J Korean Ophthalmol Soc.
2011 Jun;52(6):759-765. 10.3341/jkos.2011.52.6.759.
Traumatic Eyeball Protrusion with Optic Chiasmal Injury
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. changmh@dankook.ac.kr
- KMID: 2214652
- DOI: http://doi.org/10.3341/jkos.2011.52.6.759
Abstract
- PURPOSE
To report a case of eyeball protrusion with optic chiasmal injury due to eyeball trauma.
CASE SUMMARY
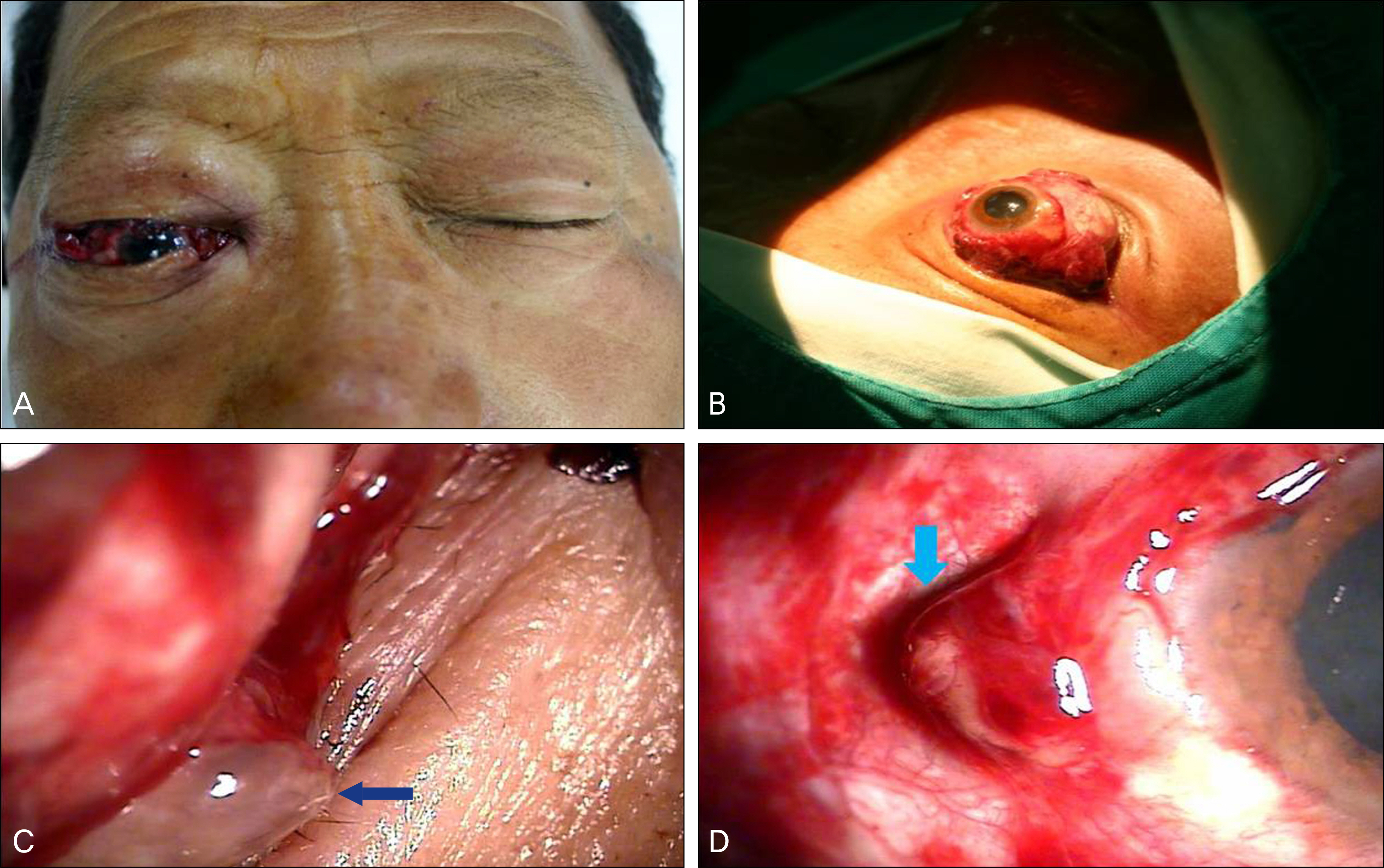
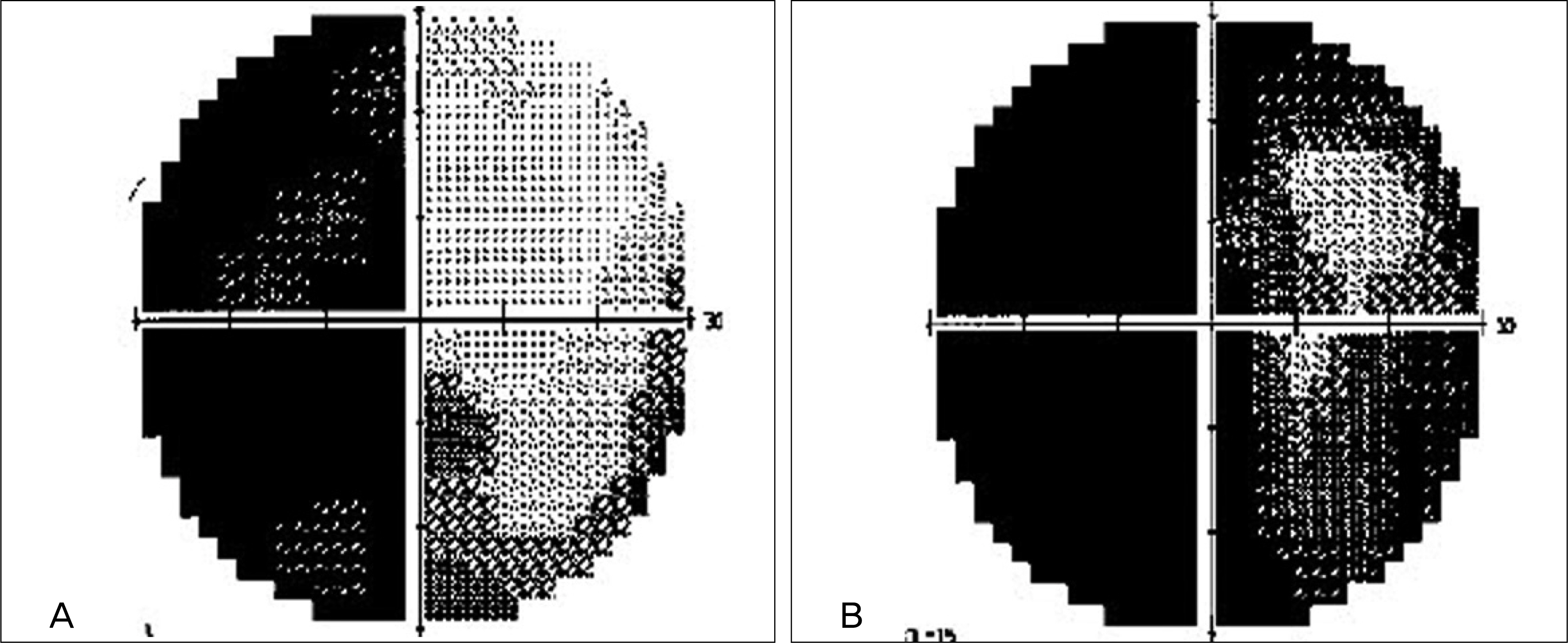
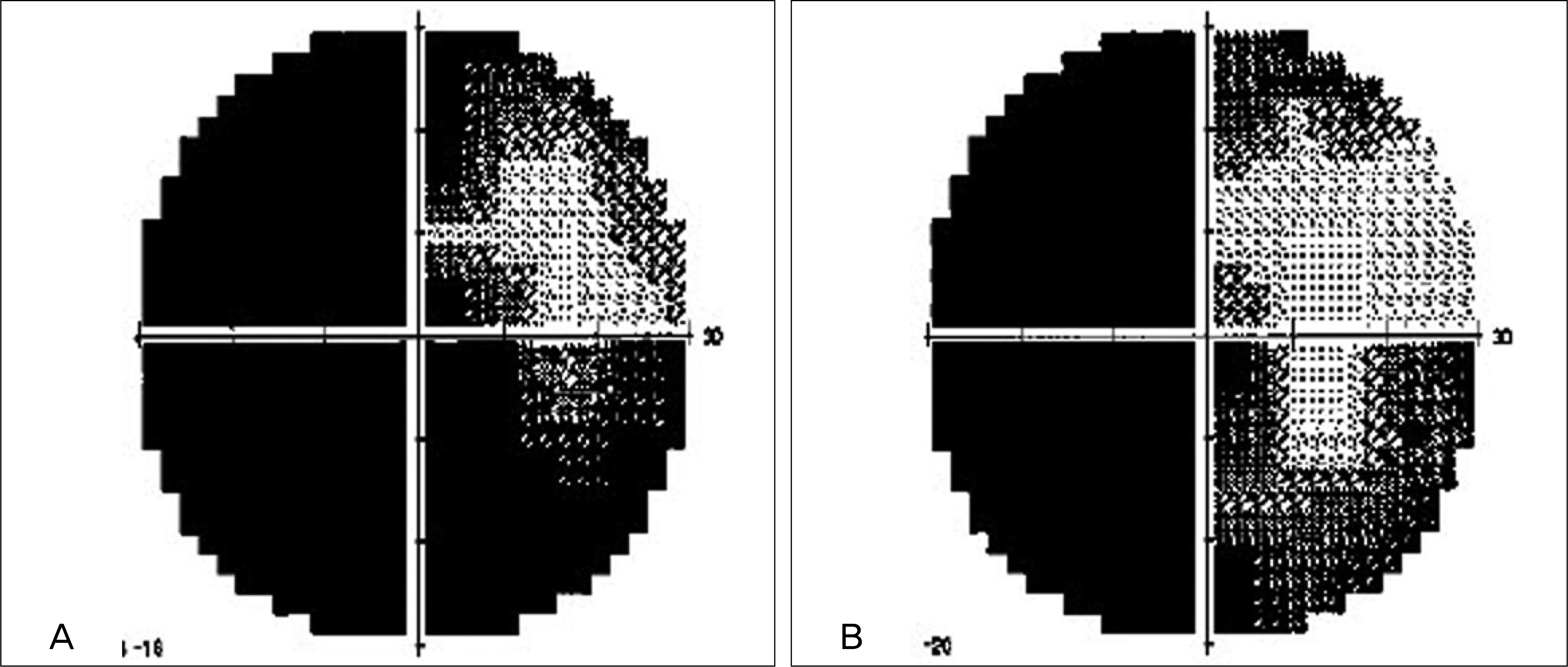
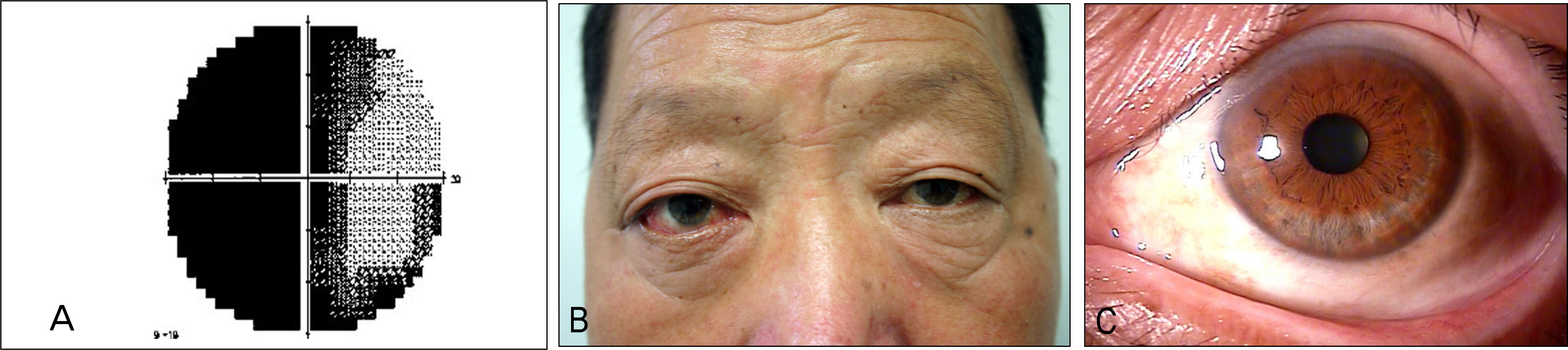
A 59-year-old male presented to the emergency room for right eyeball pain, eyeball protrusion and decreased visual acuity after collision with a metal pipe. On initial examination, the right eyeball was protruded, the patient could not perceive light, his pupil was dilated and did not respond to the light. The patient had a laceration of the lower canaliculi and the medial, superior and inferior rectus muscles were separated from the eyeball. Abnormal left pupil response was observed, and visual acuity of the left eye was 0.7. He underwent primary repair of the right medial, inferior and superior rectus muscles and reconstruction of the lower canaliculi. Because the visual field of the left eye at post-operative day 1 demonstrated temporal hemianopsia, an optic chiasmal injury was revealed on brain magnetic resonance imaging (MRI). The patient underwent left optic chiasmal decompression because the visual field was aggravated despite the immediate high dose of corticosteroid therapy. At post-operative 2 months, the patient's left visual acuity was 0.3 and the visual field was stable.
CONCLUSIONS
Optic chiasmal injury should be considered and promptly diagnosed through visual field test and MRI when ipsilateral optic nerve injury with abnormal contralateral pupil response is caused by eyeball protrusion. Optic chiasmal decompression should be considered when traumatic optic nerve and chiasmal injuries do not respond to high-dose corticosteroid therapy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Habal MB. Clinical observations on the isolated optic nerve injury. Ann Plast Surg. 1978; 1:603–7.
Article2. Dul MW. Optic nerve trauma. Optom Clin. 1993; 3:91–101.3. Rosenberg PN, Stasior OB. Optic nerve evulsion and transection. Adv Ophthalmic Plast Reconstr Surg. 1987; 6:63–9.4. Kim SH, Paik SH, Lee TS. Treatment of complete traumatic eye-ball extrusion. J Korean Ophthalmol Soc. 1995; 36:2271–5.5. Huh JS, Chun DH, Kim BJ, Lee HB. A case of traumatic eyeball extrusion with complex, comminuted fractures. J Korean Ophthalmol Soc. 2003; 44:251–8.6. Steinsapir KD, Goldberg RA. Traumatic optic neuropathies. Miller NR, Newman NJ, editors. Walsh and Hoyt's Clinical Neuroophthalmology. 5th ed.Baltimore: Williams and Wilkins;1998. 1:chap. 16.7. Wurdermann. Injuries of the Eye. 2nd ed.part I. St. Louis: CV Mosby;1962. p. 1–264.8. Song MH, Kim JW, Chung SK. The statistical observation of ocular injury. J Korean Ophthalmol Soc. 2009; 50:580–7.
Article9. Han YS, Shyn KH. A statistical observation of the ocular injuries. J Korean Ophthalmol Soc. 2005; 46:117–24.10. Laursen AB. Traumatic bitemporal hemianopsia. Survey of the literature and report of a case. Acta Ophthalmol. 1971; 49:134–42.11. Hassan A, Crompton JL, Sandhu A. Traumatic chiasmal syndrome: a series of 19 patients. Clin Experiment Ophthalmol. 2002; 30:273–80.
Article12. De Nunzio M, McAuliffe W, Chakera TM. Magnetic resonance imaging of traumatic transection of the optic chiasm. Australas Radiol. 1997; 41:155–6.
Article13. Savino PJ, Glaser JS, Schatz NJ. Traumatic chiasmal syndrome. Neurology. 1980; 30:963–70.
Article14. Heinz GW, Nunery WR, Grossman CB. Traumatic chiasmal syndrome associated with midline basilar skull fractures. Am J Ophthalmol. 1994; 117:90–6.
Article15. Schiefer U, Isbert M, Mikolaschek E, et al. Distribution of scotoma pattern related to chiasmal lesions with special reference to anterior junction syndrome. Graefes Arch Clin Exp Ophthalmol. 2004; 242:468–77.
Article16. Blamires TL, Reeves BC. Vision defects in patients with peri-chiasmal lesions. Optometry and vision science. 1996; 73:572–8.
Article17. Hirai T, Ito Y, Arai M, et al. Loss of stereopsis with optic chiasmal lesions and stereoscopic tests as a differential test. Ophthalmology. 2002; 109:1692–702.
Article18. Shin MC, Ha JK, Oh JS. Optic nerve evulsion: 1 case report. J Korean Ophthalmol Soc. 1998; 39:800–4.19. Morris WR, Osborn FD, Fleming JC. Traumatic evulsion of the globe. Ophthal Plast Reconstr Surg. 2002; 18:261–7.
Article20. Anderson RL, Panje WR, Gross CE. Optic nerve blindness following blunt forehead trauma. Ophthalmology. 1982; 89:445–55.
Article21. Seiff SR. High dose corticosteroids for treatment of vision loss due to indirect injury to the optic nerve. Ophthalmic Surg. 1990; 21:389–95.
Article22. Lam BL, Weingeist TA. Corticosteroid-responsive traumatic optic neuropathy. Am J Ophthalmol. 1990; 109:99–101.23. Spoor TC, Hartel WC, Lensink DB, Wilkinson MJ. Treatment of traumatic optic neuropathy with corticosteroids. Am J Ophthalmol. 1990; 110:665–9.
Article24. Guy J, Sherwood M, Day AL. Surgical treatment of progressive visual loss in traumatic optic neuropathy. Report of two cases. J Neurosurg. 1989; 70:799–801.25. Bedrossian RH. Emergency orbital decompression. Ophthalmic Surg. 1985; 16:293–5.
Article26. Osguthorpe JD, Sofferman RA. Optic nerve decompression. Otolaryngol Clin North Am. 1988; 21:155–69.27. Levin LA, Beck RW, Joseph MP, et al. The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma Study. Ophthalmology. 1999; 106:1268–77.28. Lessell S. Indirect optic nerve trauma. Arch Ophthalmol. 1989; 107:382–6.
Article29. Lee AG. Traumatic optic neuropathy. Ophthalmology. 2000; 107:814.
Article30. Chung IY, Park JM, Yoo JM. High dose steroid and optic canal decompression in the treatment of traumatic optic neuropathy. J Korean Ophthalmol Soc. 2000; 41:1210–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of suspected arteriosclerotic optical chiasmal syndrome
- A Case of Traumatic Eyeball Extrusion
- Penetrating Injury of Optic Chiasm after Head Injury
- A Case of Optic chiasmal and focal hypothalamic infarction
- Assessment of Visual Outcome Following Optic Canal Decompression in Traumatic Optic Nerve Injuries