J Korean Soc Endocrinol.
2006 Jun;21(3):239-244. 10.3803/jkes.2006.21.3.239.
A Case of Type 1 von Hippel-Lindau (VHL) Disease associated with VHL Germline Mutation
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Korea.
- 2Department of Radiology, Kosin University College of Medicine, Korea.
- 3Korean Hereditary Tumor Registry, Cancer Research Institute, Seoul National University, Korea.
- KMID: 2200736
- DOI: http://doi.org/10.3803/jkes.2006.21.3.239
Abstract
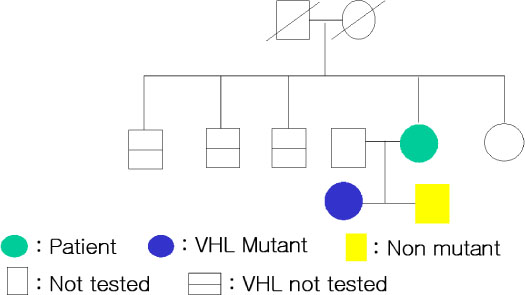
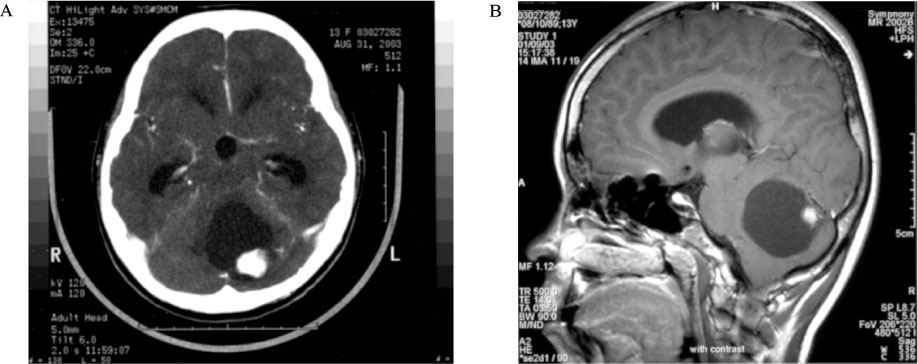
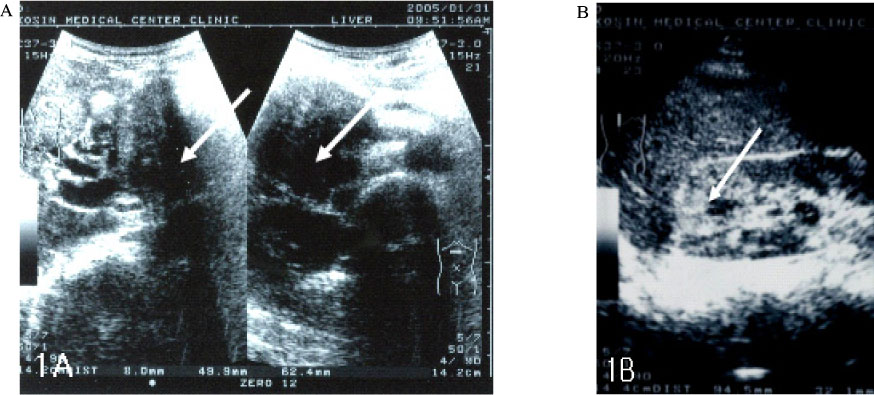
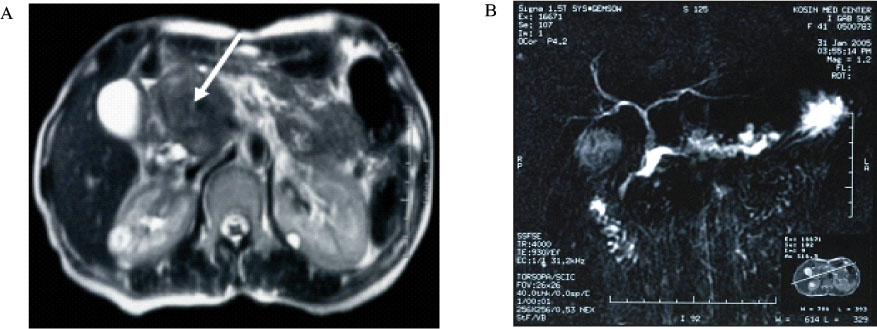
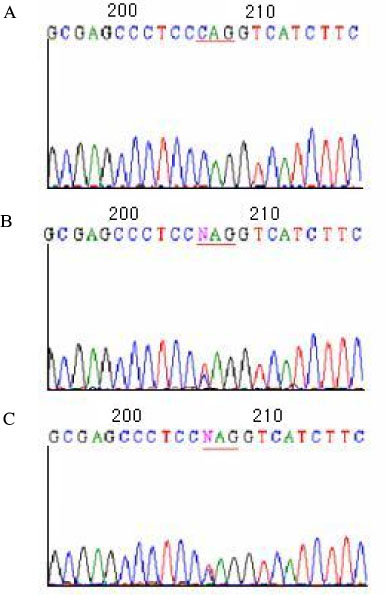
- Von Hippel-Lindau (VHL) disease is an autosomal dominant neoplasia syndrome that result from a germline mutation in the VHL gene. Germline mutation in the VHL gene lead to the development of hemangioblastomas of the central nervous system and retina, cysts and clear cell carcinoma of the kidney, cyst adenomas of other organs, and pheochromocytoma. VHL is a tumor suppressor gene on the short arm of chromosome 3. VHL disease has been classified into two main clinical subtypes depending on the presence (type 2) or absence (type 1) of pheochromocytoma. Type 2 has been subdivided into three categories depending on the presence (type 2B) or absence (type 2A) of renal cell carcinoma, with type 2C being a rare subtype in which pheochromocytoma is the sole manifestation of VHL disease. Recently we experienced a family with VHL type 1 who carry C to T (Q73X) transition in codon 217 nonsense germline mutation in exon 1 of VHL gene. The authors report this case with literature review.
MeSH Terms
Figure
Reference
-
1. Maher ER, Yates JR, Harries R, Benjamin C, Harris R, Moore AT, Ferguson-Smith MA. Clinical features and natural history of von Hippel-Lindau disease. Q J Med. 1990. 77:1151–1163.2. Chen F, Kishida T, Yao M, Hustad T, Glavac D, Dean M, Gnarra JR, Orcutt ML, Duh FM, Glenn G. Germline mutations in the von Hippel-Lindau disease tumor suppressor gene: correlations with phenotype. Hum Mutat. 1995. 5:66–75.3. Zbar B, Kishida T, Chen F, Schmidt L, Maher ER, Richards FM, Crossey PA, Webster AR, Affara NA, Ferguson-Smith MA, Brauch H, Glavac D, Neumann HP, Tisherman S, Mulvihill JJ, Gross DJ, Shuin T, Whaley J, Seizinger B, Kley N, Olschwang S, Boisson C, Richard S, Lips CH, Lerman M. Germline mutations in the von Hippel-Lindau disease (VHL) gene in families from North America, Europe, and Japan. Hum Mutat. 1996. 8:348–357.4. Kim BW, Min JK, Chon DS, Chae HS, Han SW, Chung IS, Sun HS. One case of von Hippel-Lindau disease with autosomal dominant inheritance. Korean J Med. 1993. 44:139–146.5. Kim JW, Choi SJ, Kim YK, Ahn SM, Song KE, Jung SH, Kim DJ, Chung YS, Lee KW, Kim IJ, Kang HC, Park JG. A case report of von Hippel-Lindau disease manifested in a monozygous twin. J Kor Soc Endocrinol. 2005. 20:395–400.6. Yang JH, Choi YS, Park YH, Oh KS, Chun BK, Lee SJ, Kim IJ. A case of von Hippel-Lindau (VHL) germline mutation associated with familial bilateral pheochromocytoma in the VHL disease. Korean J Med. 2005. 69:S873–S878.7. Maher ER, Iselius L, Yates JR, Littler M, Benjamin C, Harris R, Sampson J, Williams A, Ferguson-Smith MA, Morton N. Von Hippel-Lindau disease: a genetic study. J Med Genet. 1991. 28:443–447.8. Choyke PL, Glenn GM, Walther MM, Patronas NJ, Linehan WM, Zbar B. Von Hippel-Lindau disease: genetic, clinical and imaging features. Radiology. 1995. 194:629–642.9. Couch V, Lindor NM, Karnes PS, Michel VV. Review of von Hippel-Lindau disease. Mayo Clin Proc. 2000. 75:265–272.10. Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, Stackhouse T, Kuzmin I, Modi W, Geil L. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993. 260:1317–1320.11. Pause A, Lee S, Lonergan KM, Klausner RD. The von Hippel-Lindau tumor suppressor gene is required for cell cycle exit upon serum withdrawal. Proc Natl Acad Sci USA. 1998. 95:993–998.12. Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, Wykoff CC, Pugh CW, Maher ER, Ratcliffe PJ. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature. 1999. 399:271–275.13. Seizinger BR, Rouleau GA, Ozelius LJ, Lane AH, Farmer GE, Lamiell JM, Haines J, Yuen JWM, Collins D, Majoor-Krakauer D, Bonner T, Mathew C, Rubenstein A, Halperin J, McConkie-Rosell A, Green JS, Trofatter JA, Ponder BA, Eierman L, Bowmer MI, Schimke R, Oostra B, Aronin N, Smith DI, Drabkin H, Waziri MH, Hobbs WJ, Martuza RL, Conneally PM, Hsia YE, Gusella JF. von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature. 1988. 332:268–269.14. Sims KB. Von Hippel-Lindau disease: gene to bedside. Curr Opin Neurol. 2001. 14:695–703.15. Richard S, Graff J, Lindau J, Resche F. Von Hippel-Lindau disease. Lancet. 2004. 363:1231–1234.16. Filling-Katz MR, Choyke PL, Oldfield E, Charnas L, Patronas NJ, Glenn GM, Gorin MB, Morgan JK, Linehan WM, Seizinger BR. Central nervous system involvement in von Hippel-Lindau disease. Neurology. 1991. 41:41–46.17. Richard S, Campello C, Taillandier L, Parker F, Resche F. Haemangioblastoma of the central nervous system in von Hippel-Lindau disease. French VHL Study Group. J Intern Med. 1998. 243:547–553.18. Maher ER, Kaelin WG Jr. von Hippel-Lindau disease. Medicine (Baltimore). 1997. 76:381–391.19. Neumann HP, Dinkel E, Brambs H, Wimmer B, Frieburg H, Volk B, Sigmund G, Riegler P, Haag K, Schollmeyer P. Pancreatic lesions in the von Hippel-Lindau syndrome. Gastroenterology. 1991. 101:465–471.20. Marcos HB, Libutti SK, Alexander HR, Lubensky IA, Bartlett DL, Walther MM, Lienhan WM, Glenn GM, Choyke PL. Neuroendocrine tumors of the pancreas in von Hippel-Lindau disease: spectrum of appearances at CT and MR imaging with histopathologic comparison. Radiology. 2002. 225:751–758.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatic Cyst in von Hippel-Lindau Disease
- A Case of von Hippel-Lindau Disease Presenting with Pancreatic Neuroendocrine Tumor
- A Case of von Hippel-Lindau Disease with Aortic Valve Insufficiency
- Mutational Research of von Hippel-Lindau Gene of Family with von Hippel-Lindau Disease
- Brain Metastasis of Renal Cell Carcinoma in Von Hippel-Lindau Disease