J Korean Neurosurg Soc.
2013 Mar;53(3):194-196. 10.3340/jkns.2013.53.3.194.
Dissecting Aneurysm of Vertebral Artery Manifestating as Contralateral Abducens Nerve Palsy
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea.
- 2Department of Neurosurgery, SMG-Seoul National University Boramae Medical Center, Seoul, Korea. nslee@snu.ac.kr
- 3Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2190764
- DOI: http://doi.org/10.3340/jkns.2013.53.3.194
Abstract
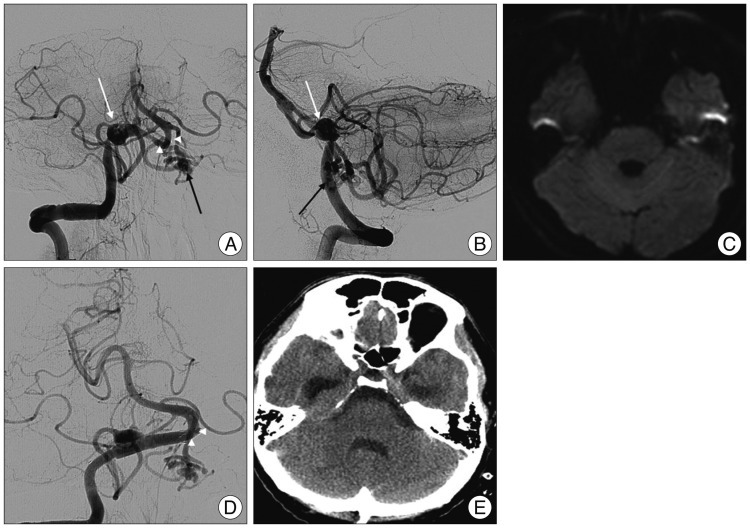
- Isolated abducens nerve paresis related to ruptured vertebral artery (VA) aneurysm is rare. It usually occurs bilaterally or ipsilaterally to the pathologic lesions. We report the case of a contralateral sixth nerve palsy following ruptured dissecting VA aneurysm. A 38-year-old man was admitted for the evaluation of a 6-day history of headache. Abnormalities were not seen on initial computed tomography (CT). On admission, the patient was alert and no signs reflecting neurologic deficits were noted. Time of flight magnetic resonance angiography revealed a fusiform dilatation of the right VA involving origin of the posterior inferior cerebellar artery. The patient suddenly suffered from severe headache with diplopia the day before the scheduled cerebral angiography. Neurologic examination disclosed nuchal rigidity and isolated left abducens nerve palsy. Emergent CT scan showed high density in the basal and prepontine cistern compatible with ruptured aneurismal hemorrhage. Right vertebral angiography illustrated a right VA dissecting aneurysm with prominent displaced vertebrobasilar artery to inferiorly on left side. Double-stent placement was conducted for the treatment of ruptured dissecting VA aneurysm. No diffusion restriction signals were observed in follow-up magnetic resonance imaging of the brain stem. Eleven weeks later, full recovery of left sixth nerve palsy was documented photographically. In conclusion, isolated contralateral abducens nerve palsy associated with ruptured VA aneurysm may develop due to direct nerve compression by displaced verterobasilar artery triggered by primary thick clot in the prepontine cistern.
MeSH Terms
-
Abducens Nerve
Abducens Nerve Diseases
Aneurysm
Aneurysm, Dissecting
Angiography
Arteries
Brain Stem
Cerebral Angiography
Diffusion
Dilatation
Diplopia
Follow-Up Studies
Headache
Hemorrhage
Humans
Magnetic Resonance Angiography
Magnetic Resonance Imaging
Muscle Rigidity
Neurologic Examination
Neurologic Manifestations
Paresis
Subarachnoid Hemorrhage
Vertebral Artery
Figure
Reference
-
1. Coppeto JR, Chan YS. Abducens nerve paresis caused by unruptured vertebral artery aneurysm. Surg Neurol. 1982; 18:385–387. PMID: 7179103.
Article2. Dumas S, Shults WT. Abducens paresis. A rare presenting sign of posterior-inferior cerebellar artery aneurysm. J Clin Neuroophthalmol. 1982; 2:55–60. PMID: 6226689.3. Duvoisin RC, Yahr MD. Posterior Fossa Aneurysms. Neurology. 1965; 15:231–241. PMID: 14262321.
Article4. Göksu E, Akyüz M, Gürkanlar D, Tuncer R. Bilateral abducens nerve palsy following ruptured anterior communicating artery aneurysm : report of 2 cases. Neurocirugia (Astur). 2007; 18:420–422. PMID: 18008016.
Article5. Hirose Y, Nakamura T, Takamiya Y, Kinoshita N, Hirai H. Fusiform superior cerebellar artery aneurysm presenting with contralateral abducens nerve paresis--case report. Neurol Med Chir (Tokyo). 1990; 30:119–122. PMID: 1695332.
Article6. Hoeoek O, Norlen G, Guzman J. Saccular Aneurysms of the Vertebral-Basilar Arterial System. A Report of 28 Cases. Acta Neurol Scand. 1963; 39:271–304. PMID: 14082563.7. Morioka T, Matsushima T, Yokoyama N, Muratani H, Fujii K, Fukui M. Isolated bilateral abducens nerve palsies caused by the rupture of a vertebral artery aneurysm. J Clin Neuroophthalmol. 1992; 12:263–267. PMID: 1287052.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Bilateral Abducens Nerve Palsy Caused by Basilar Artery Dissecting Aneurysm
- Stent Assisted Coil Embolization of a Dissecting Aneurysm of the Vertebral Artery: A Case Involving a Patient with Hypoplasia of the Contralateral Vertebral Artery
- Unilateral Abducens Nerve Palsy Associated with Ruptured Anterior Communicating Artery Aneurysm
- Isolated ipsilateral abducens nerve palsy and contralateral homonymous hemianopsia associated with unruptured posterior cerebral artery aneurysm: A rare neurological finding
- Dissecting Aneurysm of the Intracranial Vertbral Artery: Case Report