J Korean Assoc Oral Maxillofac Surg.
2010 Apr;36(2):71-77. 10.5125/jkaoms.2010.36.2.71.
The effect of platelet rich plasma in bone formation on implant installation in the tibia of beagle dogs
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Dental Science Research Insitutue, Chonnam National University, Gwang-Ju, Korea. hkoh@jnu.ac.kr
- 2Department of Radiology, Nambu University, Gwang-Ju, Korea.
- 3College of Veterinary Medicine, Chonnam National University, Gwang-Ju, Korea.
- KMID: 2189972
- DOI: http://doi.org/10.5125/jkaoms.2010.36.2.71
Abstract
- INTRODUCTION
The purpose of this study is to evaluate the effect of platelet rich plasma in bone formation and osseointegration of implant installed in the bone marrow space.
MATERIALS AND METHODS
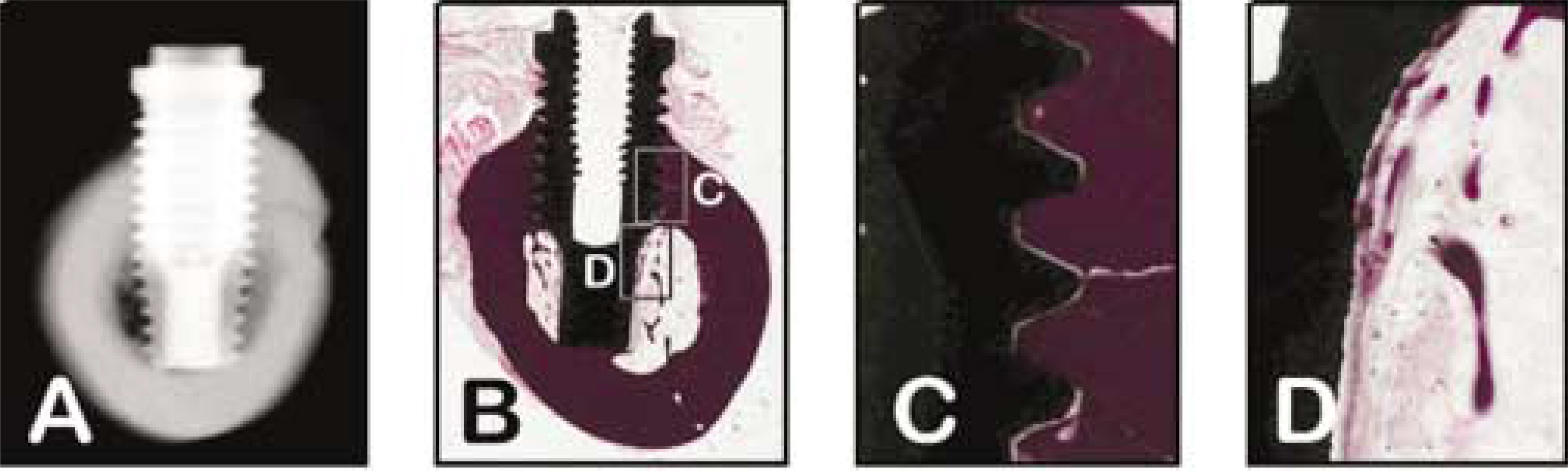
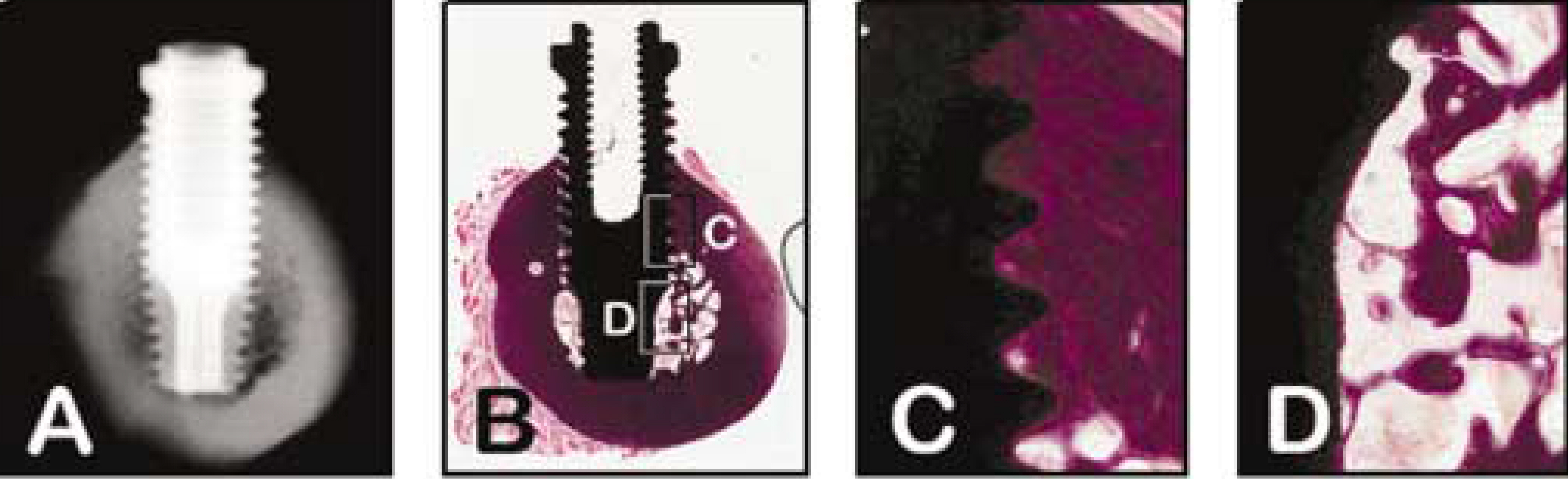
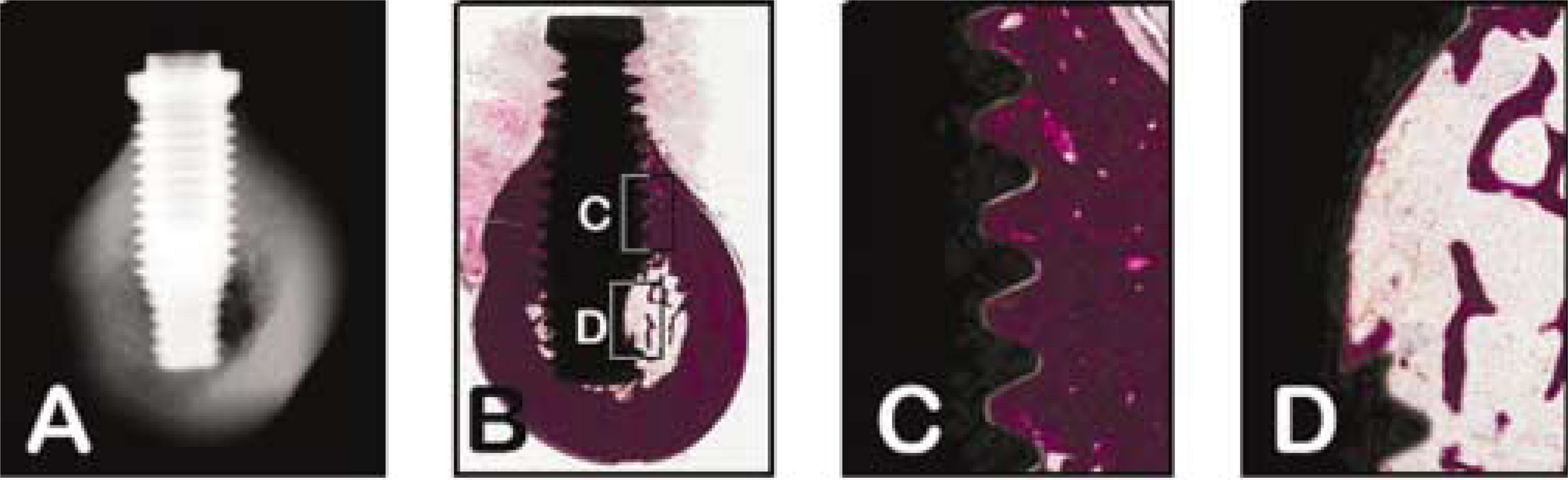
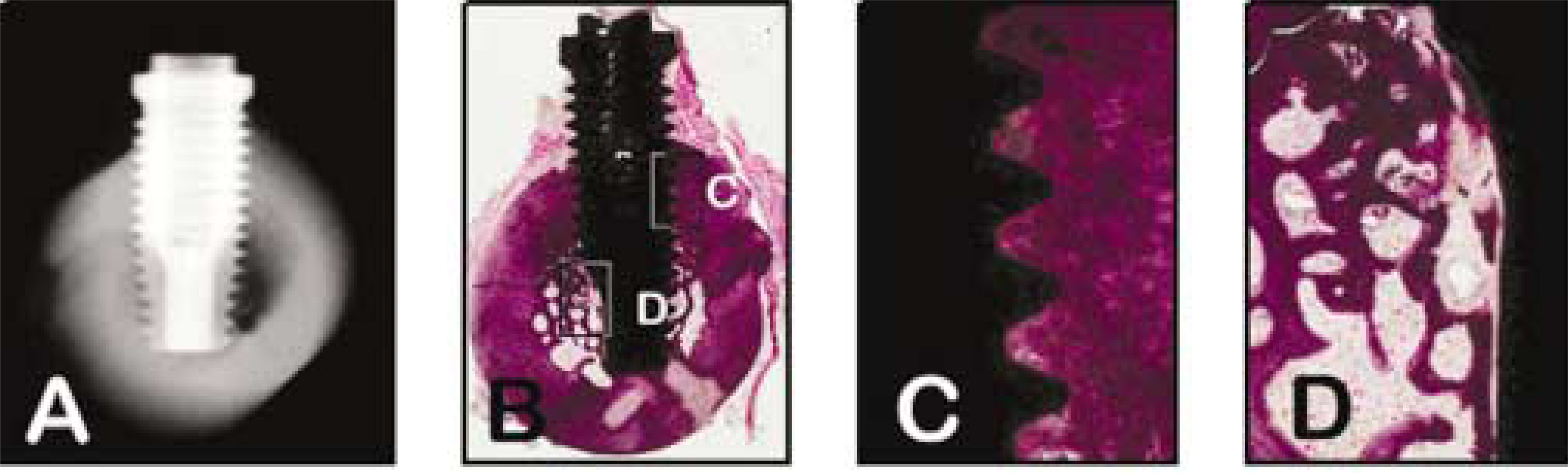
Five beagle dogs were used as experimental animals. Two implants were installed on each tibia in the dogs. Implants of the control group were installed with no additional graft. Those of the experimental group 1 were installed with autogenous bone graft from the ilium autogenous bone. Platelet rich plasma (PRP) alone was used in experimental group 2 and the mixture of PRP and autogenous bone was used in experimental group 3. The animals were sacrificed at 8 weeks after implantation. The parts of tibia containing implant were harvested and radiographs were taken for radiographic examination. The specimens were prepared for histological examination and histomorphometric analysis of implant-bone contact ratios.
RESULTS
1. All implants showed sufficient osseointegration in the cortical bone radiographically and histologically, but osseointergration in the marrow space was not satisfactory. 2. Histomorphometrically, the implant-bone contact ratios in the bone marrow was sequentially high in the experimental group 3 (autogenous bone + PRP group), group 1 (autogenous bone group), group 2 (PRP group), and control group (non-additive). 3. It was verified that there was statistical significance between two experimental groups (group 1 and 3) and the other groups (group 2 and control group). (P<0.005) 4. However, there was no statistical significance between group 3 and group 1, also group 2 and control group respectively.
CONCLUSION
These results suggest that platelet rich plasma is effective to osseointegration in the implant installation but there is no statistical significance.
MeSH Terms
Figure
Reference
-
References
1. Hutton JE, Heath MR, Chai JY, Harnett J, Jemt T, Johns RB, et al. Factors related to success and failure rates at 3-year follow-up in a multicenter study of overdentures supported by Bra � nemark implants. Int J Oral Maxillofac Implants. 1995; 10:33–42.2. Jaffin RA, Berman CL. The excessive loss of Bra � nemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991; 62:2–4.3. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 85:638–46.4. Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res. 2008; 19:539–45.
Article5. Whitman DH, Berry RL, Green DM. Platelet gel: an autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1997; 55:1294–9.
Article6. Kassolis JD, Reynold MA. Evaluation of the adjunctive benefits of platelet-rich plasma in subantral sinus augmentation. J Craniofac Surg. 2005; 16:280–7.
Article7. Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzarevic M, Kenney EB. Platelet-rich plasma and bovine porous bone mineral combined with guided tissue regeneration in the treatment of intrabony defects in humans. J Periodontal Res. 2002; 37:300–6.
Article8. Lekovic V, Camargo PM, Weinlaender M, Vasilic N, Aleksic Z, Kenney EB. Effectiveness of a combination of platelet-rich plasma, bovine porous bone mineral and guided tissue regeneration in the treatment of mandibular grade II molar furcations in humans. J Clin Periodontol. 2003; 30:746–51.
Article9. Fennis JP, Stoelinga PJ, Jansen JA. Mandibular reconstruction: a histological and histomorphometric study on the use of autogenous scaffolds, particulate cortico-cancellous bone grafts and platelet rich plasma in goats. Int J Oral Maxillofac Surg. 2004; 33:48–55.
Article10. Nikolidakis D, van den Dolder J, Wolke JG, Stoelinga PJ, Jansen JA. The effect of platelet-rich plasma on the bone healing around calcium phosphate-coated and non-coated oral implants in trabecular bone. Tissue Eng. 2006; 12:2555–63.
Article11. Froum SJ, Wallace SS, Tarnow DP, Cho SC. Effect of platelet-rich plasma on bone growth and osseointegration in human maxillary sinus grafts: three bilateral case reports. Int J Periodontics Restorative Dent. 2002; 22:45–53.12. Monov G, Fuerst G, Tepper G, Watzak G, Zechner W, Watzek G. The effect of platelet-rich plasma upon implant stability measured by resonance frequency analysis in the lower anterior mandibles. A pilot study. Clin Oral Implants Res. 2005; 16:461–5.13. Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, van der Wal JE, Vissink A. Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? Clin Oral Implants Res. 2005; 16:349–56.
Article14. Thor A, Wannfors K, Sennerby L, Rasmusson L. Reconstruction of the severely resorbed maxilla with autogenous bone, platelet-rich plasma, and implants: 1-year results of a controlled prospective 5-year study. Clin Implant Dent Relat Res. 2005; 7:209–20.15. Plachokova AS, van den Dolder J, Stoelinga PJ, Jansen JA. The bone regenerative effect of platelet-rich plasma in combination with an osteoconductive material in rat cranial defects. Clin Oral Implants Res. 2006; 17:305–11.
Article16. Carlsson L, Ro ¨stlund T, Albrektsson B, Albrektsson T. Implant fixation improved by close fit. Cylindrical implant-bone interface studied in rabbits. Acta Orthop Scand. 1988; 59:272–5.17. Lekholm U, Zarb GA. Patient selection and preparation. Bra � nemark PI, Zarb GA, Albrektsson T, editors. Tissue integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence;1985. p. 199–209.19. Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery-clinical, prospective, biomechanical, and imaging study. Bone. 2005; 37:776–80.
Article20. Branemark R, Ohrnell L, Skalak R, Carlsson L, Branemark PI. Biomechanical characterization of osseointegration: an experimental in vivo investigation in the beagle dog. J Orthop Res. 1998; 16:61–9.21. Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004; 62:489–96.
Article22. Roussy Y, Bertrand Duchesne MP, Gagnon G. Activation of human platelet-rich plasmas: effect on growth factors release, cell division and in vivo bone formation. Clin Oral Implants Res. 2007; 18:639–48.
Article23. Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001; 10:225–8.
Article24. Stimulation of in vitro human skin collagenase expression by platelet-derived growth factor. Proc Natl Acad Sci USA. 1985; 82:4132–6.25. Tzeng DY, Deuel TF, Huang JS, Baehner RL. Platelet-derived growth factor promotes human peripheral monocyte activation. Blood. 1985; 66:179–83.
Article26. Miyazono K, Ten Dijke P, Ichijo H, Heldin CH. Receptors for transforming growth factor-beta. Adv Immunol. 1994; 55:181–220.27. Canalis E, Centrella M, Burch W, McCarthy TL. Insulin-like growth factor I mediates selective anabolic effects of parathyroid hormone in bone cultures. J Clin Invest. 1989; 83:60–5.
Article28. Jakse N, Tangl S, Gilli R, Berghold A, Lorenzoni M, Eskici A, et al. Influence of PRP on autogenous sinus grafts. An experimental study on sheep. Clin Oral Implants Res. 2003; 14:578–83.29. Kim SG, Chung CH, Kim YK, Park JC Lim SC. Use of particulate dentin plaster of paris combination with/without platelet-rich plasma in the treatment of bone defects around implants. Int J Oral Maxillofac Implants. 2002; 17:86–94.30. Butterfield KJ, Bennett J, Gronowicz G, Adams D. Effect of platelet-rich plasma with autogenous bone graft for maxillary sinus augmentation in a rabbit model. J Oral Maxillofac Surg. 2005; 63:370–6.
Article31. Sa′nchez AR, Sheridan PJ, Kupp LI. Is platelet-rich plasma the perfect enhancement factor? A current review. Int J Oral Maxillofac Implants. 2003; 18:93–103.32. Anitua E, Sa′nchez M, Nurden AT, Nurden P, Orive G, Andia I. New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol. 2006; 24:227–34.
Article33. Hallman M, Thor A. Bone substitutes and growth factors as an alternative/complement to autogenous bone for grafting in implant dentistry. Periodontol 2000. 2008; 47:172–92.
Article34. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003; 8:328–43.
Article35. Schlegel KA, Donath K, Rupprecht S, Falk S, Zimmermann R, Felszeghy E, et al. De novo bone formation using bovine collagen and platelet-rich plasma. Biomaterials. 2004; 25:5387–93.
Article36. Wiltfang J, Kloss FR, Kessler P, Nkenke E, Schultze-Mosgau S, Zimmermann R, et al. Effects of platelet-rich plasma on bone healing in combination with autogenous bone and bone substitutes in critical-size defects. An animal experiment. Clin Oral Implants Res. 2004; 15:187–93.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Regenerative effects of Platelet-Rich Plasma and Enamel Matrix Protein on Grade III Furcation defects in beagle dogs
- The Effect of Platelet Rich Plasma Combined with Bovine Bone on the Treatment of Grade II Furcation Defects in Beagle Dogs
- The Effects of various Regeneration techniques on Bone Regeneration around Dental Implant
- The Effects of Platelet-Rich Plasma on Regeneration around Dental Implant Defects
- The Effect of Platelet Rich Plasma Combined with Bovine Bone on the Treatment of Grade II Furcation Defects in Beagle Dogs