Korean Circ J.
2012 Aug;42(8):575-579. 10.4070/kcj.2012.42.8.575.
Radiofrequency Catheter Ablation for Unifocal Premature Ventricular Complexes Triggering Recurrent Ventricular Fibrillations in a Young Man Without Structural Heart Disease
- Affiliations
-
- 1Cardiovascular Center, Dong-A University Hospital, Busan, Korea. thinkmed@dau.ac.kr
- KMID: 2225011
- DOI: http://doi.org/10.4070/kcj.2012.42.8.575
Abstract
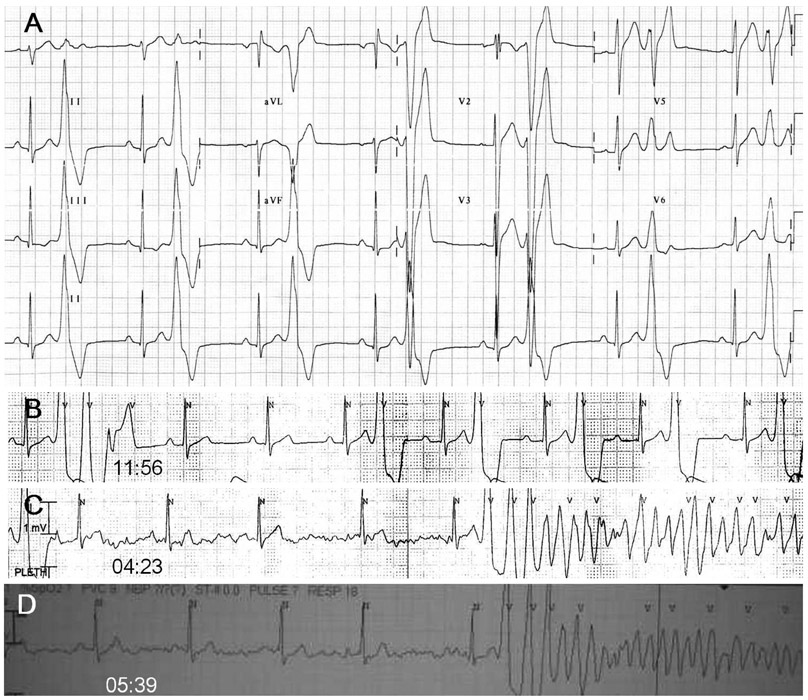
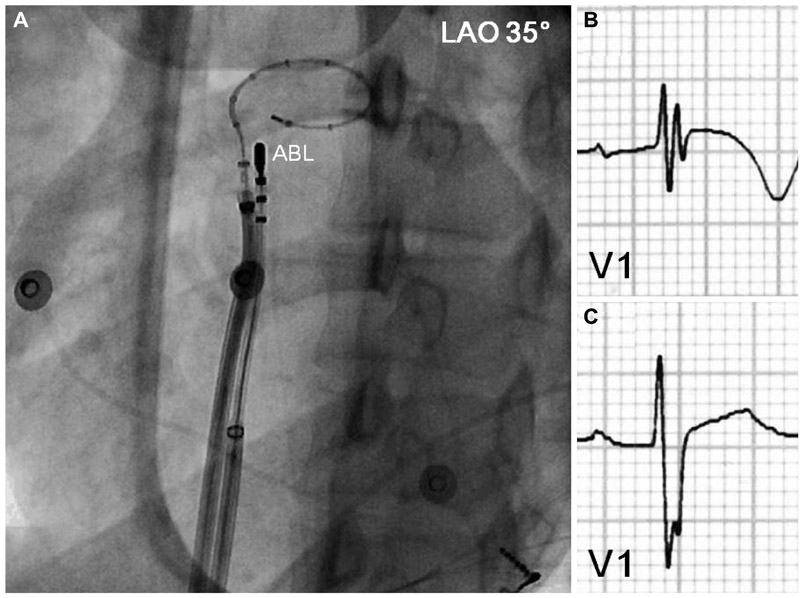
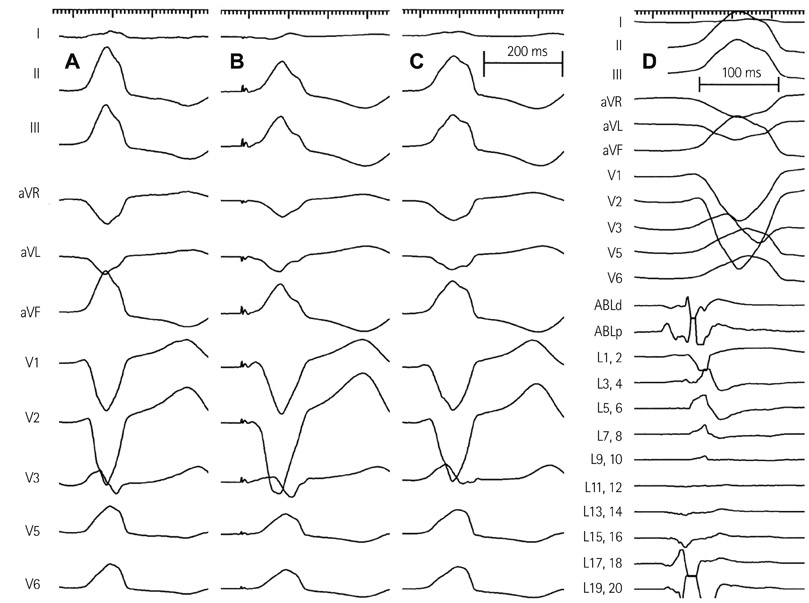
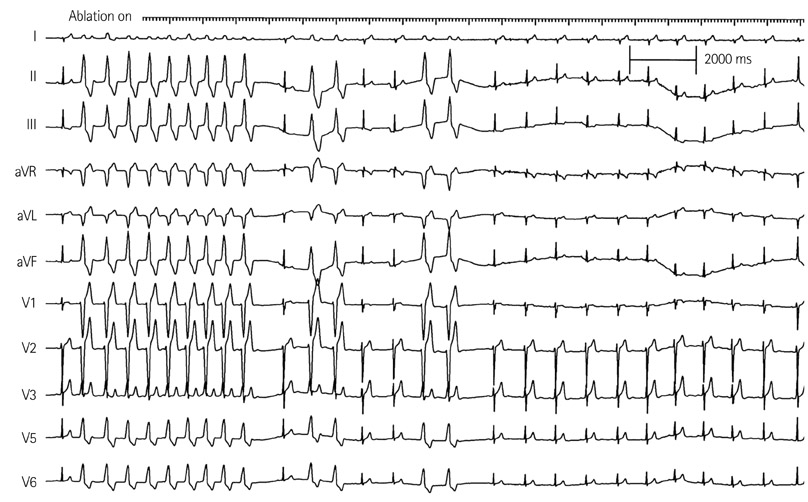
- A 17-year-old man was referred for aborted sudden cardiac death. Ventricular fibrillation (VF) was recorded by automated external defibrillator. Post-resuscitation electrocardiograms showed frequent monomorphic premature ventricular complexes (PVCs), with left bundle branch block configuration and inferior axis. Cardiac arrest due to VF recurred twice within the initial 42 hours. Rhythm monitoring revealed multiple episodes of sustained VF triggered by a triplet of monomorphic PVCs having similar morphology with isolated PVCs. Comprehensive cardiologic workup revealed no structural heart disease and ion-channelopathies. With the impression of idiopathic VF triggered by unifocal PVCs of right ventricular outflow tract (RVOT) origin, radiofrequency catheter ablation was performed to prevent frequent VF recurrence before implantable cardioverter-defibrillator (ICD) implantation. After successful ablation of the origin of unifocal PVCs at anterolateral wall of RVOT, the burden of PVCs decreased remarkably and VF did not recur. The patient was discharged after ICD implantation.
MeSH Terms
Figure
Cited by 1 articles
-
Cardiac Arrest due to Recurrent Ventricular Fibrillation Triggered by Unifocal Ventricular Premature Complexes in a Silent Myocardial Infarction
Dong Hyun Lee, Seul Lee, Hyo Jin Jung, Soo Jin Kim, Jeong-Min Seo, Jae-Hyuk Choi, Jong Sung Park
Korean J Crit Care Med. 2014;29(4):331-335. doi: 10.4266/kjccm.2014.29.4.331.
Reference
-
1. Survivors of out-of-hospital cardiac arrest with apparently normal heart: need for definition and standardized clinical evaluation: consensus Statement of the Joint Steering Committees of the Unexplained Cardiac Arrest Registry of Europe and of the Idiopathic Ventricular Fibrillation Registry of the United States. Circulation. 1997. 95:265–272.2. Haïssaguerre M, Shoda M, Jaïs P, et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002. 106:962–967.3. Uemura T, Yamabe H, Tanaka Y, et al. Catheter ablation of a polymorphic ventricular tachycardia inducing monofocal premature ventricular complex. Intern Med. 2008. 47:1799–1802.4. Nogami A, Sugiyasu A, Kubota S, Kato K. Mapping and ablation of idiopathic ventricular fibrillation from the Purkinje system. Heart Rhythm. 2005. 2:646–649.5. Buxton AE, Waxman HL, Marchlinski FE, Simson MB, Cassidy D, Josephson ME. Right ventricular tachycardia: clinical and electrophysiologic characteristics. Circulation. 1983. 68:917–927.6. Noda T, Shimizu W, Taguchi A, et al. Malignant entity of idiopathic ventricular fibrillation and polymorphic ventricular tachycardia initiated by premature extrasystoles originating from the right ventricular outflow tract. J Am Coll Cardiol. 2005. 46:1288–1294.7. Knecht S, Sacher F, Wright M, et al. Long-term follow-up of idiopathic ventricular fibrillation ablation: a multicenter study. J Am Coll Cardiol. 2009. 54:522–528.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Ablation of Recurrent Ventricular Premature Complex Originating from near Left Ventricular Summit Guided by Intracardiac Echocardiography
- Catheter Ablation for Brugada Syndrome
- Catheter Ablation of Parahisian Premature Ventricular Complex
- Radiofrequency Catheter Ablation of Ventricular Tachycardia in Patients without Structural Heart Disease
- Tachycardiomyopathy Induced by Ventricular Premature Complexes: Complete Recovery after Radiofrequency Catheter Ablation