J Korean Med Assoc.
2006 Dec;49(12):1141-1153. 10.5124/jkma.2006.49.12.1141.
Recent Knowledge of Breast Reconstruction
- Affiliations
-
- 1Department of Plastic and Reconstruction Surgery, The Catholic University of Korea College of Medicine, Korea. pklee@catholic.ac.kr
- KMID: 2184744
- DOI: http://doi.org/10.5124/jkma.2006.49.12.1141
Abstract
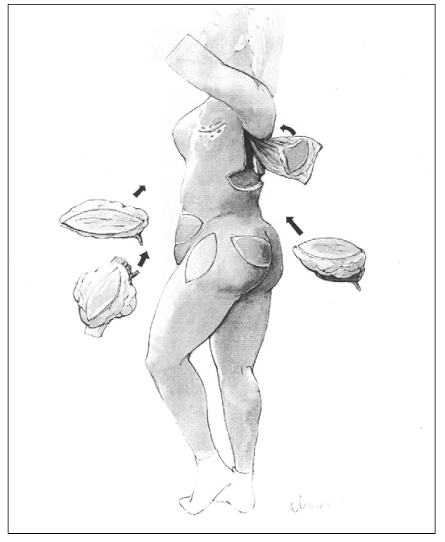
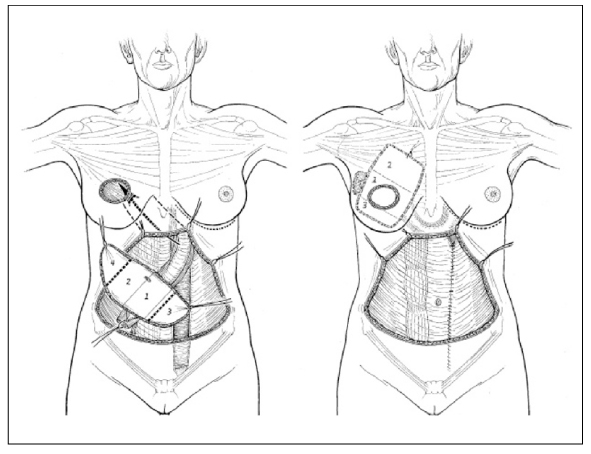
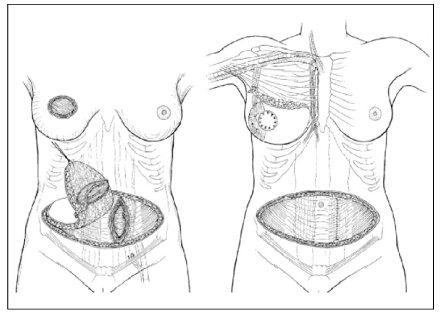
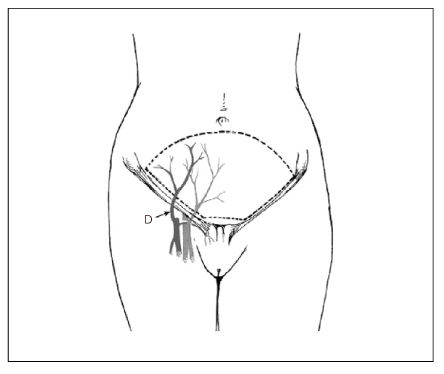
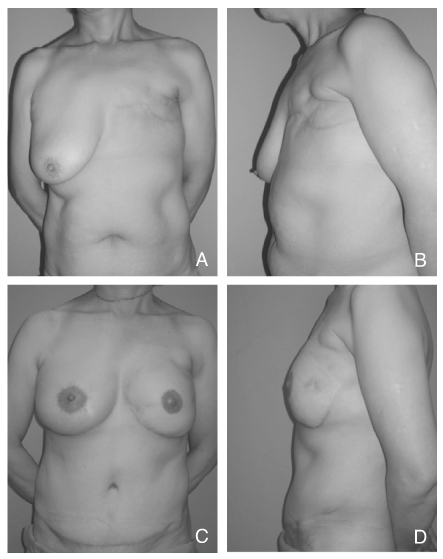
- Breast is one of the most important organ which characterize the femininity and the maternity. As growing not only in numbers of breast cancer patients but also concerns about the quality of life, breast reconstruction after mastectomy turns into hot topics in the area of plastic surgery. Historically, numerous operation techniques have been introduced for breast reconstruction using prosthesis (tissue expander and breast implant) and autologous tissues (various pedicled flaps and free flaps). The most ideal method for breast reconstruction is to make a natural soft breast with less complications and morbidities, and no single technique can be universally accepted in every cases. However, in terms of making a natural, good-looking breast autologous tissue is more superior to tissue expander and breast implant in breast reconstruction. Usually a breast reconstruction is performed in 3 stages; 1st stage is breast mound reconstruction using autologous tissue or tissue expander and implant. 2nd stage is revision of the reconstructed breast and donor site such as abdomen (scar revision, volume adjustment using suction-assisted lipectomy and excision), nipple reconstruction, and surgery of the opposite normal breast (augmentation, mastopexy, or reduction) for maximizing cosmetic results. 3rd stage is a intradermal tattooing for nipple-areolar complex. In this article, various techniques are presented with their indications, methods, advantages and disadvantages. For the choice of best modality, many factors should be considered including an extent of mastectomy, the size and shape of opposite breast, the condition of possible donor sites, postoperative adjuvant therapy (radiation, chemotherapy), patient's age, and patient's preferance.
Keyword
MeSH Terms
Figure
Reference
-
1. Bae YC, Kim SH, Kim JH, Bae YT. A study on the perception of breast reconstruction in mastectomized patients and general population in Korea. J Korean Soc Plast Reconstr Surg. 1997. 24:1062–1075.2. Becker H. Breast reconstruction using an inflatable breast implant with detachable reservoir. Plast Reconstr Surg. 1984. 73:678–683.
Article3. Maxwell GP. Iginio Tansini and the origin of the latissimus dorsi musculocutaneous flap. Plast Reconstr Surg. 1980. 65:686–692.
Article4. Schneider WJ, Hill HL Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg. 1977. 30:277–281.
Article5. Fujino T, Harashina T, Enomoto K. Primary breast reconstruction after a standard radical mastectomy by a free flap transfer. Case report. Plast Reconstr Surg. 1976. 58:371–374.
Article6. Robbins TH. Rectus abdominis myocutaneous flap for breast reconstruction. Aust N Z J Surg. 1979. 49:527–530.
Article7. Scheflan M, Hartrampf CR, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982. 69:908–909.8. Germann G, Steinau HU. Breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 1996. 97:519–526.
Article9. Chang DW, Youssef A, Cha S, Reece GP. Autologous breast reconstruction with the extended latissimus dorsi flap. Plast Reconstr Surg. 2002. 110:751–759. discussion 760-751.
Article10. Beckenstein MS, Grotting JC. Breast reconstruction with free-tissue transfer. Plast Reconstr Surg. 2001. 108:1345–1353. quiz 1354.
Article11. Arnez ZM, Khan U, Pogorelec D, Planinsek F. Breast reconstruction using the free superficial inferior epigastric artery (SIEA) flap. Br J Plast Surg. 1999. 52:276–279.
Article12. Chevray PM. Breast reconstruction with superficial inferior epigastric artery flaps: a prospective comparison with TRAM and DIEP flaps. Plast Reconstr Surg. 2004. 114:1077–1083. discussion 2004; 1084-75.
Article13. Ulusal BG, Cheng MH, Wei FC, Ho-Asjoe M, Song D. Breast reconstruction using the entire transverse abdominal adipocutaneous flap based on unilateral superficial or deep inferior epigastric vessels. Plast Reconstr Surg. 2006. 117:1395–1403. discussion 1404-1396.
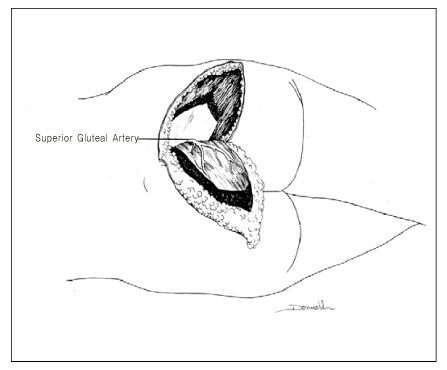
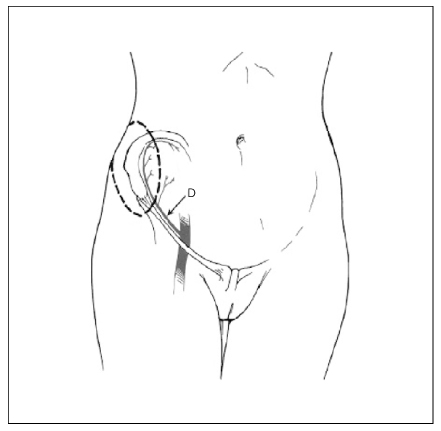
Article14. Shaw WW. Breast reconstruction by superior gluteal microvascular free flaps without silicone implants. Plast Reconstr Surg. 1983. 72:490–501.
Article15. Paletta CE, Bostwick J 3rd, Nahai F. The inferior gluteal free flap in breast reconstruction. Plast Reconstr Surg. 1989. 84:875–883. discussion 884-75.
Article16. Elliott LF, Beegle PH, Hartrampf CR Jr. The lateral transverse thigh free flap: an alternative for autogenous-tissue breast reconstruction. Plast Reconstr Surg. 1990. 85:169–178. discussion 179-81.17. Elliott LF, Hartrampf CR Jr. The Rubens flap. The deep circumflex iliac artery flap. Clin Plast Surg. 1998. 25:283–289.18. Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994. 32:32–38.
Article19. DellaCroce FJ, Sullivan SK. Application and refinement of the superior gluteal artery perforator free flap for bilateral simultaneous breast reconstruction. Plast Reconstr Surg. 2005. 116:97–103. discussion 104-5.
Article20. Allen RJ, Levine JL, Granzow JW. The in-the-crease inferior gluteal artery perforator flap for breast reconstruction. Plast Reconstr Surg. 2006. 118:333–339.
Article21. Nahabedian MY, Momen B, Galdino G, Manson PN. Breast Reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg. 2002. 110:466–475. discussion 476-67.
Article22. Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with the deep inferior epigastric perforator flap: history and an update on current technique. J Plast Reconstr Aesthet Surg. 2006. 59:571–579.
Article23. Mathes SJ. Plastic surgery. 2005. VI:2nd ed. Philadelphia: Saunders Elsevier;631–1052.24. Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg. 2006. 117:737–746. discussion 747-50.
Article25. Lee PK, Lim JH, Ahn ST, Oh DY, Rhie JW, Han KT. Nipple reconstruction with dermis(scar tissue) graft and C-V flap. J Korean Soc Plast Reconstr Surg. 2006. 33:101–106.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Findings of Postoperative Change after Breast Reconstruction
- Mondor's Disease after Immediate Breast Reconstruction with Silicone Implant
- A Clinical Study of Subcutaneous Mastectomy with Immediate Reconstruction as Treatment for Early Breast Carcinoma
- Expander/Implant Breast Reconstruction after Reconstruction Using an Extended Cutaneous Thoracoabdominal Flap: A Case Report
- How to optimize aesthetic outcomes in implant-based breast reconstruction