Korean J Hepatobiliary Pancreat Surg.
2013 Feb;17(1):14-20. 10.14701/kjhbps.2013.17.1.14.
Living donor liver transplantation for patients with alcoholic liver disease
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2243164
- DOI: http://doi.org/10.14701/kjhbps.2013.17.1.14
Abstract
- BACKGROUNDS/AIMS
Since most transplantation studies for alcoholic liver disease (ALD) were performed on deceased donor liver transplantation, little was known following living donor liver transplantation (LDLT).
METHODS
The clinical outcome of 18 ALD patients who underwent LDLT from Febraury 1997 to December 2004 in a large-volume liver transplantation center was assessed retrospectively.
RESULTS
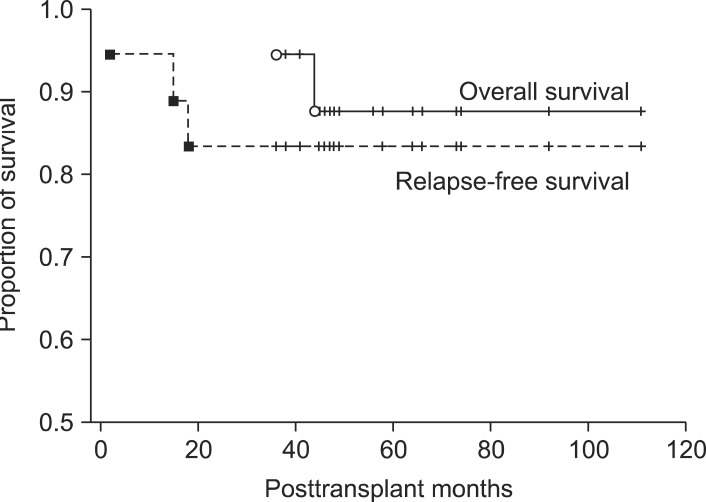
The model for end-stage liver disease score was 23+/-11, and mean pretransplant abstinence period was 16+/-13 months, with 14 (77.8%) patients being abstinent for at least 6 months. Graft types were right lobe grafts in 11, left lobe grafts in 2 and dual grafts in 5. Graft to recipient body weight ratio was 0.94+/-0.16. The relapse rates in patients who did and did not maintain 6 months of abstinence were 7.1% and 50%, respectively (p=0.097). Younger recipient age was a significant risk factor for alcohol relapse (p=0.027). Five recipients with antibody to hepatitis B surface antigen (HBsAg) received core antibody-positive liver graft, but two of them showed positive HBsAg seroconversion. Overall 5-year patient survival rate following LDLT was 87.8%, with a 5-year relapse rate of 16.7%.
CONCLUSIONS
Pretransplant abstinence for 6 months appears to be benefical for preventing posttransplant relapse. Life-long prophylactic measure should be followed after use of anti-HBc-positive liver grafts regardless of hepatitis B viral marker status of the recipient.
MeSH Terms
Figure
Cited by 1 articles
-
Changes in the indications for living donor liver transplantation: single-institution experience of 3,145 cases over 10 years
Sang-Hyun Kang, Shin Hwang, Chul-Soo Ahn, Ki-Hun Kim, Deok-Bog Moon, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Jung-Man Namgoong, Young-In Yoon, Hui-Dong Cho, Jae-Hyun Kwon, Yong-Kyu Chung, Jin-Uk Choi, Sung-Gyu Lee
Korean J Transplant. 2020;34(1):47-54. doi: 10.4285/kjt.2020.34.1.47.
Reference
-
1. Pageaux GP, Michel J, Coste V, et al. Alcoholic cirrhosis is a good indication for liver transplantation, even for cases of recidivism. Gut. 1999; 45:421–426. PMID: 10446113.
Article2. Hwang S, Lee SG, Kim KK, et al. Efficacy of 6-month pretransplant abstinence for patients with alcoholic liver disease undergoing living donor liver transplantation. Transplant Proc. 2006; 38:2937–2940. PMID: 17112869.
Article3. Lee SG, Park KM, Hwang S, et al. Adult-to-adult living donor liver transplantation at the Asan Medical Center, Korea. Asian J Surg. 2002; 25:277–284. PMID: 12470999.
Article4. Hwang S, Lee SG, Lee YJ, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–927. PMID: 16721780.
Article5. Mathurin P. Is alcoholic hepatitis an indication for transplantation? Current management and outcomes. Liver Transpl. 2005; (11 Suppl 2):S21–S24. PMID: 16237730.
Article6. Veldt BJ, Lainé F, Guillygomarc'h A, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol. 2002; 36:93–98. PMID: 11804670.
Article7. Maddrey WC, Boitnott JK, Bedine MS, et al. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978; 75:193–199. PMID: 352788.
Article8. Mathurin P, Mendenhall CL, Carithers RL Jr, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol. 2002; 36:480–487. PMID: 11943418.
Article9. Dunn W, Jamil LH, Brown LS, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology. 2005; 41:353–358. PMID: 15660383.
Article10. Burra P, Lucey MR. Liver transplantation in alcoholic patients. Transpl Int. 2005; 18:491–498. PMID: 15819795.
Article11. Mackie J, Groves K, Hoyle A, et al. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl. 2001; 7:418–427. PMID: 11349262.
Article12. Lim JK, Keeffe EB. Liver transplantation for alcoholic liver disease: current concepts and length of sobriety. Liver Transpl. 2004; 10(10 Suppl 2):S31–S38. PMID: 15382288.
Article13. Burra P, Mioni D, Cecchetto A, et al. Histological features after liver transplantation in alcoholic cirrhotics. J Hepatol. 2001; 34:716–722. PMID: 11434618.
Article14. Cuadrado A, Fábrega E, Casafont F, et al. Alcohol recidivism impairs long-term patient survival after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2005; 11:420–426. PMID: 15776421.
Article15. Jauhar S, Talwalkar JA, Schneekloth T, et al. Analysis of factors that predict alcohol relapse following liver transplantation. Liver Transpl. 2004; 10:408–411. PMID: 15004769.
Article16. Perney P, Bismuth M, Sigaud H, et al. Are preoperative patterns of alcohol consumption predictive of relapse after liver transplantation for alcoholic liver disease? Transpl Int. 2005; 18:1292–1297. PMID: 16221161.
Article17. Miguet M, Monnet E, Vanlemmens C, et al. Predictive factors of alcohol relapse after orthotopic liver transplantation for alcoholic liver disease. Gastroenterol Clin Biol. 2004; 28:845–851. PMID: 15523219.
Article18. Williams RS, Alisa AA, Karani JB, et al. Adult-to-adult living donor liver transplant: UK experience. Eur J Gastroenterol Hepatol. 2003; 15:7–14. PMID: 12544688.19. Testa G, Malagó M, Nadalin S, et al. Right-liver living donor transplantation for decompensated end-stage liver disease. Liver Transpl. 2002; 8:340–346. PMID: 11965577.
Article20. Kasahara M, Takada Y, Fujimoto Y, et al. Impact of right lobe with middle hepatic vein graft in living-donor liver transplantation. Am J Transplant. 2005; 5:1339–1346. PMID: 15888039.
Article21. Berlakovich GA, Windhager T, Freundorfer E, et al. Carbohydrate deficient transferrin for detection of alcohol relapse after orthotopic liver transplantation for alcoholic cirrhosis. Transplantation. 1999; 67:1231–1235. PMID: 10342314.
Article22. Markowitz JS, Martin P, Conrad AJ, et al. Prophylaxis against hepatitis B recurrence following liver transplantation using combination lamivudine and hepatitis B immune globulin. Hepatology. 1998; 28:585–589. PMID: 9696028.
Article23. Takemura N, Sugawara Y, Tamura S, et al. Liver transplantation using hepatitis B core antibody-positive grafts: review and university of Tokyo experience. Dig Dis Sci. 2007; 52:2472–2477. PMID: 17805972.
Article24. Prakoso E, Strasser SI, Koorey DJ, et al. Long-term lamivudine monotherapy prevents development of hepatitis B virus infection in hepatitis B surface-antigen negative liver transplant recipients from hepatitis B core-antibody-positive donors. Clin Transplant. 2006; 20:369–373. PMID: 16824156.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Deceased Donor Liver Transplantation for Alcoholic Liver Disease in Korea in MELD Era
- Liver retransplantation for adult recipients
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Pediatric liver transplantation in Korea: long-term outcomes and allocations