J Korean Ophthalmol Soc.
2016 Jan;57(1):125-129. 10.3341/jkos.2016.57.1.125.
A Case of Acute Retinal Necrosis in Healthy Childhood
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. parkjm@gnu.ac.kr
- 2Institute of Health Science, Gyeongsang National University, Jinju, Korea.
- KMID: 2213857
- DOI: http://doi.org/10.3341/jkos.2016.57.1.125
Abstract
- PURPOSE
To describe a case of acute retinal necrosis (ARN) in childhood.
CASE SUMMARY
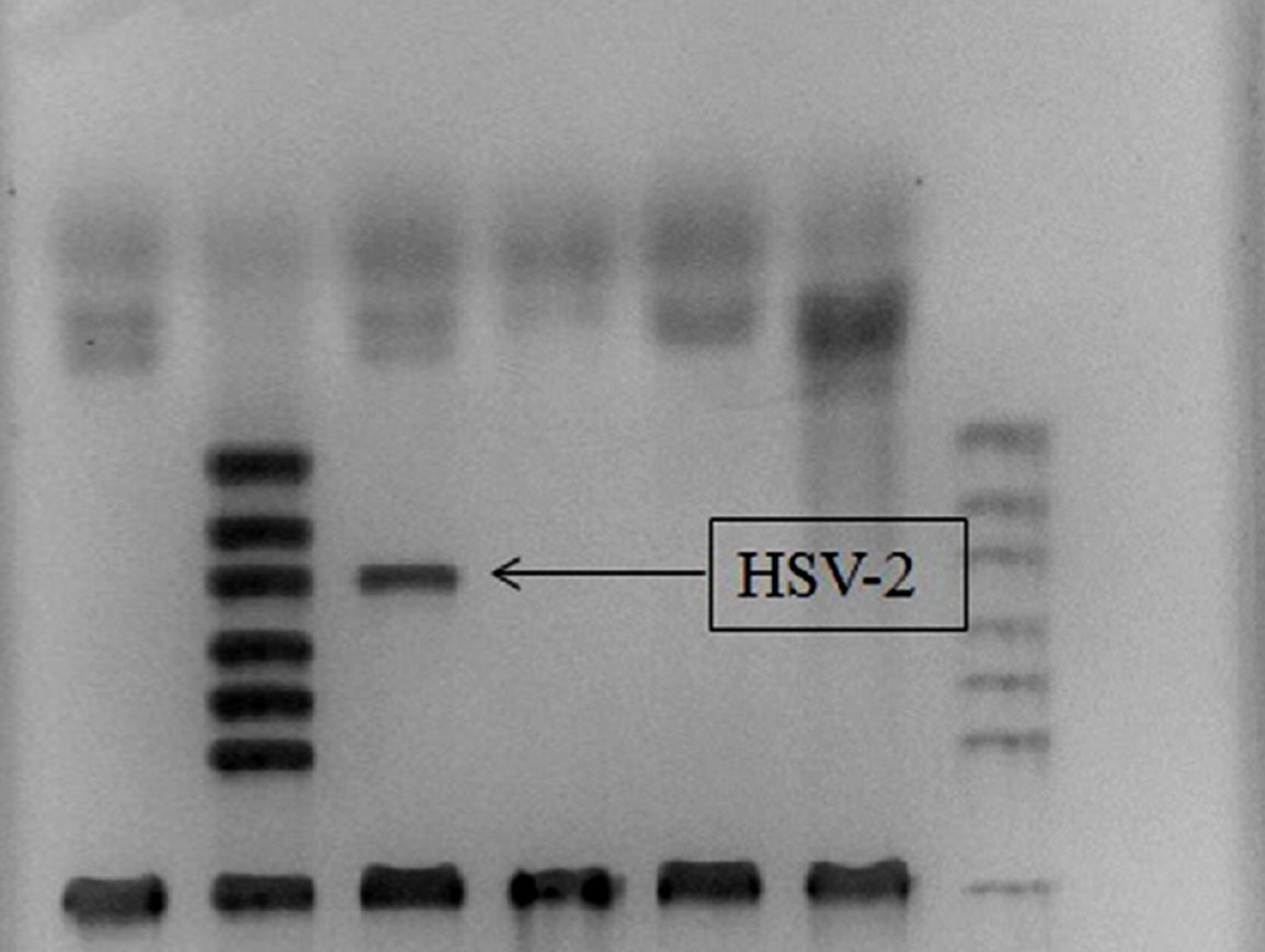
A 6-year-old child visited our clinic complaining of conjunctival injection and decreased visual acuity in the left eye. Slit-lamp examination showed conjunctival injection, inflammatory cells (4+) in the anterior chamber, and keratic precipitates. Fundus examination showed disc swelling. The patient was treated with 30 mg of oral prednisolone and 1% prednisolone acetate with the suspicion of uveitis. After 2 days, retinal examination showed a peripheral multifocal yellowish patch and retinal hemorrhage. Herpes simplex virus-2 was detected using polymerase chain reaction (PCR) analysis of the aqueous humor, which was obtained by anterior chamber paracentesis. In the present case, ARN in childhood was successfully treated with intravenous acyclovir.
CONCLUSIONS
We report a case of ARN in childhood diagnosed using PCR. Intravenous acyclovir may be an effective therapy in children with ARN. Ophthalmologists should promptly perform PCR analysis in patients diagnosed with ARN.
MeSH Terms
Figure
Reference
-
References
1. Holland GN. Standard diagnostic criteria for the acute retinal ne-crosis syndrome. Executive Committee of the American Uveitis Society. Am J Ophthalmol. 1994; 117:663–7.2. Rungger-Brändle E. Roux L. Leuenberger PM. Bilateral acute reti-nal necrosis (BARN). Identification of the presumed infectious agent. Ophthalmology. 1984; 91:1648–58.3. Urayama A, Yamada N, Sasaki T. . Unilateral acute uveitis with retinal periarteritis and detachment. Jpn J Clin Ophthalmol. 1971; 25:607–19.4. Silva RA, Berrocal AM, Moshfeghi DM. . Herpes simplex vi-rus type 2 mediated acute retinal necrosis in a pediatric population: case series and review. Graefes Arch Clin Exp Ophthalmol. 2013; 251:559–66.
Article5. Cottet L, Kaiser L, Hirsch HH, Baglivo E. HSV2 acute retinal ne-crosis: diagnosis and monitoring with quantitative polymerase chain reaction. Int Ophthalmol. 2009; 29:199–201.
Article6. Flaxel CJ, Yeh S, Lauer AK. Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syn-drome (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2013; 111:133–44.7. Lau CH, Missotten T, Salzmann J. Lightman SL. Acute retinal ne-crosis features, management, and outcomes. Ophthalmology. 2007; 114:756–62.8. Freeman WR, Lerner CW, Mines JA. . A prospective study of the ophthalmologic findings in the acquired immune deficiency syndrome. Am J Ophthalmol. 1984; 97:133–42.
Article9. Culbertson WW, Blumenkranz MS, Haines H. . The acute reti-nal necrosis syndrome. Part 2: histopathology and etiology. Ophthalmology. 1982; 89:1317–25.10. Lewis ML, Culbertson WW, Post JD. . Herpes simplex virus type 1. A cause of the acute retinal necrosis syndrome. Ophthalmology. 1989; 96:875–8.11. Green LK, Pavan-Langston D. Herpes simplex ocular in-flammatory disease. Int Ophthalmol Clin. 2006; 46:27–37.
Article12. Van Gelder RN. Willig JL. Holland GN. Kaplan HJ. Herpes sim-plex virus type 2 as a cause of acute retinal necrosis syndrome in young patients. Ophthalmology. 2001; 108:869–76.
Article13. Ganatra JB, Chandler D, Santos C. . Viral causes of the acute retinal necrosis syndrome. Am J Ophthalmol. 2000; 129:166–72.
Article14. Grose C. Acute retinal necrosis caused by herpes simplex virus type 2 in children: reactivation of an undiagnosed latent neonatal herpes infection. Semin Pediatr Neurol. 2012; 19:115–8.
Article15. An TS, Kwon SI, Hwang DJ. Park JW. A case of acute retinal ne-crosis following herpes simplex virus (HSV) encephalitis. J Korean Ophthalmol Soc. 2012; 53:1186–9.
Article16. Silva RA, Berrocal AM, Moshfeghi DM. . Herpes simplex vi-rus type 2 mediated acute retinal necrosis in a pediatric population: case series and review. Graefes Arch Clin Exp Ophthalmol. 2013; 251:559–66.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Retinal Necrosis Syndrome in an Immunosuppressed Kidney Transplant Patient
- 4 Cases of Acute Retinal Necrosis
- 5 Cases of Acute Retinal Necrosis
- Treatment of Acute Retinal Necrosis with Intravenous Acyclovir
- Vitrectomy and Silicone Oil Tamponade to Prevent Retinal Detachment in Severe Acute Retinal Necrosis Syndrome