J Korean Ophthalmol Soc.
2009 May;50(5):762-768. 10.3341/jkos.2009.50.5.762.
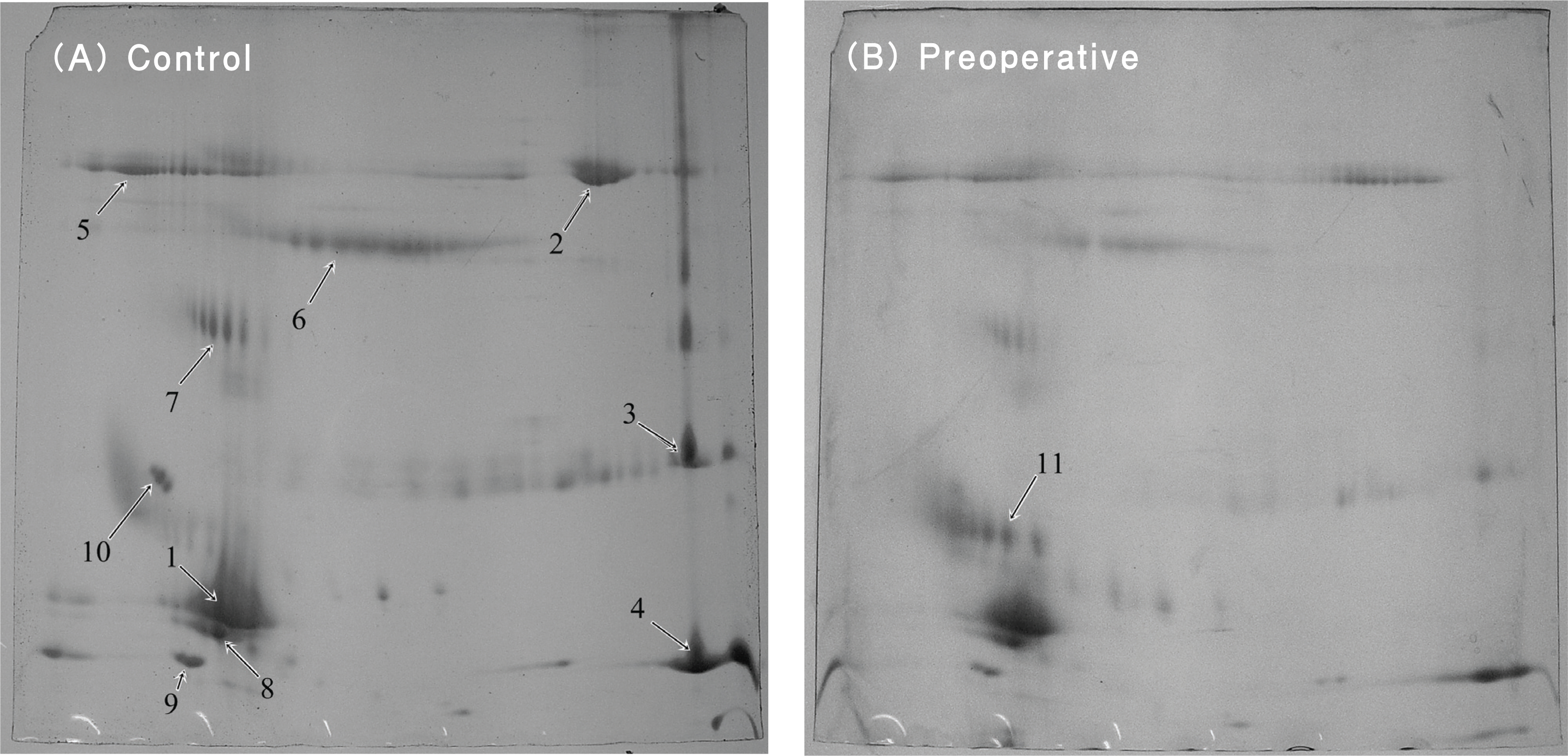
Comparative Analysis of the Tear Protein Expression After Photorefractive Keratectomy Using Two-Dimensional Electrophoresis
- Affiliations
-
- 1Department of Ophthalmology, Military Manpower Administration, Seoul, Korea. sg50@lycos.co.kr
- 2Department of Ophthalmology, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea.
- 3Department of Ophthalmology, Nune Eye Hospital, Seoul, Korea.
- KMID: 2212319
- DOI: http://doi.org/10.3341/jkos.2009.50.5.762
Abstract
-
PURPOSE:To investigate the change in the tear protein composition of patients who underwent refractive surgery.
METHODS
Tear samples were collected before photorefrative keratectomy (PRK), on the first, the second, and the third postoperative day, and then a month after the operation from 40 eyes of 20 patients. These tear samples were analyzed using two-dimensional gel electrophoresis (2-DE). Matrix-associated laser desorption/ionization time of flight (MALDI-TOF) was employed for the identification of expressed proteins. Control tear samples were collected from 40 eyes of 20 healthy volunteers who had no history of ocular surgery or pathology.
RESULTS
On the first postoperative day, lipocalin-1 precursor, lipocalin-1, and lysozyme were up-regulated. On the second postoperative day, serum albumin precursor and serum albumin were up-regulated. The tears collected on the third postoperative day and after 1 month had similar protein expression levels to the control group. Lipocalin 1 precursor and lysozyme were up-regulated and down-regulated after reftactive surgery, respectively. However, each protein had a different molecular weight and isopotential point.
CONCLUSIONS
The tear protein composition changed uniquely in the early postoperative period, and proteins with different isopotential points were detected after PRK. We hypothesized that the healing process might influence the expression of the tear proteins.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of the Effectiveness between Sampling Methods for Protein Analysis of Tear Fluids
Chul Hee Lee, Areum Yeo, Tae Im Kim, Kyoung Yul Seo, Eung Kweon Kim, Hyung Keun Lee
J Korean Ophthalmol Soc. 2015;56(11):1677-1683. doi: 10.3341/jkos.2015.56.11.1677.
Reference
-
References
1. Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983; 96:710–5.
Article2. Shyn KH, Yoon SC. Refractive survey 2005 in Korea. J Korean Ophthalmol Soc. 2008; 49:570–6.3. Murphy PJ, Corbett MC, O'Brart DP, et al. Loss and recovery of corneal sensitivity following photorefracitve keratectomy for myopia. J Refract Surg. 1999; 15:38–45.4. Perez-Santonja JJ, Sakla HF, Cardona C, et al. Corneal sensitivity after photorefractive keratectomy and laser in situ keratomileusis for low myopia. Am J Ophthalmol. 1999; 127:497–504.5. Kanellapoulos AJ, Pallikaris IG, Donnenfeld ED, et al. Comparison of corneal sensation following photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 1997; 23:34–8.6. Campos M, Hertzog L, Garbus JJ, McDonnell PJ. Corneal sensitivity afterphotorefractive keratectimy. Am J Ophthalmol. 1992; 114:51–4.7. Kauffmann T, Bodanowitz S, Hesse L, Kroll P. Corneal reinner-vation after photorefractive keratectomy and laser in situ keratomileusis: an in vivo study with a confocal videomicroscope. Ger J Ophthalmol. 1996; 5:508–12.8. Tervo K, Latvala T, Tervo T. Recovery of corneal innervation following photorefractive keratoabration. Arch Ophthalmol. 1994; 112:1466–70.9. Tervo T, Virtanen T, Honkanen N, et al. Tear fluid plasmin activity after excimer laser photorefractive keratectomy. Invest Ophthalmol Vis Sci. 1994; 35:3045–50.10. Vesaluoma MH, Tervo TT. Tenascin and cytokines in tear fluid after photorefractive keratectomy. J Refract Surg. 1998; 14:447–54.
Article11. Mertaniemi P, Ylatuoa S, Partanen P, Tervo T. Increased release of immunoreactive calcitonin gene-related peptide (CGRP) in tears after excimer laser keratectomy. Exp Eye Res. 1995; 60:659–65.12. Virtanen T, Ylatupa S, Mertaniemi P, et al. Tear fluid fibronectin levels after photorefractive keratectomy. J Refract Surg. 1995; 11:106–12.13. Bilgihan A, Bilgihan K, Toklu Y, et al. Ascobic acid levels in human tear after photorefractive keratectomy, transepithelial photorefractive keratectomy, and laser in situ keratomileusis. J Cataract Refract Surg. 2001; 27:585–8.14. Song WK, Lee HK, Kim HC, et al. Nerve growth factor concentration and implications in photorefractive keratectomy versus laser in situ keratomileusis. J Korean Ophthalmol Soc. 2006; 47:1349–57.15. Csutak A, Silver DM, Tozser J, et al. Plasminogen activator inhibitor in human tear after laser refractive surgery. J Cataract Refract Surg. 2008; 34:897–901.16. Fust A, Veres A, Kiszel P, et al. Changes in tear protein pattern after photorefractive keratectomy. Eur J Ophthalmol. 2003; 13:525–31.17. Joo H, Han J. Proteomics. 1st ed.Seoul: Panmun;2004. p. 38–87.18. Grus FH, Augustin AJ. Protein analysis methods in diagnosis of sicca syndrome. Ophthalmologe. 2000; 97:54–61.19. Grus FH, Augustin AJ. Analysis of tear protein patterns by a neural network as diagnostical tool for the detection of dry eyes. Electrophoresis. 1999; 20:875–80.20. Grus FH, Sabuncruo P, Augustin AJ. Quantitative analysis of tear protein profile for soft contact lenses-a clinical study. Klin Monatsbl Augenheilkd. 2001; 218:239–42.21. Herber S, Grus FH, Sabuncuo P, Augustin AJ. Two-dimensional analysis of tear fluid patterns of diabetes patients. Electrophoresis. 2001; 22:1838–44.22. Janssen PT, van Bijsterveld OP. Origin and biosynthesis of human tear fluid proteins. Invest Ophthalmol Vis Sci. 1983; 24:623–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Changes of Tear Break-up Time and Schirmer's Test after Photore fractive Keratectomy
- Complications after Excimer Laser Photorefractive Keratectomy in Myopia
- The changes of tear break up time after myopic excimer laser photorefractive keratectomy
- Nerve Growth Factor Concentration and Implications in Photorefractive Keratectomy Versus Laser in Situ Keratomileusis
- A Case of Ocular Deviation after Excinier Laser Photorefractive Keratectomy