycosis was also found in eight of the parents (13.6%). Distal and lateral subungual onychomycosis was the most common (62.7%) clinical type. In toenails, Trichophyton rubrum was the most common etiological agent (51.3%), followed by Candida albicans (10.2%), C. parapsilosis (5.1%), C. tropicalis (2.6%), and C. guilliermondii (2.6%). In fingernails, C. albicans was the most common isolated pathogen (50.0%), followed by T. rubrum (10.0%), C. parapsilosis (10.0%), and C. glabrata (5.0%).
CONCLUSION
Because of the increase in pediatric onychomycosis, we suggest the need for a careful mycological examination of children who are diagnosed with onychomycosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Verma S, Heffernan MP. Superficial fungal infections: dermatophytosis, onychomycosis, tinea nigra, piedra. In : Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw-Hill;2008. p. 1807–1821.2. Chang P, Logemann H. Onychomycosis in children. Int J Dermatol. 1994; 33:550–551.
Article3. Ploysangam T, Lucky AW. Childhood white superficial onychomycosis caused by Trichophyton rubrum: report of seven cases and review of the literature. J Am Acad Dermatol. 1997; 36:29–32.
Article4. Gupta AK, Sibbald RG, Lynde CW, Hull PR, Prussick R, Shear NH, et al. Onychomycosis in children: prevalence and treatment strategies. J Am Acad Dermatol. 1997; 36:395–402.
Article5. Lateur N, Mortaki A, André J. Two hundred ninety-six cases of onychomycosis in children and teenagers: a 10-year laboratory survey. Pediatr Dermatol. 2003; 20:385–388.
Article6. Romano C, Papini M, Ghilardi A, Gianni C. Onychomycosis in children: a survey of 46 cases. Mycoses. 2005; 48:430–437.
Article7. Sigurgeirsson B, Kristinsson KG, Jonasson PS. Onychomycosis in Icelandic children. J Eur Acad Dermatol Venereol. 2006; 20:796–799.
Article8. Lange M, Roszkiewicz J, Szczerkowska-Dobosz A, Jasiel-Walikowska E, Bykowska B. Onychomycosis is no longer a rare finding in children. Mycoses. 2006; 49:55–59.
Article9. Gunduz T, Metin DY, Sacar T, Hilmioglu S, Baydur H, Inci R, et al. Onychomycosis in primary school children: association with socioeconomic conditions. Mycoses. 2006; 49:431–433.
Article10. Martinez Roig A, Torres Rodriguez JM. Twelve cases of tinea unguium in a pediatric clinic in 9 years. Eur J Pediatr. 2007; 166:975–977.
Article11. Bonifaz A, Saúl A, Mena C, Valencia A, Paredes V, Fierro L, et al. Dermatophyte onychomycosis in children under 2 years of age: experience of 16 cases. J Eur Acad Dermatol Venereol. 2007; 21:115–117.
Article12. Leibovici V, Evron R, Dunchin M, Westerman M, Ingber A. A population-based study of toenail onychomycosis in Israeli children. Pediatr Dermatol. 2009; 26:95–97.
Article13. Zac RI, Café ME, Neves DR, E Oliveira PJ, Barbosa VG. Onychomycosis in a very young child. Pediatr Dermatol. 2009; 26:761–762.
Article14. Sachdeva S, Gupta S, Prasher P, Aggarwal K, Jain VK, Gupta S. Trichophyton rubrum onychomycosis in a 10-week-old infant. Int J Dermatol. 2010; 49:108–109.
Article15. Rodríguez-Pazos L, Pereiro-Ferreirós MM, Pereiro M Jr, Toribio J. Onychomycosis observed in children over a 20-year period. Mycoses. 2011; 54:450–453.
Article16. Choo EH, Choi GJ, Cho BK. Mycological and clinical study on dermatophytoses in infants and preschoolers. Korean J Dermatol. 1984; 22:369–374.17. Suh MK, Choi SK, Kim SH, Suh SB, Sung YO, Oh SH. Tinea pedis & tinea manus in children. Korean J Dermatol. 1993; 31:713–719.18. Lee JH, Chung HJ, Lee KH. A clinical and mycological study on dermatophytoses in children. Korean J Med Mycol. 2002; 7:209–216.19. Baran R, Hay RJ, Tosti A, Haneke E. A new classification of onychomycosis. Br J Dermatol. 1998; 139:567–571.
Article20. English MP. Nails and fungi. Br J Dermatol. 1976; 94:697–701.
Article21. Lange M, Nowicki R, Barańska-Rybak W, Bykowska B. Dermatophytosis in children and adolescents in Gdansk, Poland. Mycoses. 2004; 47:326–329.
Article22. Hwang SM, Kim DM, Suh MK, Kwon KS, Kim KH, Ro BI, et al. Epidemiologic survey of onychomycosis in Koreans: multicenter study. Korean J Med Mycol. 2011; 16:35–43.
Article23. Lim SW, Suh MK, Ha GY. Clinical features and identification of etiologic agents in onychomycosis (1999-2002). Korean J Dermatol. 2004; 42:53–60.24. Suh MK, Sung YO, Ha GY. Dermatophytoses in Kyongju area. Korean J Dermatol. 1995; 33:294–302.25. Park JK, Kwon KS, Yu HJ. A clinical study of onychomycosis. Korean J Med Mycol. 2005; 10:46–54.26. Sohn JK, Lee SH. Onychomycosis in the elderly. Korean J Med Mycol. 2001; 6:77–83.27. Tullio V, Banche G, Panzone M, Cervetti O, Roana J, Allizond V, et al. Tinea pedis and tinea unguium in a 7-year-old child. J Med Microbiol. 2007; 56:1122–1123.
Article28. Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol. 2010; 28:151–159.
Article29. Inanir I, Sahin MT, Gündüz K, Dinç G, Türel A, Arisoy A, et al. Case report. Tinea pedis and onychomycosis in primary school children in Turkey. Mycoses. 2002; 45:198–201.
Article30. Chun DK, Lee UH, Park HS, Choi JC. Onychomycosis in a premature infant caused by Candida tropicalis. J Eur Acad Dermatol Venereol. 2004; 18:617–618.
Article31. Gupta AK, Skinner AR. Onychomycosis in children: a brief overview with treatment strategies. Pediatr Dermatol. 2004; 21:74–79.
Article