Chonnam Med J.
2013 Apr;49(1):27-30. 10.4068/cmj.2013.49.1.27.
Impact of Physician's Education on Adherence to Tuberculosis Treatment for Patients of Low Socioeconomic Status in Bangladesh
- Affiliations
-
- 1Department of Medicine, Bangladesh-Korea Friendship Hospital, Savar, Bangladesh. haroc153@naver.com
- 2Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Medical Education, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2172173
- DOI: http://doi.org/10.4068/cmj.2013.49.1.27
Abstract
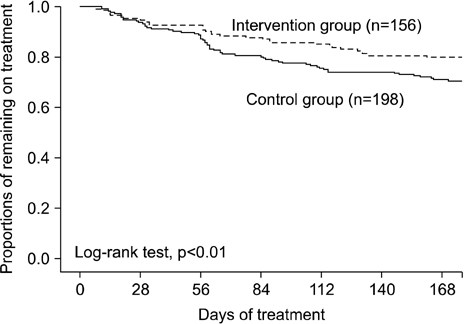
- Successful tuberculosis control depends on good adherence to treatment. Yet, limited data are available on the efficacy of methods for improving the adherence of patients of low socioeconomic status. We evaluated the impact of physician-provided patient education on adherence to anti-tuberculosis medication in a low socioeconomic status and resource-limited setting. A pre-/post-intervention study was conducted at a suburban primary health care clinic in Bangladesh where an intensive education strategy was established in May 2006. Treatment outcomes of tuberculosis patients from March 2005 to April 2006 (pre-intervention) and from May 2006 to December 2007 (post-intervention) were compared. Among 354 patients, 198 (56%) were treated before intervention and 156 (44%) were treated after intervention. Cumulative adherence to anti-tuberculosis medication was significantly greater in the intervention group than in the control group in univariate and multivariate analyses. Physician's education can contribute to increasing the adherence of patients in resource-limited settings.
Keyword
MeSH Terms
Figure
Reference
-
1. Arora VK, Sarin R, Lönnroth K. Feasibility and effectiveness of a public-private mix project for improved TB control in Delhi, India. Int J Tuberc Lung Dis. 2003. 7:1131–1138.2. World Health Organization. The Stop TB Strategy: Building on and Enhancing DOTS to Meet the TB-related Millennium Development Goals. 2006. Geneva: World Health Organization.3. Quy HT, Lönnroth K, Lan NT, Buu TN. Treatment results among tuberculosis patients treated by private lung specialists involved in a public-private mix project in Vietnam. Int J Tuberc Lung Dis. 2003. 7:1139–1146.4. Liefooghe R, Suetens C, Meulemans H, Moran MB, De Muynck A. A randomised trial of the impact of counselling on treatment adherence of tuberculosis patients in Sialkot, Pakistan. Int J Tuberc Lung Dis. 1999. 3:1073–1080.5. Morisky DE, Malotte CK, Choi P, Davidson P, Rigler S, Sugland B, et al. A patient education program to improve adherence rates with antituberculosis drug regimens. Health Educ Q. 1990. 17:253–267.
Article6. Thiam S, LeFevre AM, Hane F, Ndiaye A, Ba F, Fielding KL, et al. Effectiveness of a strategy to improve adherence to tuberculosis treatment in a resource-poor setting: a cluster randomized controlled trial. JAMA. 2007. 297:380–386.
Article7. Volmink J, Garner P. Systematic review of randomised controlled trials of strategies to promote adherence to tuberculosis treatment. BMJ. 1997. 315:1403–1406.
Article8. World Health Organization. Global Tuberculosis Control 2009: Epidemiology, Strategy, Financing. 2009. Geneva: World Health Organization.9. Menzies R, Rocher I, Vissandjee B. Factors associated with compliance in treatment of tuberculosis. Tuber Lung Dis. 1993. 74:32–37.
Article10. Hill PC, Stevens W, Hill S, Bah J, Donkor SA, Jallow A, et al. Risk factors for defaulting from tuberculosis treatment: a prospective cohort study of 301 cases in the Gambia. Int J Tuberc Lung Dis. 2005. 9:1349–1354.11. Khan MA, Walley JD, Witter SN, Imran A, Safdar N. Costs and cost-effectiveness of different DOT strategies for the treatment of tuberculosis in Pakistan. Directly observed treatment. Health Policy Plan. 2002. 17:178–186.
Article12. Hane F, Thiam S, Fall AS, Vidal L, Diop AH, Ndir M, et al. Identifying barriers to effective tuberculosis control in Senegal: an anthropological approach. Int J Tuberc Lung Dis. 2007. 11:539–543.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study of relationships among tuberculosis knowledge, family support, and medication adherence in tuberculosis patients
- Relationship between Knowledge and Adherence to Self-management Guidelines, and Influencing Factors of Adherence for Hemodialysis Patients
- Predictors of Adherence with Positive Airway Pressure Treatment in Patients with Obstructive Sleep Apnea in Korean
- The Association between Socioeconomic Status and Adherence to Health Check-up in Korean Adults, Based on the 2010–2012 Korean National Health and Nutrition Examination Survey
- Influence of Social Support and Negative Emotional Status on Self-care Adherence in Symptomatic Patients with Heart Failure