Korean Circ J.
2020 Apr;50(4):289-301. 10.4070/kcj.2019.0344.
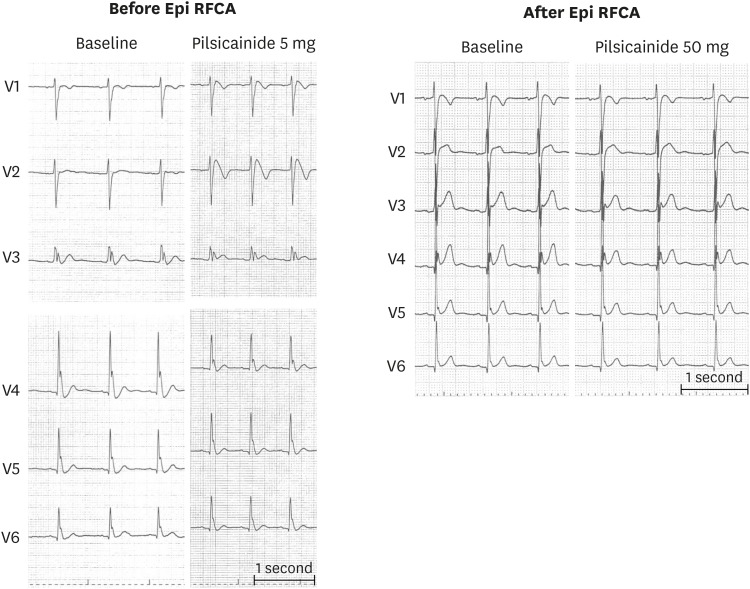
Catheter Ablation for Brugada Syndrome
- Affiliations
-
- 1Department of Cardiology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan. anogami@md.tsukuba.ac.jp
- 2Division of Cardiac Electrophysiology, Al Najaf Center for Cardiac Surgery and Trans-Catheter Therapy, Najaf, Iraq.
- KMID: 2471279
- DOI: http://doi.org/10.4070/kcj.2019.0344
Abstract
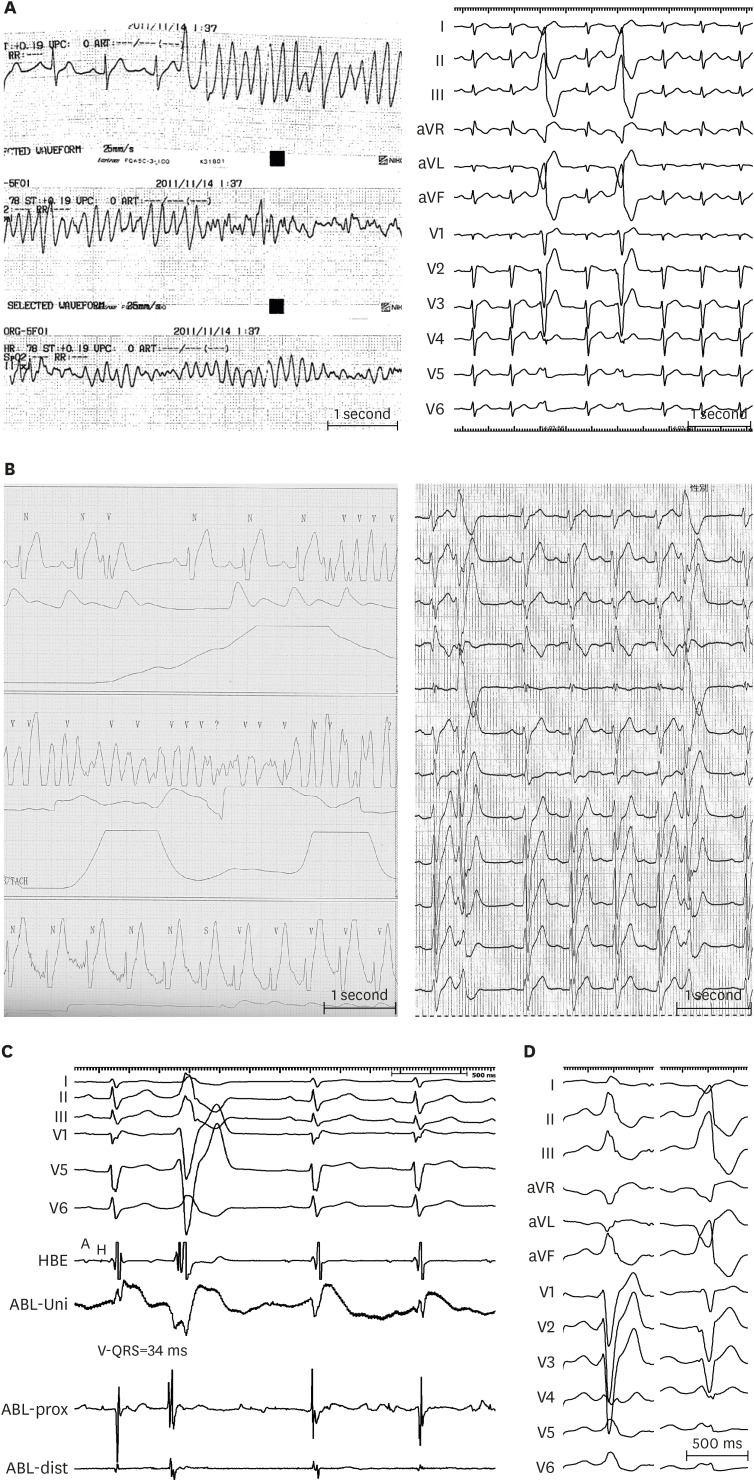
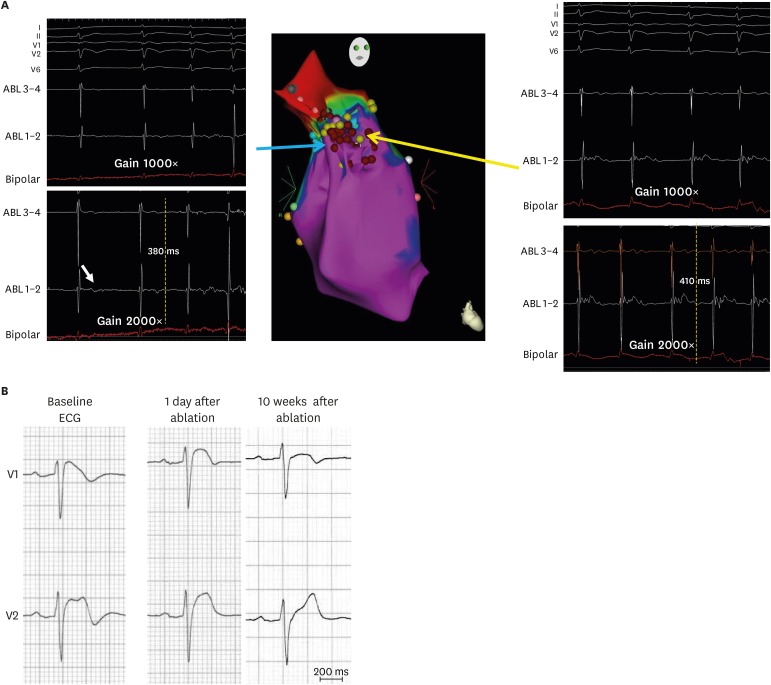
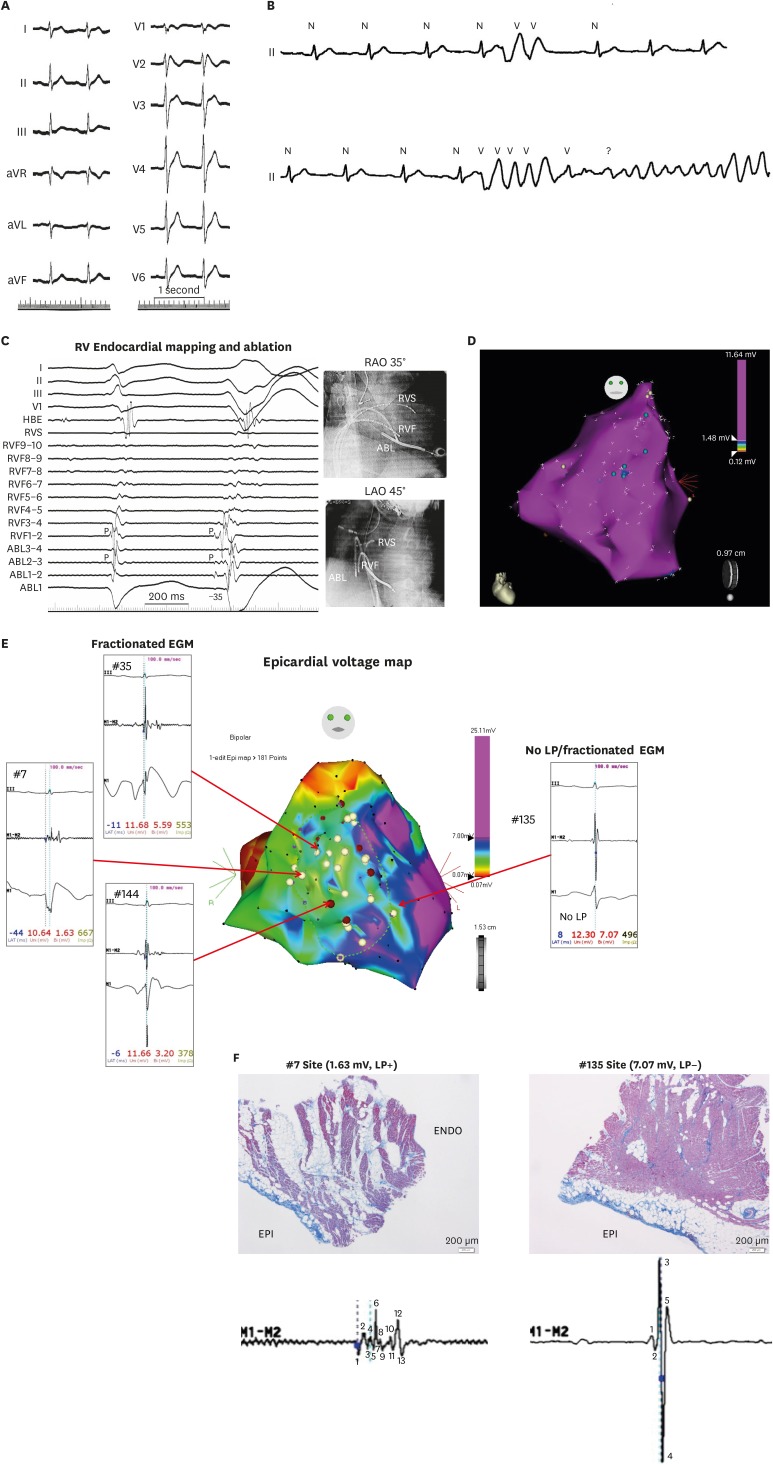
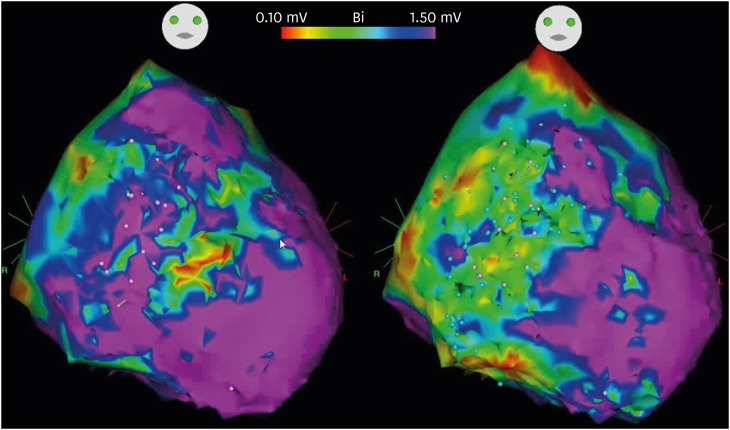
- Brugada syndrome (BrS) is an arrhythmogenic disease associated with an increased risk of ventricular fibrillation (VF) and sudden cardiac death (SCD). To date, the standard therapy for the prevention of SCD in BrS is the use of an implantable cardioverter-defibrillator (ICD) especially in patients who have experienced a prior cardiac arrest or syncopal events secondary to VF. However, ICDs do not prevent the occurrence of VF but react to defibrillate the VF episode, thereby preventing SCD. Often patients with recurrent VF have to be maintained on antiarrhythmic drugs that are effective but have remarkable adverse effects. An alternative therapy for BrS with recurrent VF is catheter ablation which emerged as an effective therapy in eliminating VF-triggering premature ventricular complexes in limited case series; however, there has been a remarkable progress in effectiveness of catheter ablation since epicardial substrate ablation was first applied in 2011 and such approach is now widely applicable.
MeSH Terms
Figure
Cited by 1 articles
-
Can Artemisinin Be a Game Changer Even as an Antiarrhythmic Drug?
Jongmin Hwang
Korean Circ J. 2023;53(4):251-253. doi: 10.4070/kcj.2023.0031.
Reference
-
1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396. PMID: 1309182.2. Hermida JS, Lemoine JL, Aoun FB, Jarry G, Rey JL, Quiret JC. Prevalence of the Brugada syndrome in an apparently healthy population. Am J Cardiol. 2000; 86:91–94. PMID: 10867101.3. Furuhashi M, Uno K, Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001; 86:161–166. PMID: 11454832.4. Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015; 36:2793–2867. PMID: 26320108.5. Belhassen B, Glick A, Viskin S. Efficacy of quinidine in high-risk patients with Brugada syndrome. Circulation. 2004; 110:1731–1737. PMID: 15381640.6. Viskin S, Wilde AA, Guevara-Valdivia ME, et al. Quinidine, a life-saving medication for Brugada syndrome, is inaccessible in many countries. J Am Coll Cardiol. 2013; 61:2383–2387. PMID: 23583244.7. Haïssaguerre M, Extramiana F, Hocini M, et al. Mapping and ablation of ventricular fibrillation associated with long-QT and Brugada syndromes. Circulation. 2003; 108:925–928. PMID: 12925452.8. Nademanee K, Veerakul G, Chandanamattha P, et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011; 123:1270–1279. PMID: 21403098.9. Kakishita M, Kurita T, Matsuo K, et al. Mode of onset of ventricular fibrillation in patients with Brugada syndrome detected by implantable cardioverter defibrillator therapy. J Am Coll Cardiol. 2000; 36:1646–1653. PMID: 11079671.10. Morita H, Fukushima-Kusano K, Nagase S, et al. Site-specific arrhythmogenesis in patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2003; 14:373–379. PMID: 12741708.11. Nademanee K, Raju H, de Noronha SV, et al. Fibrosis, connexin-43, and conduction abnormalities in the Brugada syndrome. J Am Coll Cardiol. 2015; 66:1976–1986. PMID: 26516000.12. Coronel R, Casini S, Koopmann TT, et al. Right ventricular fibrosis and conduction delay in a patient with clinical signs of Brugada syndrome: a combined electrophysiological, genetic, histopathologic, and computational study. Circulation. 2005; 112:2769–2777. PMID: 16267250.13. Darmon JP, Bettouche S, Deswardt P, et al. Radiofrequency ablation of ventricular fibrillation and multiple right and left atrial tachycardia in a patient with Brugada syndrome. J Interv Card Electrophysiol. 2004; 11:205–209. PMID: 15548887.14. Nakagawa E, Takagi M, Tatsumi H, Yoshiyama M. Successful radiofrequency catheter ablation for electrical storm of ventricular fibrillation in a patient with Brugada syndrome. Circ J. 2008; 72:1025–1029. PMID: 18503235.15. Talib AK, Takagi M, Shimane A, et al. Efficacy of endocardial ablation of drug-resistant ventricular fibrillation in Brugada syndrome: long-term outcome. Circ Arrhythm Electrophysiol. 2018; 11:e006675. PMID: 30354324.16. Krittayaphong R, Veerakul G, Nademanee K, Kangkagate C. Heart rate variability in patients with Brugada syndrome in Thailand. Eur Heart J. 2003; 24:1771–1778. PMID: 14522573.17. Talib AK, Yui Y, Kaneshiro T, Sekiguchi Y, Nogami A, Aonuma K. Alternative approach for management of an electrical storm in Brugada syndrome: importance of primary ablation within a narrow time window. J Arrhythm. 2016; 32:220–222. PMID: 27354869.18. Shah AJ, Hocini M, Lamaison D, Sacher F, Derval N, Haissaguerre M. Regional substrate ablation abolishes Brugada syndrome. J Cardiovasc Electrophysiol. 2011; 22:1290–1291. PMID: 21457386.19. Sunsaneewitayakul B, Yao Y, Thamaree S, Zhang S. Endocardial mapping and catheter ablation for ventricular fibrillation prevention in Brugada syndrome. J Cardiovasc Electrophysiol. 2012; 23(Suppl 1):S10–S16. PMID: 22988965.20. Hayashi T, Nitta J, Goya M, Isobe M, Hirao K. Endocardial-only catheter ablation with substantial improvement in ventricular fibrillation recurrences in a patient with Brugada syndrome. HeartRhythm Case Rep. 2016; 2:428–431. PMID: 28491726.21. Morita H, Zipes DP, Morita ST, Lopshire JC, Wu J. Epicardial ablation eliminates ventricular arrhythmias in an experimental model of Brugada syndrome. Heart Rhythm. 2009; 6:665–671. PMID: 19328041.22. Brugada J, Pappone C, Berruezo A, et al. Brugada syndrome phenotype elimination by epicardial substrate ablation. Circ Arrhythm Electrophysiol. 2015; 8:1373–1381. PMID: 26291334.23. Pappone C, Brugada J, Vicedomini G, et al. Electrical substrate elimination in 135 consecutive patients with Brugada syndrome. Circ Arrhythm Electrophysiol. 2017; 10:e005053. PMID: 28500178.24. Sacher F, Jesel L, Jais P, Haïssaguerre M. Insight into the mechanism of Brugada syndrome: epicardial substrate and modification during ajmaline testing. Heart Rhythm. 2014; 11:732–734. PMID: 23732228.25. Chung FP, Raharjo SB, Lin YJ, et al. A novel method to enhance phenotype, epicardial functional substrates, and ventricular tachyarrhythmias in Brugada syndrome. Heart Rhythm. 2017; 14:508–517. PMID: 28065832.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Idiopathic Brugada ECG Pattern Developed in Relation To Fever
- Large Circular Ring Catheter Ablation Versus Anatomically Guided Ablation of Atrial Fibrillation: Back to the Future for Successful Catheter Ablation of Atrial Fibrillation?
- Anesthesia in a Patient with Brugada Syndrome without a Characteristic ECG Pattern: A case report
- COVID-19 Vaccination-Induced Ventricular Fibrillation in an Afebrile Patient With Brugada Syndrome
- Brugada Syndrome Presenting With Convulsion in the Emergency Department: A Case Report