J Breast Cancer.
2011 Mar;14(1):58-63. 10.4048/jbc.2011.14.1.58.
Comparing Scalpel, Electrocautery and Ultrasonic Dissector Effects: The Impact on Wound Complications and Pro-Inflammatory Cytokine Levels in Wound Fluid from Mastectomy Patients
- Affiliations
-
- 1Department of General Surgery, Ankara Diskapi Training and Research Hospital, Ankara, Turkey. borakerim@yahoo.com
- 2Department of General Surgery, Ankara Oncology Training and Research Hospital, Ankara, Turkey.
- 3Department of Clinical Biochemistry, Gazi University, Ankara, Turkey.
- KMID: 2175644
- DOI: http://doi.org/10.4048/jbc.2011.14.1.58
Abstract
- PURPOSE
Introducing the relationship between the surgical instruments used in modified radical mastectomy and wound complications is important for preventing and decreasing complications. This prospective randomized trial was designed to assess the impact of scalpel, electrocautery, and ultrasonic dissector usage on wound complications and tissue damage.
METHODS
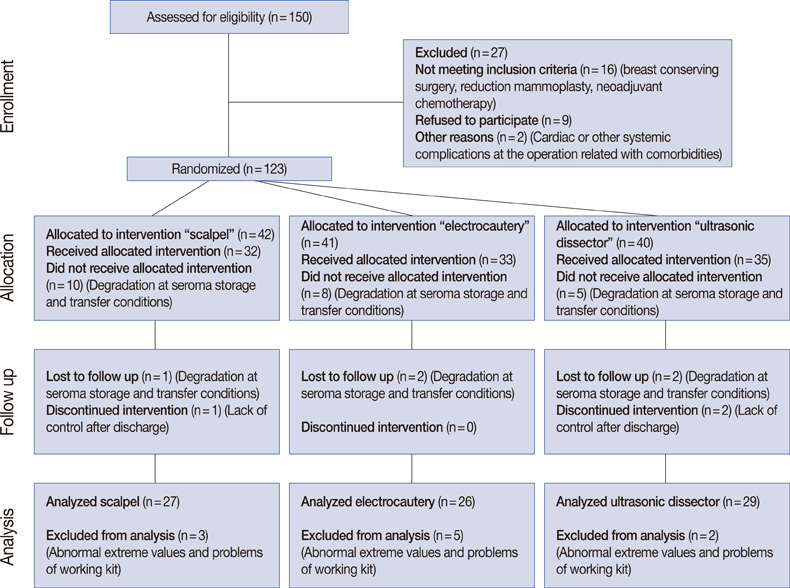
Eighty-two consecutive patients operated with mastectomy were studied. The postoperative time period needed for hemovac drainage, the amount and duration of seroma, infection, flap ecchymosis and necrosis rates were compared. Tumor necrosis factor alpha (TNF-alpha) and interleukin-6 (IL-6) levels in drainage fluids were determined to confirm the inflammatory response and tissue damage.
RESULTS
The numbers of patients included in the scalpel, electrocautery and ultrasonic dissector groups were 27, 26, and 29, respectively. The groups were homogenous with respect to age, body mass index, stage, cormorbidities, breast volume and flap area. Operation time and the amount of bleeding were statistically higher in the scalpel group. The incidence of seroma was higher in the electrocautery group and arm mobilization had to be delayed in this group. There were no differences between groups with respect to hematoma, infection, ecchymosis, necrosis, hemovac drainage and the total and first 3 days of seroma volume. TNF-alpha and IL-6 levels were significantly higher in samples obtained from the drains of patients operated with electrocautery.
CONCLUSION
Ultrasonic dissector decreases operation time by decreasing the amount of bleeding without increasing the seroma incidence. High cytokine levels in drainage fluids from patients operated with elecrocautery indicates that electrocautery induces more tissue damage and acute inflammatory response. Therefore, seroma, due to acute inflammatory response, was seen more frequently in the electrocautery group. Ultrasonic dissector coagulates protein by breaking hydrogen bonds which may close vascular and lymphatic channels more precisely. But, its actual preventive effect on seroma formation might be related to diminished inflammatory response.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Wound healing and postsurgical complications in breast cancer surgery: a comparison between PEAK PlasmaBlade and conventional electrosurgery – a preliminary report of a case series
Corrado Chiappa, Anna Fachinetti, Carlo Boeri, Veronica Arlant, Stefano Rausei, Gianlorenzo Dionigi, Francesca Rovera
Ann Surg Treat Res. 2018;95(3):129-134. doi: 10.4174/astr.2018.95.3.129.The Effect of Plasmakinetic Cautery on Wound Healing and Complications in Mastectomy
Lutfi Dogan, Mehmet Ali Gulcelik, Murat Yuksel, Osman Uyar, Osman Erdogan, Erhan Reis
J Breast Cancer. 2013;16(2):198-201. doi: 10.4048/jbc.2013.16.2.198.
Reference
-
1. Henry G, Garner WL. Inflammatory mediators in wound healing. Surg Clin North Am. 2003. 83:483–507.
Article2. Grellner W, Georg T, Wilske J. Quantitative analysis of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Sci Int. 2000. 113:251–264.
Article3. Shamley DR, Barker K, Simonite V, Beardshaw A. Delayed versus immediate exercises following surgery for breast cancer: a systematic review. Breast Cancer Res Treat. 2005. 90:263–271.
Article4. Coveney EC, O'Dwyer PJ, Geraghty JG, O'Higgins NJ. Effect of closing dead space on seroma formation after mastectomy-a prospective randomized clinical trial. Eur J Surg Oncol. 1993. 19:143–146.5. Kuroi K, Shimozuma K, Taguchi T, Imai H, Yamashiro H, Ohsumi S, et al. Pathophysiology of seroma in breast cancer. Breast Cancer. 2005. 12:288–293.
Article6. Watt-Boolsen S, Nielsen VB, Jensen J, Bak S. Postmastectomy seroma. A study of the nature and origin of seroma after mastectomy. Dan Med Bull. 1989. 36:487–489.7. Wu FP, Hoekman K, Meijer S, Cuesta MA. VEGF and endostatin levels in wound fluid and plasma after breast surgery. Angiogenesis. 2003. 6:255–257.
Article8. Hoefer RA Jr, DuBois JJ, Ostrow LB, Silver LF. Wound complications following modified radical mastectomy: an analysis of perioperative factors. J Am Osteopath Assoc. 1990. 90:47–53.
Article9. Miller E, Paull DE, Morrissey K, Cortese A, Nowak E. Scalpel versus electrocautery in modified radical mastectomy. Am Surg. 1988. 54:284–286.10. Gelman CL, Barroso EG, Britton CT, Haklin MF, Staren ED. The effect of lasers, electrocautery, and sharp dissection on cutaneous flaps. Plast Reconstr Surg. 1994. 94:829–833.
Article11. Lumachi F, Brandes AA, Burelli P, Basso SM, Iacobone M, Ermani M. Seroma prevention following axillary dissection in patients with breast cancer by using ultrasound scissors: a prospective clinical study. Eur J Surg Oncol. 2004. 30:526–530.
Article12. Galatius H, Okholm M, Hoffmann J. Mastectomy using ultrasonic dissection: effect on seroma formation. Breast. 2003. 12:338–341.
Article13. Deo SV, Shukla NK, Asthana S, Niranjan B, Srinivas G. A comparative study of modified radical mastectomy using harmonic scalpel and electrocautery. Singapore Med J. 2002. 43:226–228.14. Adwani A, Ebbs SR. Ultracision reduces acute blood loss but not seroma formation after mastectomy and axillary dissection: a pilot study. Int J Clin Pract. 2006. 60:562–564.
Article15. Sanguinetti A, Docimo G, Ragusa M, Calzolari F, D'Ajello F, Ruggiero R, et al. Ultrasound scissors versus electrocautery in axillary dissection: our experience. G Chir. 2010. 31:151–153.16. Bennett NT, Schultz GS. Growth factors and wound healing: biochemical properties of growth factors and their receptors. Am J Surg. 1993. 165:728–737.
Article17. Gailit J, Clark RA. Wound repair in the context of extracellular matrix. Curr Opin Cell Biol. 1994. 6:717–725.
Article18. Lin E, Calvano SE, Lowry SF. Inflammatory cytokines and cell response in surgery. Surgery. 2000. 127:117–126.
Article19. Gallucci RM, Simeonova PP, Matheson JM, Kommineni C, Guriel JL, Sugawara T, et al. Impaired cutaneous wound healing in interleukin-6-deficient and immunosuppressed mice. FASEB J. 2000. 14:2525–2531.
Article20. Schmidt A, Bengtsson A, Tylman M, Blomqvist L. Pro-inflammatory cytokines in elective flap surgery. J Surg Res. 2007. 137:117–121.
Article21. Loo WT, Sasano H, Chow LW. Pro-inflammatory cytokine, matrix metalloproteinases and TIMP-1 are involved in wound healing after mastectomy in invasive breast cancer patients. Biomed Pharmacother. 2007. 61:548–552.
Article22. Reber PU, Andren-Sandberg A, Schmied B, Büchler MW. Cytokines in surgical trauma: cholecystectomy as an example. Dig Surg. 1998. 15:92–101.
Article23. Reith HB, Kaman S, Mittelkötter O, Kilic Y, Kozuschek W. Cytokine activation in patients undergoing open or laparoscopic cholecystectomy. Int Surg. 1997. 82:389–393.24. Kristiansson M, Saraste L, Soop M, Sundqvist KG, Thörne A. Diminished interleukin-6 and C-reactive protein responses to laparoscopic versus open cholecystectomy. Acta Anaesthesiol Scand. 1999. 43:146–152.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Plasmakinetic Cautery on Wound Healing and Complications in Mastectomy
- The effects of scalpel, harmonic scalpel and monopolar electrocautery on the healing of colonic anastomosis after colonic resection
- Clinical Trial Comparing Pain and Clinical Function after Conventional Semi-open Milligan Hemorrhoidectomy vs Open Ultrasonic Dissector Hemorrhoidectomy
- Ultrasonic dissection versus electrocautery for immediate prosthetic breast reconstruction
- Comparison of a Hemorrhoidectomy With Ultrasonic Scalpel Versus a Conventional Hemorrhoidectomy