J Korean Med Assoc.
2006 Aug;49(8):707-716. 10.5124/jkma.2006.49.8.707.
High-intensity Focused Ultrasound in the Solid Tumor Treatment
- Affiliations
-
- 1Department of Diagnostic Radiology / HIFU Cancer Therapy Center, The Catholic University of Korea College of Medicine, Korea. sthahn@catholic.ac.kr
- KMID: 2184700
- DOI: http://doi.org/10.5124/jkma.2006.49.8.707
Abstract
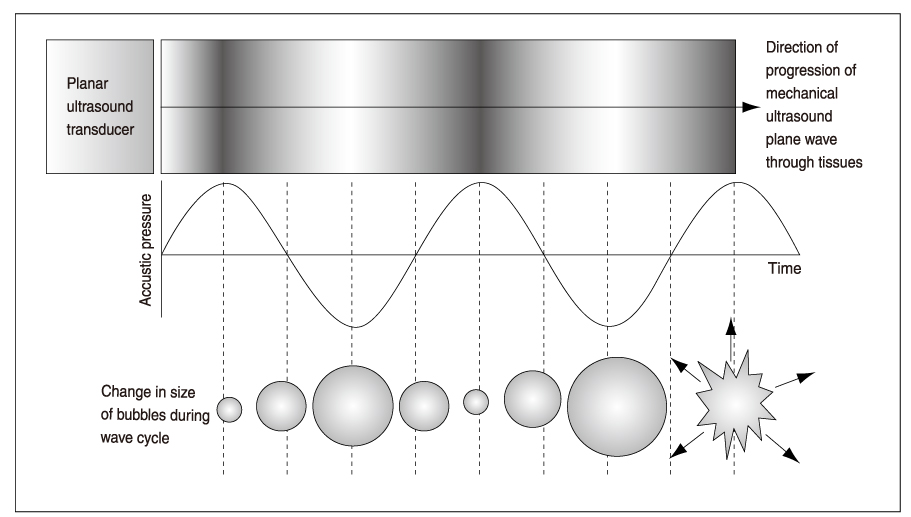
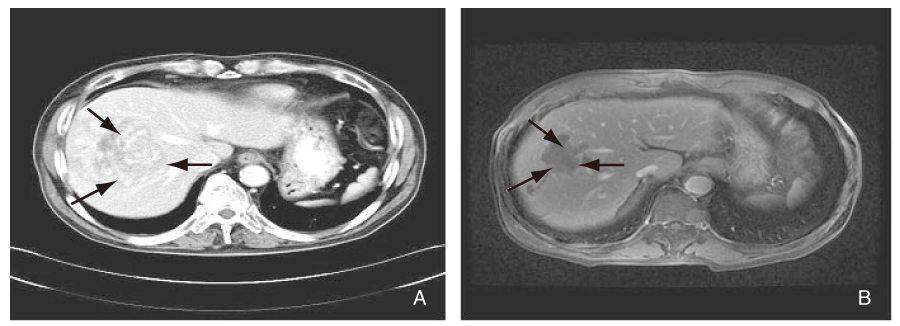
- High intensity focused ultrasound (HIFU) is a technique that was first introduced in the 1940s as a potential method of destroying selective regions within the brain to aid neurobehavioral studies. A beam of ultrasound can be delivered to a targeted focus at a distance from its source, and if a sufficient amount of energy is concentrated in the focus, the cells lying within this focal volume are selectively killed. This is, therefore, a non-invasive method of producing selective and "trackless" tissue destruction in deep-seated targets in the body without damage to the overlying tissues. Although it had not been in clinical use for a long time, HIFU is now widely used as a non-invasive treatment method for malignant tumors of the liver, kidney, breast, bone, uterus and pancreas, as well as for the relief of chronic pain of malignant origin. Further improvement of technology and imaging of HIFU in the near future will make it one of the most important tools in the treatment of solid tumors, further expanding its clinical applications.
Figure
Cited by 1 articles
-
Spontaneous Uterine Rupture during Second Trimester Pregnancy after High-intensity Focused Ultrasound
Yun Dan Kang, Choong Hak Park
Korean J Perinatol. 2015;26(4):373-376. doi: 10.14734/kjp.2015.26.4.373.
Reference
-
1. Vogl TJ, Straub R, Eichler K, Soller O, Mack MG. Colorectal carcinoma metastases in liver: laser-induced interstitial thermotherapy : local tumor control rate and survival data. Radiology. 2003. 230:450–458.
Article2. Nagaoka Y, Nakayama R, Iwata M. Cutaneous seeding following percutaneous ethanol injection therapy for hepatocellular carcinoma. Intern Med. 2004. 43:268–269.
Article3. Liu C, Frilling A, Dereskewitz C, Broelsch CE. Tumor seeding after fine needle aspiration biopsy and percutaneous radiofrequency thermal ablation of hepatocellular carcinoma. Dig Surg. 2003. 20:460–463.
Article4. Thuroff S, Chaussy C, Vallancien G, Wieland W, Kiel HJ, Gelet A, et al. High-intensity focused ultrasound and localized prostate cancer : efficacy results from the European multicentric study. J Endourol. 2003. 17:673–677.5. Kennedy JE, Wu F, ter Haar GR, Gleeson FV, Phillips RR, Middleton MR, et al. High-intensity focused ultrasound for the treatment of liver tumours. Ultrasonics. 2004. 42:931–935.
Article6. Wu F, Wang ZB, Chen WZ, Zou JZ, Bai J, Gao GW, et al. Extracorporeal focused ultrasound surgery for treatment of human solid carcinomas: early Chinese clinical experience. Ultrasound Med Biol. 2004. 30:245–250.
Article7. Gianfelice D, Kheat A, Boulanger Y, Amara M, Belblidia A. Feasibility of magnetic resonance imaging-guided focused ultrasound surgery as an adjunct to tamoxifen therapy in high-risk surgical patients with breast carcinoma. J Vasc Interv Radiol. 2003. 14:1275–1282.
Article8. Wu F, Wang ZB, Chen WZ, Bai J, Zhu H, Qiao TY. Preliminary experience using high intensity focused ultrasound for the treatment of patients with advanced stage renal malignancy. J Urol. 2003. 170:2237–2240.
Article9. Chen L, Rivens L, ter Haar G, Riddler S, Hill CR, Bensted JP. Histological changes in rat liver tumours treated with high-intensity focused ultrasound. Ultrasound Med Biol. 1993. 19:67–74.
Article10. ter Haar G, Clarke RL, Vaughan MG, Hill CR. Trackless surgery using focused ultrasound: technique and case report. Minimally invasive Therapy. 1991. 1:13–19.
Article11. Hill CR, ter Haar GR. High intensity focused ultrasound: potential for cancer treatment. Br J Radiol. 1995. 68:1296–1303.12. Wu F, Chen WZ, Bai j, Zou JZ, Wang ZL, Wang ZB, et al. Pathological changes in human malignant carcinoma treated with high-intensity focused ultrasound. Ultrasound Med Biol. 2001. 27:1099–1106.
Article13. Wu F, Wang ZB, Jin CB, Zhang JP, Chen WZ, Zou JZ, et al. Circulating tumor cells in patients with solid malignancy treated by high-intensity focused ultrasound. Ultrasound Med Biol. 2004. 30:511–517.
Article14. Vallejo R, Hord ED, Barna SA, Santiago-Palma J, Ahmed S. Perioperative immunosuppression in cancer patients. J Environ Pathol Toxicol Oncol. 2003. 22:139–146.
Article15. Mafune K, Tanaka Y. Influence of multimodality therapy on the cellular immunity of patients with esophageal cancer. Ann Surg Oncol. 2000. 7:609–616.
Article16. Kramer G, Steiner GE, Grobl M, Hrachowitz K, Reithmayr F, Marberger M, et al. Response to sublethal heat treatment of prostatic tumor cells and of prostatic tumor infiltrating T-cells. Prostate. 2004. 58:109–120.
Article17. Visioli AG, Rivens IH, ter Haar GR, Horwich A, Huddart RA, Glees J, et al. Preliminary results of a phase I dose escalation clinical trial using focused ultrasound in the treatment of localized tumours. Eur J Ultrasound. 1999. 9:11–18.
Article18. Vallancien G, Harouni M, Guillonneau B, Veillon B, Bougaran J. Ablation of superficial bladder tumors with focused extracorporeal pyrotherapy. Urology. 1996. 47:204–207.
Article19. Kennedy JE. High-intensity focused ultrasound in the treatment of solid tumors. Cancer. 2005. 5:321–327.20. Fry WJ, Mosberg WH, Bamard JW, Fry FJ. Production of focal destructive lesions in the central nervous system with ultrasound. J Neurosurg. 1954. 11:471–478.
Article21. Blana A, Walter B, Rogenhofer S, Wieland WF. High-intensity focused ultrasound for the treatment of localized prostate cancer: 5-year experience. Urology. 2004. 63:297–300.
Article22. Gelet A, Chapelon JY, Poissonnier L, Bouvier R, Rouviere O, Vallancien G, et al. Local recurrence of prostate cancer after external beam radiotherapy: early experience of salvage therapy using high-intensity focused ultrasonography. Urology. 2004. 63:625–629.
Article23. Stewart EA, Gedroyc WM, Tempany CM, Quade BJ, Inbar Y, Rabinovici J, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol. 2003. 189:48–54.
Article24. McDannold N, Moss M, Killiany R, Rosene DL, King RL, Hynynen K, et al. MRI-guided focused ultrasound surgery in the brain: tests in a primate model. Magn Reson Med. 2003. 49:1188–1191.
Article25. Wu F, Wang ZB, Cao YD, Chen WZ, Bai J, Zhu H, et al. A randomised clinical trial of high-intensity focused ultrasound ablation for the treatment of patients with localised breast cancer. Br J Cancer. 2003. 89:2227–2233.
Article26. Marbeger M, Schatzl G, Cranston D, Kennedy JE. Extracorporeal ablation of renal tumors with high intensity focused ultrasound. Br J Urol. 2005. 95:Suppl 2. 52–55.27. Wu F, Wang JB, Chen WZ, Zou JZ, Bai J, Su HB, et al. High intensity focused ultrasound ablation combined with transcatheter arterial embolisation in the treatment of advanced hepatocellular carcinoma. Radiology. 2005. 235:659–667.
Article28. Bohris C, Jenne JW, Rastert R, Simiantonakis I, Brix G, Debus J, et al. MR monitoring of focused ultrasound surgery in a breast tissue model in vivo. Magn Reson Imaging. 2001. 19:167–175.
Article29. Sedelaar JP, Aarnink RG, van Leenders GJ, Beerlage HP, Debruyne FM, de La Rosette JJ, et al. The application of three-dimensional contrast-enhanced ultrasound to measure volume of affected tissue after HIFU treatment for localized prostate cancer. Eur Urol. 2000. 37:559–568.
Article30. Anderson GS, Brinkmann F, Soulen MC, Alavi A, Zhuang H. FDG positron emission tomography in the surveillance of hepatic tumors treated with radiofrequency ablation. Clin Nucl Med. 2003. 28:192–197.
Article31. Cannon JW, Stroll JA, Salgo IS, Knowles HB, Howe RD, del Nido PJ, et al. Real-time three-dimensional ultrasound for guiding surgical tasks. Comput Aided Surg. 2003. 8:82–90.
Article32. Righetti R, Kallel F, Stafford RJ, Price RE, Krouskop TA, Ophir J, et al. Elastographic characterization of HIFU-induced lesions in canine livers. Ultrasound Med Biol. 1999. 25:1099–1113.
Article33. Penney GP, Blackall JM, Hamady MS, Sabharwal T, Adam A, Hawkes DJ. Registration of freehand 3D ultrasound and magnetic resonance liver images. Med Image Anal. 2004. 8:81–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High Intensity Focused Ultrasound Treatment-Induced Tumor Lysis Syndrome in Uterine Myoma Patient
- Current status of high-intensity focused ultrasound for the management of uterine adenomyosis
- Spontaneous Uterine Rupture during Second Trimester Pregnancy after High-intensity Focused Ultrasound
- Delayed intestinal perforation and vertebral osteomyelitis after high-intensity focused ultrasound treatment for uterine leiomyoma
- Enhanced Chemotherapeutic Drug Delivery to Tumor Tissue by High Intensity Focused Ultrasound