J Korean Neurosurg Soc.
2015 Mar;57(3):215-218. 10.3340/jkns.2015.57.3.215.
Delayed Diagnosis of Probable Radiation Induced Spinal Cord Vascular Disorders
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea. chiheon1@snu.ac.kr
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 3Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 4Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 5Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- 6Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- KMID: 2191225
- DOI: http://doi.org/10.3340/jkns.2015.57.3.215
Abstract
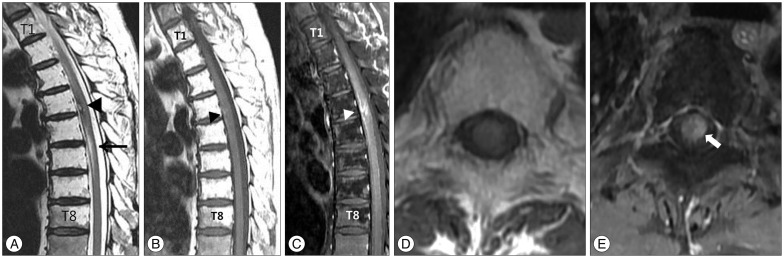
- Occasionally, unexpected neurological deficits occur after lumbar spinal surgery. We report a case of monoparesis after lumbar decompressive surgery. A 63-year-old man, who had undergone decompression of L4-5 for spinal stenosis 4 days previously in the other hospital, visted the emergency department with progressive weakness in the left leg and hypoesthesia below sensory level T7 on the right side. He had been cured of lung cancer with chemotherapy and radiation therapy 10 years previously, but detailed information of radiotherapy was not available. Whole spine magnetic resonance (MR) imaging showed fatty marrow change from T1 to T8, most likely due to previous irradiation. The T2-weighted MR image showed a high-signal T4-5 spinal cord lesion surrounded by a low signal rim, and the T1-weighted MR image showed focal high signal intensity with focal enhancement. The radiological diagnosis was vascular disorders with suspicious bleeding. Surgical removal was refused by the patient. With rehabilitation, the patient could walk independently without assistance 2 months later. Considering radiation induced change at thoracic vertebrae, vascular disorders may be induced by irradiation. If the spinal cord was previously irradiated, radiation induced vascular disorders needs to be considered.
MeSH Terms
Figure
Reference
-
1. Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone : report of eleven cases. 1948. Cancer. 1998; 82:8–34. PMID: 9428476.2. Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis. Natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987; 66:842–849. PMID: 3572515.3. Ducray F, Guillevin R, Psimaras D, Sanson M, Mokhtari K, Delanian S, et al. Postradiation lumbosacral radiculopathy with spinal root cavernomas mimicking carcinomatous meningitis. Neuro Oncol. 2008; 10:1035–1039. PMID: 18755918.
Article4. Epstein NE, Epstein JA, Carras R, Murthy VS, Hyman RA. Coexisting cervical and lumbar spinal stenosis : diagnosis and management. Neurosurgery. 1984; 15:489–496. PMID: 6493458.
Article5. Gaensler EH, Dillon WP, Edwards MS, Larson DA, Rosenau W, Wilson CB. Radiation-induced telangiectasia in the brain simulates cryptic vascular malformations at MR imaging. Radiology. 1994; 193:629–636. PMID: 7972799.
Article6. Glaser JA, Curé JK, Bailey KL, Morrow DL. Cervical spinal cord compression and the Hoffmann sign. Iowa Orthop J. 2001; 21:49–52. PMID: 11813951.7. Heckl S, Aschoff A, Kunze S. Radiation-induced cavernous hemangiomas of the brain : a late effect predominantly in children. Cancer. 2002; 94:3285–3291. PMID: 12115362.
Article8. Hsieh CH, Huang TJ, Hsu RW. Tandem spinal stenosis : clinical diagnosis and surgical treatment. Changgeng Yi Xue Za Zhi. 1998; 21:429–435. PMID: 10074729.9. Jung DY, Cho KT, Lee SC. Atypical guillain-barré syndrome misdiagnosed as lumbar spinal stenosis. J Korean Neurosurg Soc. 2013; 53:245–248. PMID: 23826482.
Article10. Labauge P, Lefloch A, Chapon F, Castelnovo G, Maubon A, Rigau V, et al. Postirradiation spinal root cavernoma. Eur Neurol. 2006; 56:256–257. PMID: 17077638.
Article11. Maraire JN, Abdulrauf SI, Berger S, Knisely J, Awad IA. De novo development of a cavernous malformation of the spinal cord following spinal axis radiation. Case report. J Neurosurg. 1999; 90(2 Suppl):234–238. PMID: 10199254.
Article12. Mathews MS, Peck WW, Brant-Zawadzki M. Brown-Séquard syndrome secondary to spontaneous bleed from postradiation cavernous angiomas. AJNR Am J Neuroradiol. 2008; 29:1989–1990. PMID: 18617590.
Article13. Narayan P, Barrow DL. Intramedullary spinal cavernous malformation following spinal irradiation. Case report and review of the literature. J Neurosurg. 2003; 98(1 Suppl):68–72. PMID: 12546391.
Article14. Nimjee SM, Powers CJ, Bulsara KR. Review of the literature on de novo formation of cavernous malformations of the central nervous system after radiation therapy. Neurosurg Focus. 2006; 21:e4. PMID: 16859257.
Article15. Sure U, Freman S, Bozinov O, Benes L, Siegel AM, Bertalanffy H. Biological activity of adult cavernous malformations : a study of 56 patients. J Neurosurg. 2005; 102:342–347. PMID: 15739564.
Article16. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010; 29:E7. PMID: 20809765.
Article17. Wilson CB. Cryptic vascular malformations. Clin Neurosurg. 1992; 38:49–84. PMID: 1537199.18. Yoshino M, Morita A, Shibahara J, Kirino T. Radiation-induced spinal cord cavernous malformation. Case report. J Neurosurg. 2005; 102(1 Suppl):101–104. PMID: 16206743.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Cord Glioblastoma Induced by Radiation Therapy of Nasopharyngeal Rhabdomyosarcoma with MRI Findings: Case Report
- Multiple Spinal Cord Recurrences of an Intracranial Ependymoma after 14 Years
- Delayed Spinal Cord Injury Following Low Voltage Electrical Accident
- Delayed Radiation Myelopathy: Serial Changes of MRI Findings
- Intervention of Vascular Diseases of the Spine