J Surg Ultrasound.
2022 May;9(1):8-12. 10.46268/jsu.2022.9.1.8.
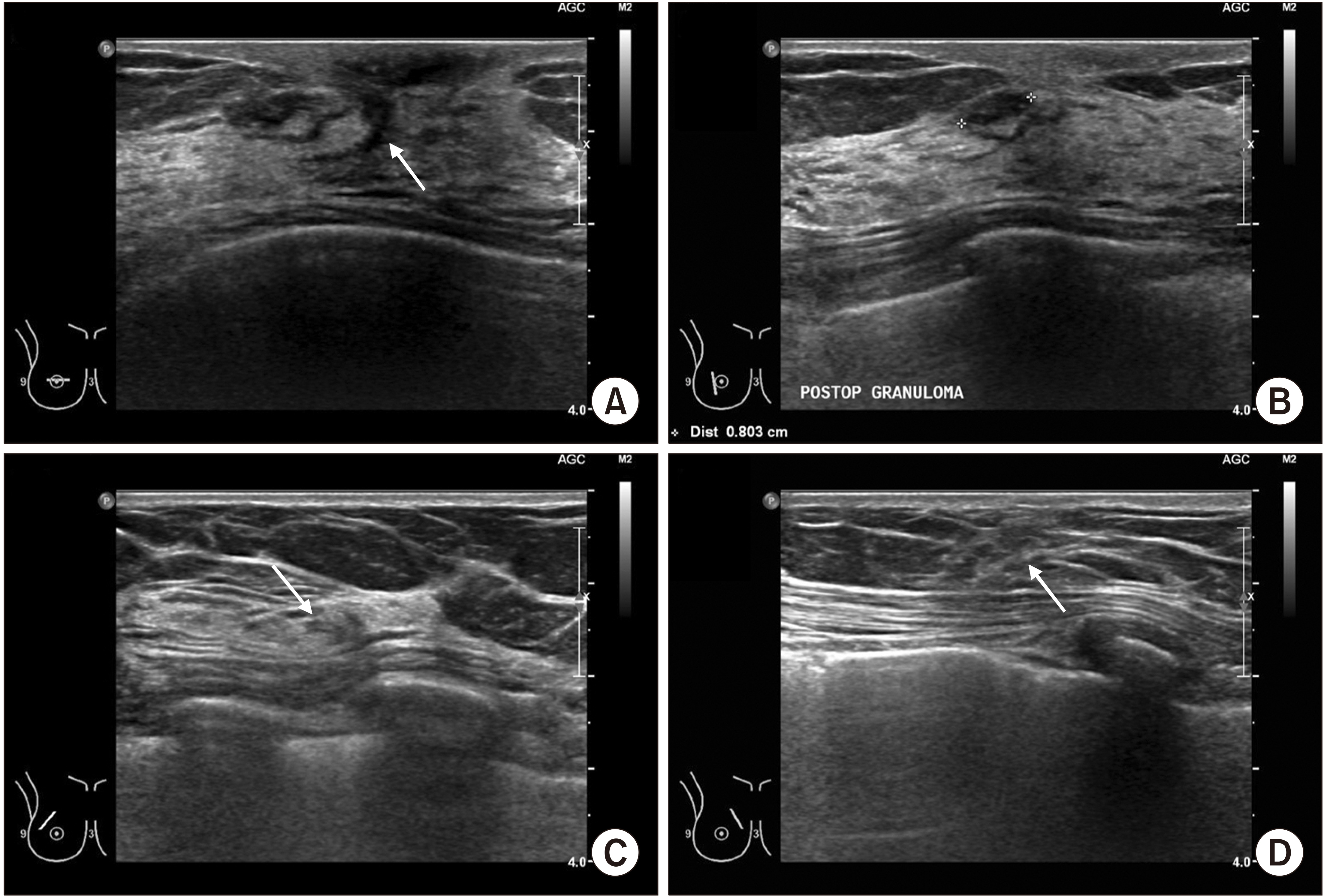
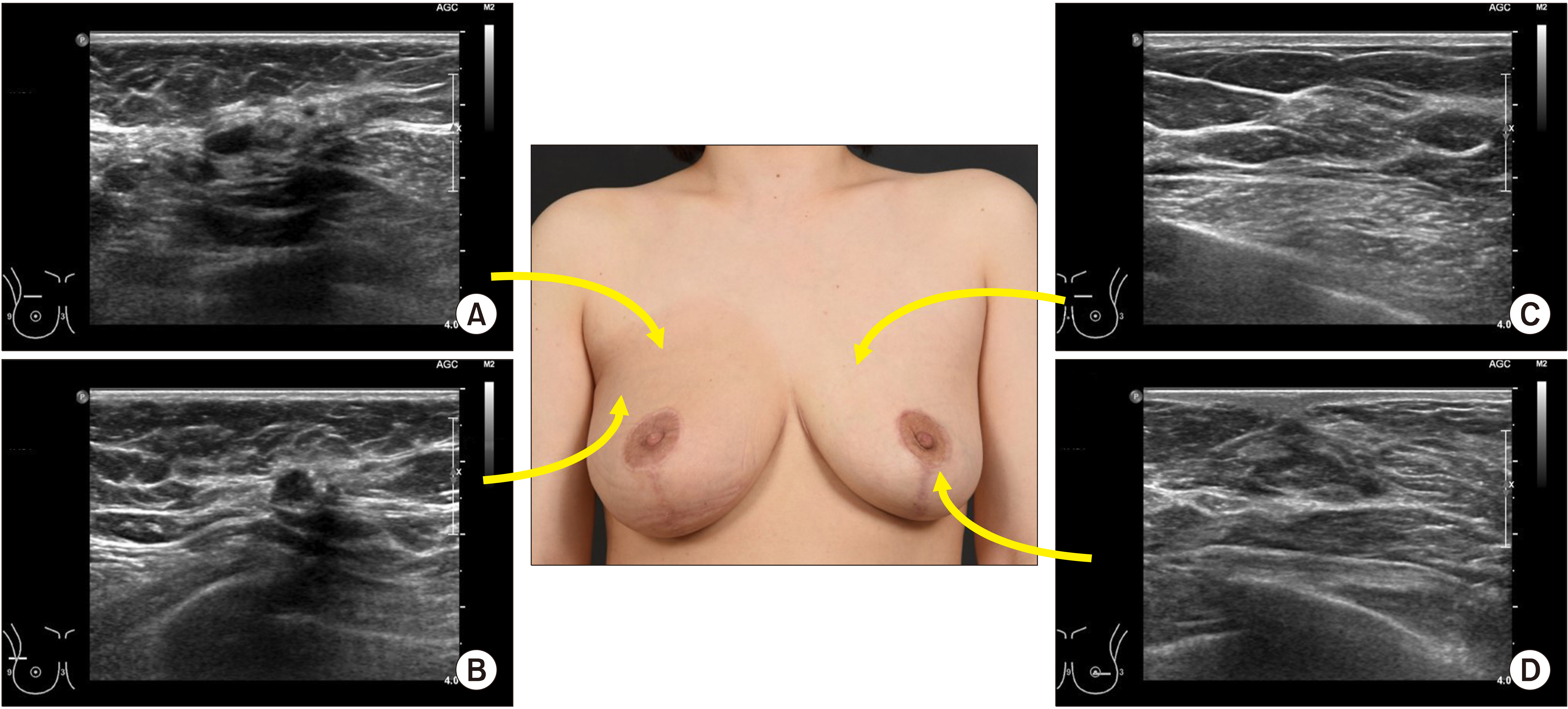
Ultrasonographic Findings of Postoperative Change after Breast Reconstruction
- Affiliations
-
- 1Department of Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2536058
- DOI: http://doi.org/10.46268/jsu.2022.9.1.8
Abstract
- Breast ultrasound is the most important tool for breast cancer surveillance after surgery. In particular, when a breast reconstruction is performed for patients with breast cancer, the sonographer should be provided with surgical information to distinguish between a benign lesion and cancer recurrence. This article describes the sonographic changes after breast reconstruction for breast cancer, which vary, but may be typical. Therefore, if breast surgeons and sonographers are aware of the typical sonographic findings, it would be helpful for the early detection and management of postoperative complications.
Figure
Reference
-
1. Korean Breast Cancer Society. 2016. Breast Cancer Facts & Figures 2016. Korean Breast Cancer Society;Seoul:2. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW. 2016; The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 19:1–7. DOI: 10.4048/jbc.2016.19.1.1. PMID: 27066090. PMCID: PMC4822102.
Article3. Margolis NE, Morley C, Lotfi P, Shaylor SD, Palestrant S, Moy L, et al. 2014; Update on imaging of the postsurgical breast. Radio-graphics. 34:642–60. DOI: 10.1148/rg.343135059. PMID: 24819786.
Article4. Heller SL, Lourenco AP, Niell BL, Ajkay N, Brown A, et al. Expert Panel on Breast Imaging. 2020; ACR Appropriateness Criteria® imaging after mastectomy and breast reconstruction. J Am Coll Radiol. 17(11S):S403–14. DOI: 10.1016/j.jacr.2020.09.009. PMID: 33153553. PMCID: PMC8173332.
Article5. Zakhireh J, Fowble B, Esserman LJ. 2010; Application of screening principles to the reconstructed breast. J Clin Oncol. 28:173–80. DOI: 10.1200/JCO.2008.21.7588. PMID: 19884555.
Article6. Jeon HJ, Park HY, Jung JH, Kim WW, Chung JH, Moon SH, et al. 2017; Usefulness of ultrasound-guided aspiration using intravenous cannulas for patients with peri-prosthetic seroma. J Surg Ultrasound. 4:18–24.7. Lee J, Kim SH, Lee JH, Han BK. 2021; Understanding silicone breast implant-associated complications for radiologists. J Korean Soc Radiol. 82:49–65. DOI: 10.3348/jksr.2020.0208.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The analysis of ultrasonographic findings in breast carcinoma
- Ultrasonographic Findings of Breast Diseases During Pregnancy and Lactating Period
- The Retrograde Limb of the Internal Mammary Artery: An Alternative Inflow Option for Free Flap Breast Reconstruction
- Ultrasonographic Findings of Post-Operative Changes after Breast Cancer Surgery
- Assessment of Breast Volume Change after Transverse Rectus Abdominis Myocutaneous Flap