Korean J Crit Care Med.
2014 Nov;29(4):331-335. 10.4266/kjccm.2014.29.4.331.
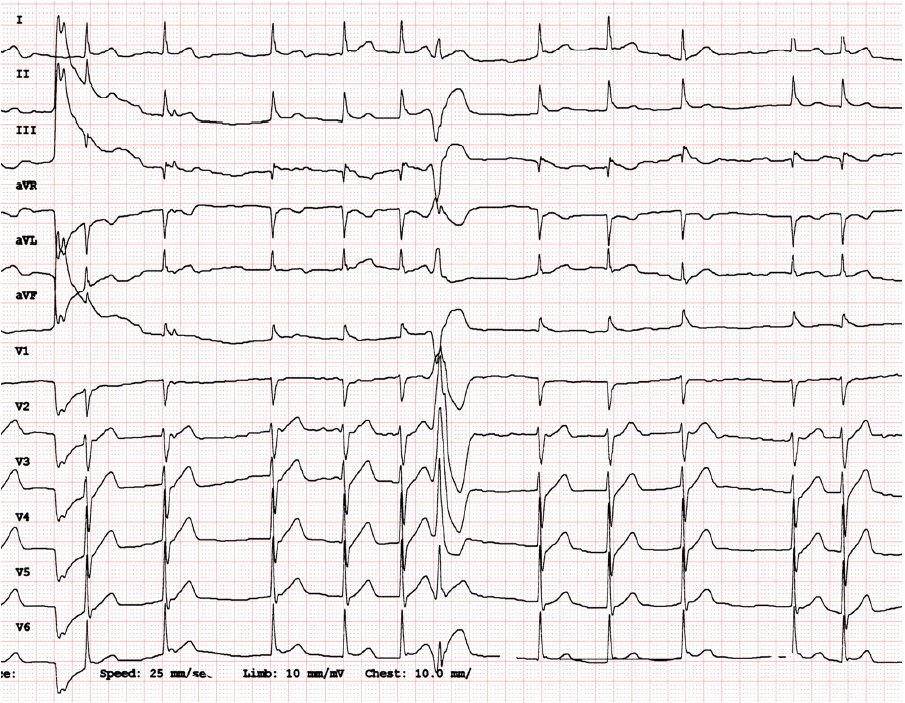
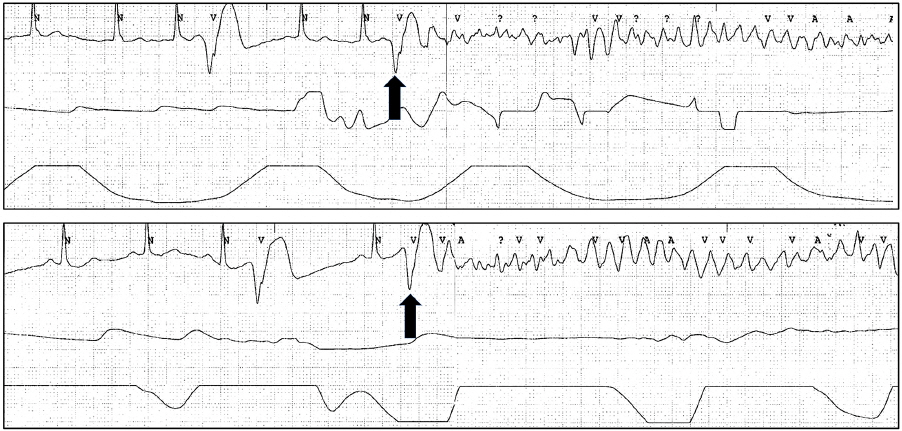
Cardiac Arrest due to Recurrent Ventricular Fibrillation Triggered by Unifocal Ventricular Premature Complexes in a Silent Myocardial Infarction
- Affiliations
-
- 1Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea. thinkmed@dau.ac.kr
- KMID: 2227742
- DOI: http://doi.org/10.4266/kjccm.2014.29.4.331
Abstract
- A 51-year-old male patient was referred for a sudden out-of-hospital cardiac arrest. Upon arrival, he was conscious and had no chest pain complaints. There was no abnormality in initial electrocardiographic and echocardiographic examinations. However, episodes of recurrent ventricular fibrillation (VF) were documented on rhythm monitoring. Each VF episode was triggered by an isolated monomorphic ventricular premature complex (VPC). Suspecting idiopathic VF, emergency radiofrequency catheter ablation was planned for the VPCs. However, when coronary angiography was performed to exclude silent ischemia, the results showed a total occlusion of the right coronary artery posterolateral branch, which is thought to supply the left ventricular inferior and septal wall. After successful reperfusion, VF episodes and the triggering VPCs disappeared. We are documenting this case to emphasize the potential for silent myocardial infarction to cause out-of-hospital sudden cardiac arrest even in a patient without any symptom or sign of acute coronary syndrome.
Keyword
MeSH Terms
-
Acute Coronary Syndrome
Catheter Ablation
Chest Pain
Coronary Angiography
Coronary Vessels
Death, Sudden, Cardiac
Echocardiography
Electrocardiography
Emergencies
Heart Arrest*
Humans
Ischemia
Male
Middle Aged
Myocardial Infarction*
Out-of-Hospital Cardiac Arrest
Reperfusion
Ventricular Fibrillation*
Ventricular Premature Complexes*
Figure
Reference
-
References
1). Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998; 98:2334–51.
Article2). O'Connor RE, Bossaert L, Arntz HR, Brooks SC, Diercks D, Feitosa-Filho G, et al. Part 9: Acute coronary syndromes: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010; 122(16 suppl 2):S422–65.3). Haissaguerre M, Shoda M, Jais P, Nogami A, Shah DC, Kautzner J, et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002; 106:962–7.
Article4). Tilz RR, Lin T, Makimoto H, Ouyang F. Successful epicardial ablation of electrical storms due to recurrent ventricular fibrillation triggered by premature ventricular contractions. Heart Rhythm. 2014; 11:146–9.
Article5). Cho YR, Park JS. Radiofrequency catheter ablation for unifocal premature ventricular complexes triggering recurrent ventricular fibrillations in a young man without structural heart disease. Korean Circ J. 2012; 42:575–9.
Article6). Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006; 114:e385–484.
Article7). Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia: a theoretical study of altered cell excitability and action potential duration. Cardiovasc Res. 1997; 35:256–72.
Article8). Little RA, Frayn KN, Randall PE, Stoner HB, Morton C, Yates DW, et al. Plasma catecholamines in the acute phase of the response to myocardial infarction. Arch Emerg Med. 1986; 3:20–7.
Article9). Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia. A mechanistic investigation of action potential conduction and conduction failure. Circ Res. 1997; 80:124–38.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Catheter Ablation for Unifocal Premature Ventricular Complexes Triggering Recurrent Ventricular Fibrillations in a Young Man Without Structural Heart Disease
- Ventricular premature complexes and associated factors in the early postinfarction period
- Observations of Arrhythmias by 24 Hour Ambulatory ECG Monitoring in Early Convalescent Phase of Acute Myocardial Infarction
- Catheter Ablation for Brugada Syndrome
- Management of Common Arrhythmia in the Neurological Intensive Care Unit