J Korean Ophthalmol Soc.
2011 Jun;52(6):679-689. 10.3341/jkos.2011.52.6.679.
Long-term Clinical Outcomes of Femtosecond LASER-Assisted Descemet's Stripping Endothelial Keratoplasty
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hwtchah@amc.seoul.kr
- KMID: 2214639
- DOI: http://doi.org/10.3341/jkos.2011.52.6.679
Abstract
- PURPOSE
To evaluate the long-term clinical outcomes of femtosecond LASER-assisted Descemet's stripping endothelial keratoplasty (DSEK).
METHODS
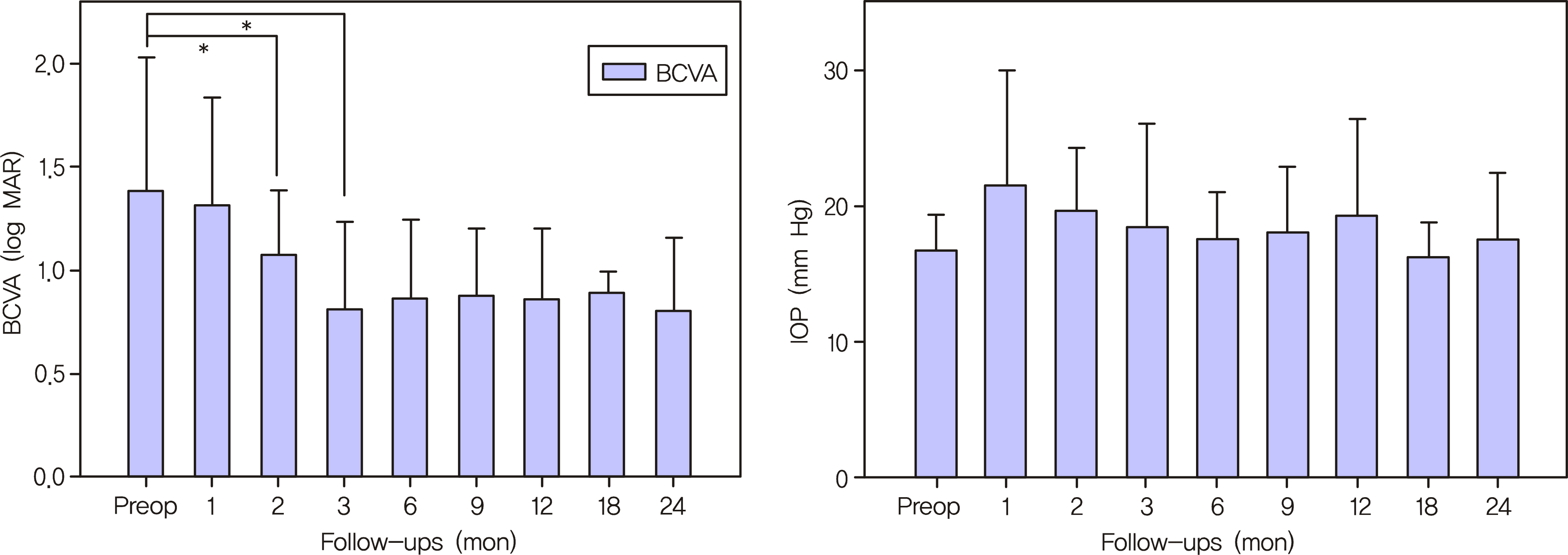
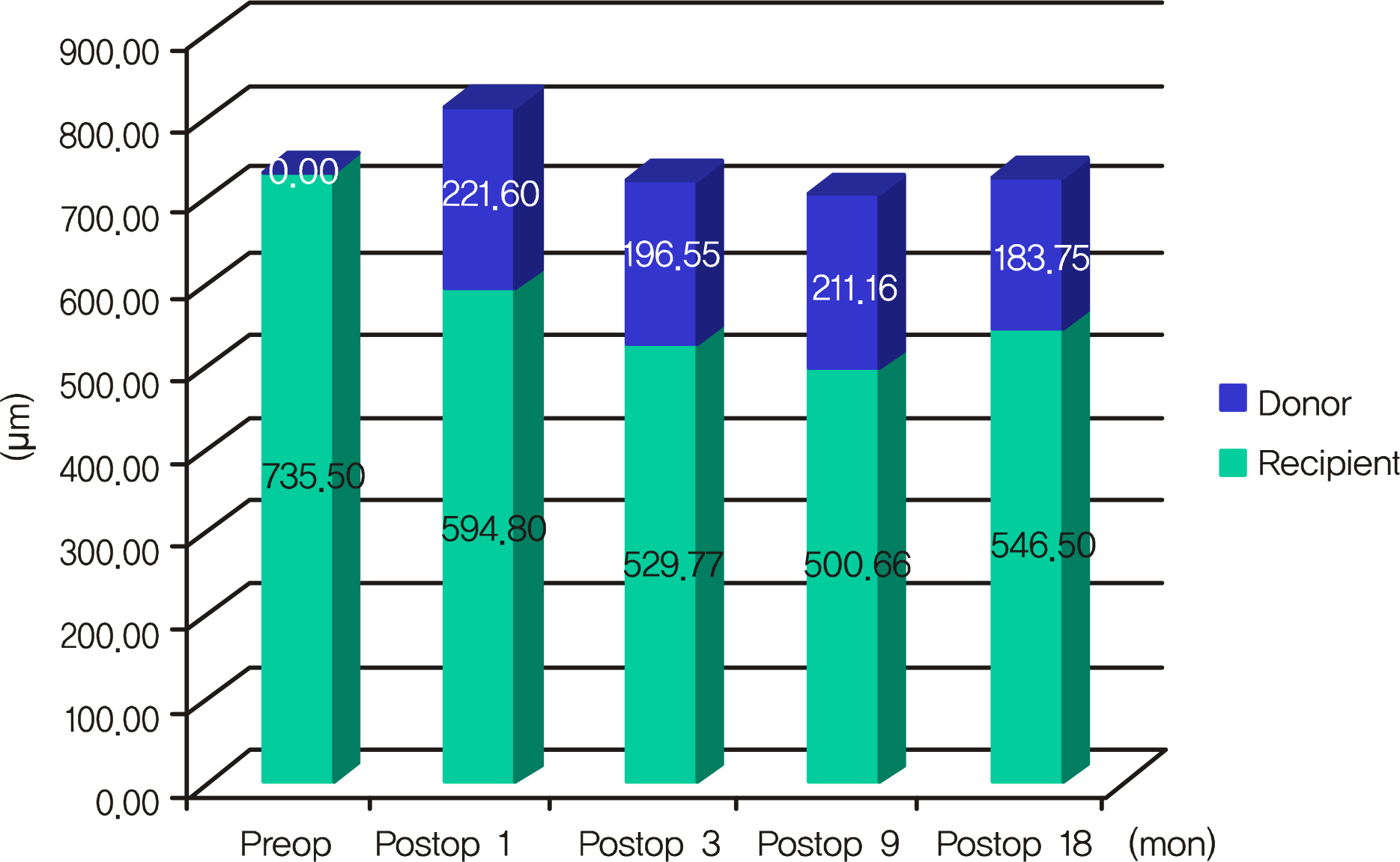
The clinical results of endothelial keratopathy from 11 consecutive patients who were followed up for at least 12 months after femtosecond LASER-assisted DSEK were retrospectively analyzed. The best corrected visual acuities (BCVA), manifest refractions, intraocular pressures, and perioperative complications were evaluated preoperatively and up to 24 months after the femtosecond LASER-assisted DSEK.
RESULTS
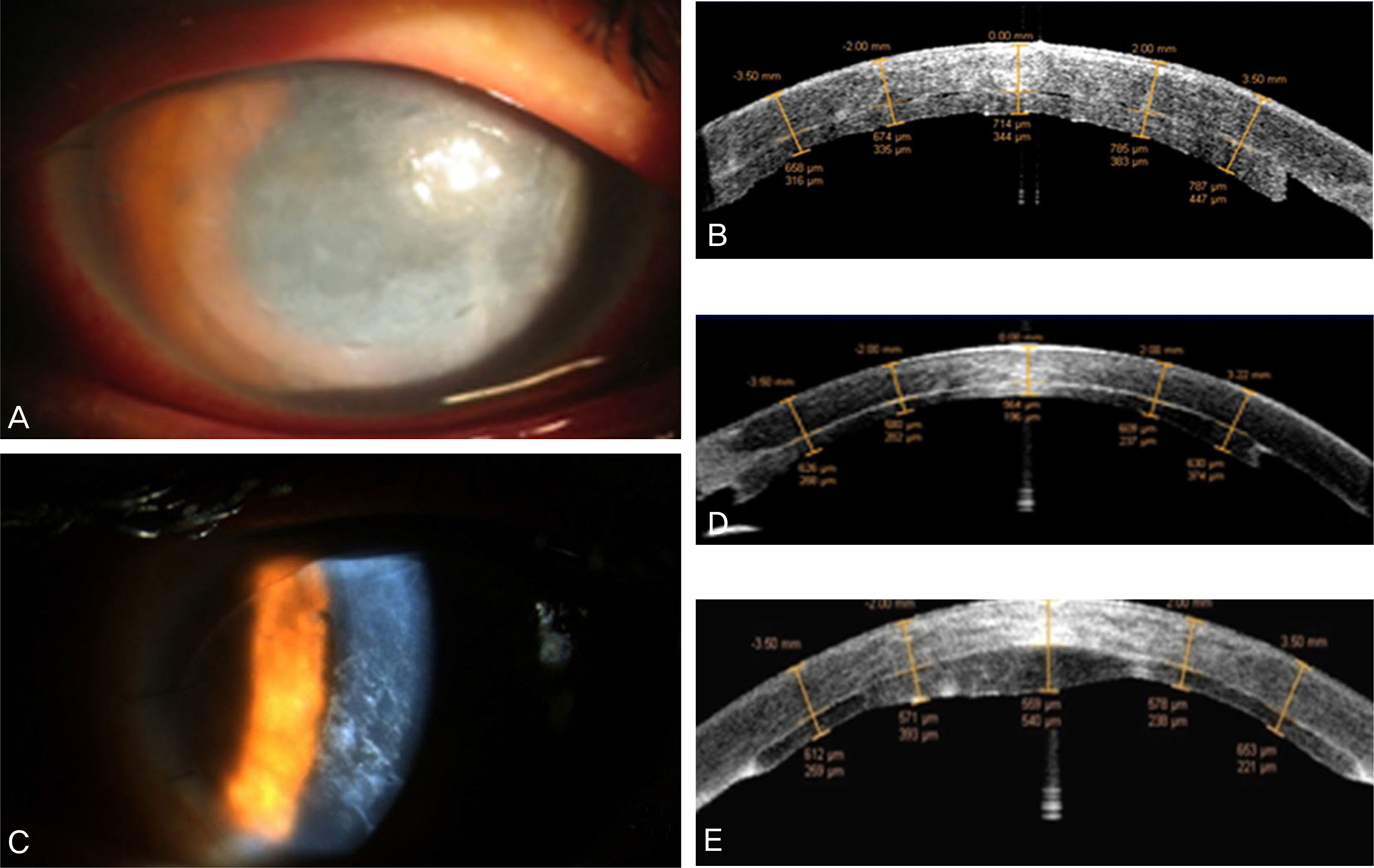
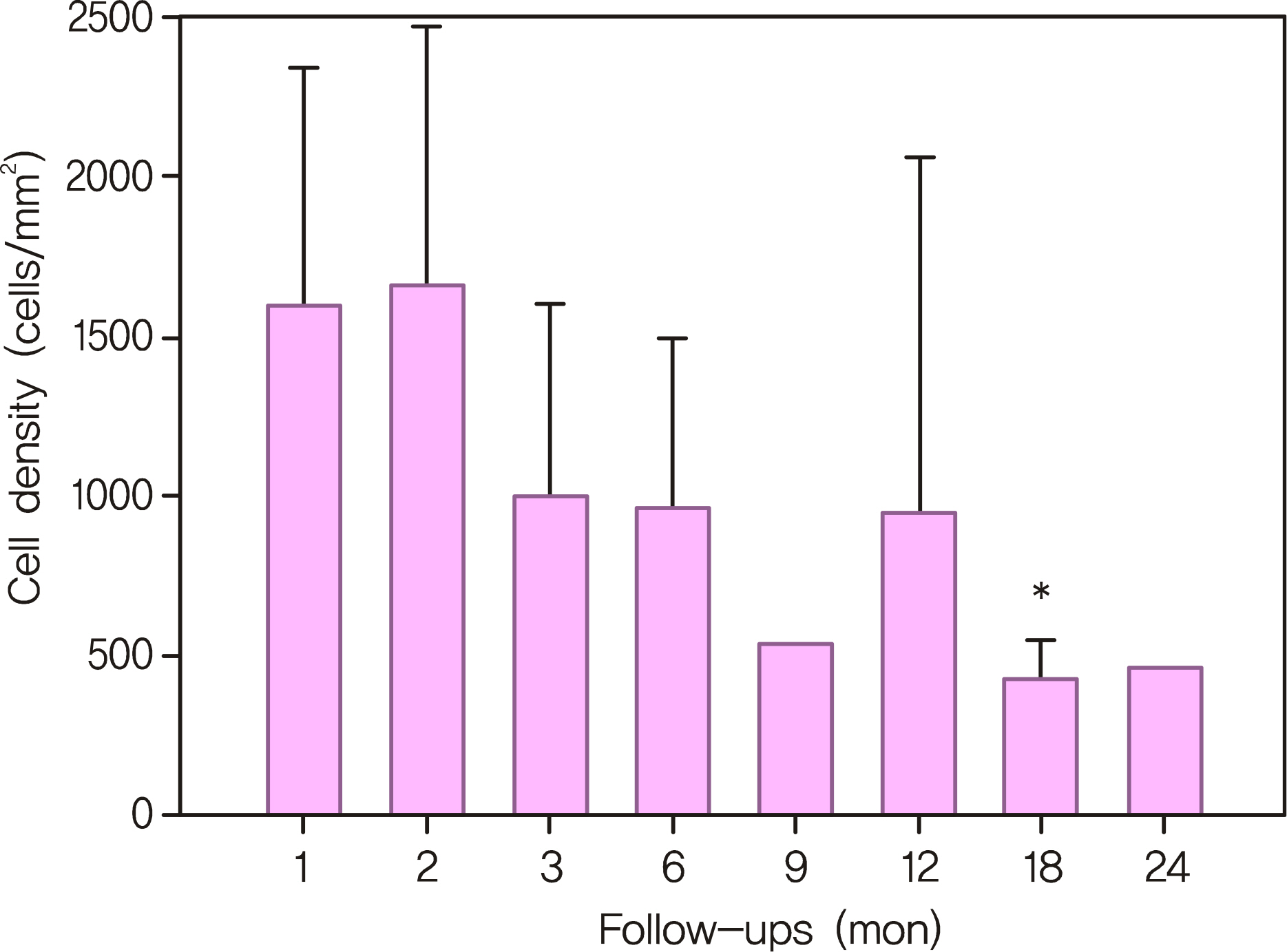
The average follow-up period was 18 months. Postoperative visual acuity had significantly improved from 1.26 (logMAR) to 0.80 (logMAR) at 3 months (p < 0.05) and this change was maintained during postoperative follow-up. All eyes underwent successful transplantation and the donor discs were well-attached. The mean endothelial cell density continued to decrease during the follow-up period. The donor-recipient stromal interface was the area where varying degree of haziness and birefringent particles were found.
CONCLUSIONS
The femtosecond LASER-assisted DSEK was effective in creating an endothelial donor disc which resulted in rapid visual recovery and low surgically-induced astigmatism. However, the operation caused rapid decrease in endothelial cell density which requires continuing further consideration by the physician.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparing Clinical Outcomes of Descemet's Membrane Stripping Automated Endothelial Keratoplasty Between Graft Insertion Methods
Ji Won Baek, Kyu Yeon Hwang, Choun-Ki Joo
J Korean Ophthalmol Soc. 2013;54(11):1655-1662. doi: 10.3341/jkos.2013.54.11.1655.
Reference
-
References
1. Price FW Jr, Price MO. Descemet's stripping with endothelial keratoplasty in 200 eyes: Early challenges and techniques to enhance donor adherence. J Cataract Refract Surg. 2006; 32:411–8.2. Terry MA, Ousley PJ. Replacing the endothelium without corneal surface incisions or sutures: the first United States clinical series using the deep lamellar endothelial keratoplasty procedure. Ophthalmology. 2003; 110:755–64.3. Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty visual acuity, astigmatism, and endothelial survival in a large prospective series. Ophthalmology. 2005; 112:1541–8.4. Melles GR, Wijdh RH, Nieuwendaal CP. A technique to excise the descemet membrane from a recipient cornea (descemetorhexis). Cornea. 2004; 23:286–8.
Article5. Cheng YY, Pels E, Nuijts RM. Femtosecond-laser-assisted Descemet's stripping endothelial keratoplasty. J Cataract Refract Surg. 2007; 33:152–5.
Article6. Espana EM, Huang B. Confocal microscopy study of donor-recipient interface after Descemet's stripping with endothelial keratoplasty. Br J Ophthalmol. 2010; 94:903–8.
Article7. Price FW Jr, Price MO. Descemet's stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg. 2005; 21:339–45.
Article8. Seo WM, Kim HK. Early result of femtosecond laser assisted descemet's membrane stripping endothelial keratoplasty. J Korean Ophthalmol Soc. 2008; 49:40–7.
Article9. Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis: prospective contralateral eye study. J Cataract Refract Surg. 2005; 31:120–6.10. Cheng YY, Schouten JS, Tahzib NG, et al. Efficacy and safety of femtosecond laser-assisted corneal endothelial keratoplasty: a randomized multicenter clinical trial. Transplantation. 2009; 88:1294–302.
Article11. Cheng YY, Pels E, Cleutjens JP, et al. Corneal endothelial viability after femtosecond laser preparation of posterior lamellar discs for Descemet-stripping endothelial keratoplasty. Cornea. 2007; 26:1118–22.
Article12. Cheng YY, Kang SJ, Grossniklaus HE, et al. Histologic evaluation of human posterior lamellar discs for femtosecond laser Descemet's stripping endothelial keratoplasty. Cornea. 2009; 28:73–9.
Article13. Cheng YY, Hendrikse F, Pels E, et al. Preliminary results of femtosecond laser-assisted descemet stripping endothelial keratoplasty. Arch Ophthalmol. 2008; 126:1351–6.
Article14. Seitz B, Langenbucher A, Hofmann-Rummelt C, et al. Nonmechanical posterior lamellar keratoplasty using the femtosecond laser (femto- plak) for corneal endothelial decompensation. Am J Ophthalmol. 2003; 136:769–72.15. Lee DH, Chung TY, Chung ES, et al. Case report: Femtosecond laser-assisted small incision deep lamellar endothelial keratoplasty. Korean J Ophthalmol. 2008; 22:43–8.
Article16. Sarayba MA, Juhasz T, Chuck RS, et al. Femtosecond laser posterior lamellar keratoplasty: a laboratory model. Cornea. 2005; 24:328–33.17. Mehta JS, Shilbayeh R, Por YM, et al. Femtosecond laser creation of donor cornea buttons for Descemet-stripping endothelial keratoplasty. J Cataract Refract Surg. 2008; 34:1970–5.
Article18. Lee JS, Park YG, Yoon KC. Long-term results of Descemet's stripping automated endothelial keratoplasty in Korea. J Korean Ophthalmol Soc. 2010; 51:1431–7.
Article19. Pineros O, Cohen EJ, Rapuano CJ, Laibson PR. Long-term results after penetrating keratoplasty for Fuchs' endothelial dystrophy. Arch Ophthalmol. 1996; 114:15–8.
Article20. Kim KE, Joo CK. Changes in astigmatism after suture removal in penetrating keratoplasty. J Korean Ophthalmol Soc. 2003; 44:284–8.21. Ousley PJ, Terry MA. Stability of vision, topography, and endothelial cell density from 1 year to 2 years after deep lamellar endothelial keratoplasty surgery. Ophthalmology. 2005; 112:50–7.
Article22. Fogla R, Padmanabhan P. Initial results of small incision deep lamellar endothelial keratoplasty (DLEK). Am J Ophthalmol. 2006; 141:346–51.
Article23. Yepes N, Segev F, Hyams M, et al. Five-millimeter-incision deep lamellar endothelial keratoplasty: one-year results. Cornea. 2007; 26:530–3.24. Patel SV, Hodge DO, Bourne WM. Corneal endothelium and postoperative outcomes 15 years after penetrating keratoplasty. Am J Ophthalmol. 2005; 139:311–9.
Article25. Ing JJ, Ing HH, Nelson LR, et al. Ten-year postoperative results of penetrating keratoplasty. Ophthalmology. 1998; 105:1855–65.
Article26. Bahar I, Kaiserman I, McAllum P, et al. Comparison of posterior lamellar keratoplasty techniques to penetrating keratoplasty. Ophthalmology. 2008; 115:1525–33.
Article27. Mearza AA, Qureshi MA, Rostron CK. Experience and 12-month results of descemet-stripping endothelial keratoplasty (DSEK) with a small-incision technique. Cornea. 2007; 26:1292–3.
Article28. Koenig SB, Covert DJ, Dupps WJ Jr, Meisler DM. Visual acuity, refractive error, and endothelial cell density six months after Descemet stripping and automated endothelial keratoplasty (DSAEK). Cornea. 2007; 26:670–4.
Article29. Terry MA, Chen ES, Shamie N, et al. Endothelial cell loss after Descemet's stripping endothelial keratoplasty in a large prospective series. Ophthalmology. 2008; 115:488–96.
Article30. Price MO, Price FW Jr. Endothelial cell loss after descemet stripping with endothelial keratoplasty influencing factors and 2-year trend. Ophthalmology. 2008; 115:857–65.31. Flanagan GW, Binder PS. Precision of flap measurements for laser in situ keratomileusis in 4428 eyes. J Refract Surg. 2003; 19:113–23.
Article32. Thomas J, Wang J, Rollins AM, Sturm J. Comparison of corneal thickness measured with optical coherence tomography, ultrasonic pachymetry, and a scanning slit method. J Refract Surg. 2006; 22:671–8.
Article33. Thompson RW Jr, Choi DM, Price MO, et al. Noncontact optical coherence tomography for measurement of corneal flap and residual stromal bed thickness after laser in situ keratomileusis. J Refract Surg. 2003; 19:507–15.
Article34. Eisner RA, Binder PS. Technique for measuring laser in situ keratomileusis flap thickness using the IntraLase laser. J Cataract Refract Surg. 2006; 32:556–8.
Article35. Koenig SB, Covert DJ. Early results of small-incision Descemet's stripping and automated endothelial keratoplasty. Ophthalmology. 2007; 114:221–6.
Article36. Covert DJ, Koenig SB. New triple procedure: Descemet's stripping and automated endothelial keratoplasty combined with phacoe-mulsification and intraocular lens implantation. Ophthalmology. 2007; 114:1272–7.
Article37. Sonigo B, Iordanidou V, Chong-Sit D, et al. In vivo corneal confocal microscopy comparison of intralase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006; 47:2803–11.
Article38. Carlson EC, Wang IJ, Liu CY, et al. Altered KSPG expression by keratocytes following corneal injury. Mol Vis. 2003; 9:615–23.39. Sundarraj N, Fite D, Belak R, et al. Proteoglycan distribution during healing of corneal stromal wounds in chick. Exp Eye Res. 1998; 67:433–42.
Article40. Toti P, Tosi GM, Traversi C, et al. CD-34 stromal expression pattern in normal and altered human corneas. Ophthalmology. 2002; 109:1167–71.
Article41. Espana EM, Kawakita T, Liu CY, Tseng SC. CD-34 expression by cultured human keratocytes is downregulated during myofibroblast differentiation induced by TGF-beta1. Invest Ophthalmol Vis Sci. 2004; 45:2985–91.42. Ljubimov AV, Burgeson RE, Butkowski RJ, et al. Extracellular matrix alterations in human corneas with bullous keratopathy. Invest Ophthalmol Vis Sci. 1996; 37:997–1007.43. Funderburgh JL, Hevelone ND, Roth MR, et al. Decorin and biglycan of normal and pathologic human corneas. Invest Ophthalmol Vis Sci. 1998; 39:1957–64.44. Ivarsen A, Thøgersen J, Keiding SR, et al. Plastic particles at the LASIK interface. Ophthalmology. 2004; 111:18–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Result of Femtosecond Laser Assisted Descemet's Membrane Stripping Endothelial Keratoplasty
- Descemet Membrane Endothelial Keratoplasty to Treat Graft Failure after Descemet Stripping Endothelial Keratoplasty
- Manual Preparation of Donor Lenticule Using Artificial Anterior Chamber for Descemet's Membrane Stripping Endothelial Keratoplasty
- Comparison of the Long-term Clinical Outcomes of Penetrating Keratoplasty Using a Manual Trephine and Femtosecond-Laser Trephination
- Case Report: Femtosecond Laser-Assisted Small Incision Deep Lamellar Endothelial Keratoplasty