Ann Dermatol.
2014 Apr;26(2):162-171. 10.5021/ad.2014.26.2.162.
A Clinicopathologic Study of Thirty Cases of Acquired Perforating Dermatosis in Korea
- Affiliations
-
- 1Department of Dermatology, Eulji General Hospital, Eulji University, Seoul, Korea. dermahan@gmail.com
- 2Department of Dermatology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2171650
- DOI: http://doi.org/10.5021/ad.2014.26.2.162
Abstract
- BACKGROUND
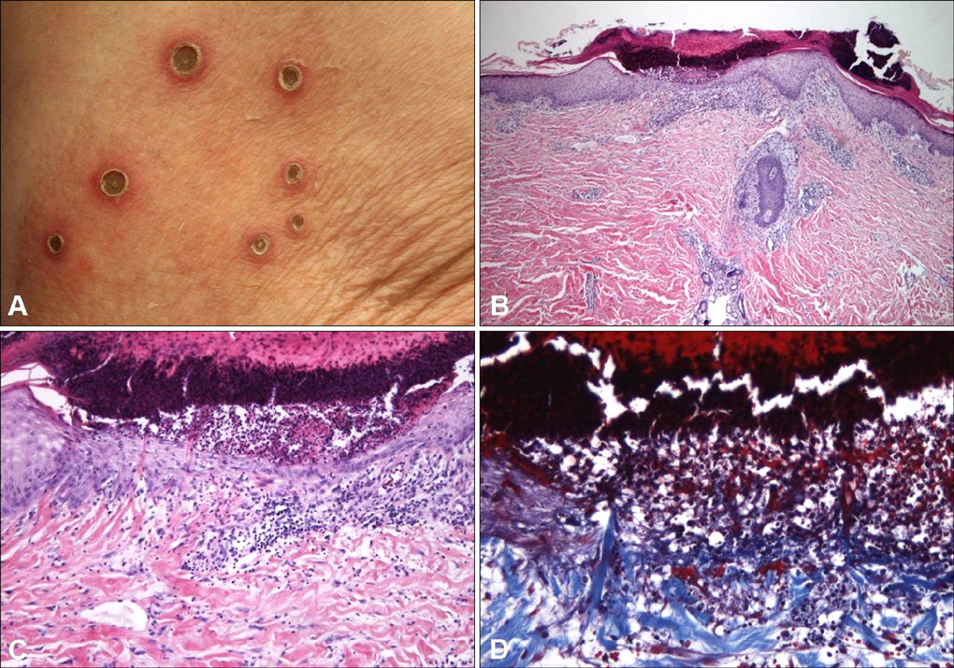
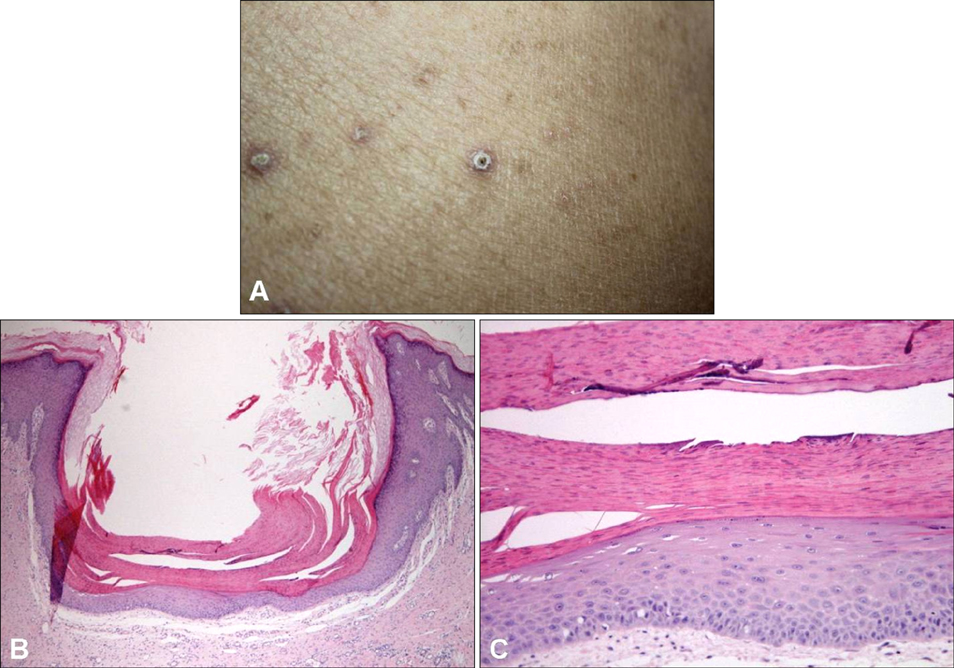
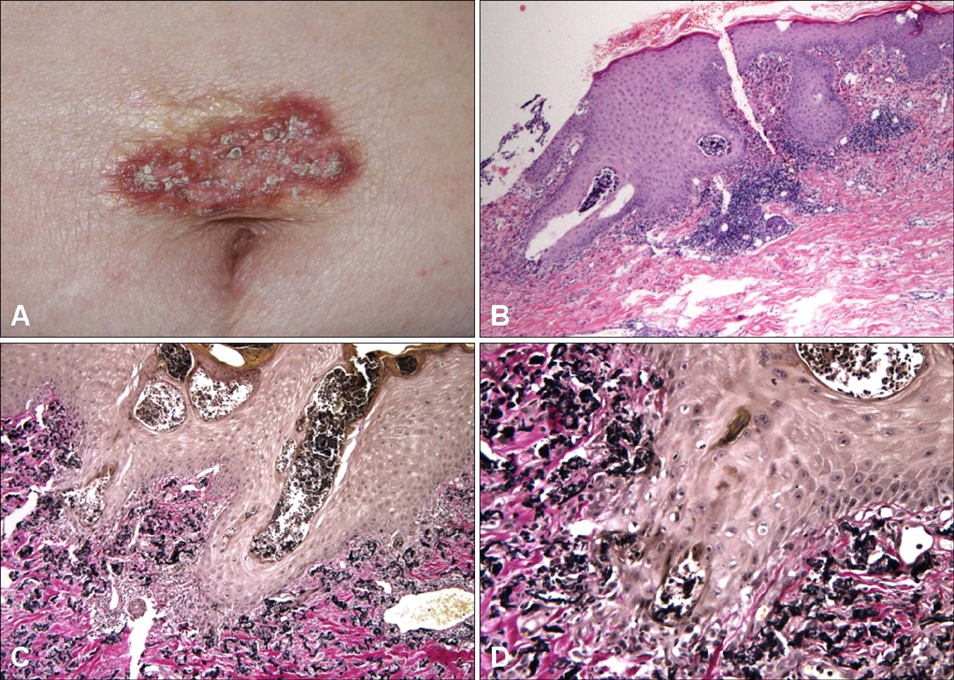
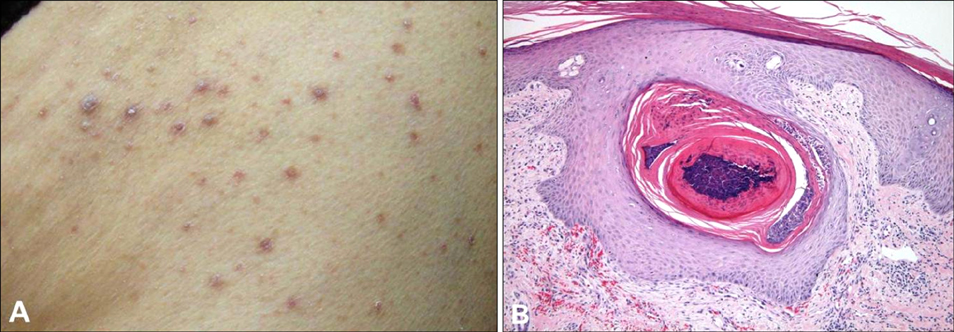
Acquired perforating dermatosis (APD) is histopathologically characterized by transepidermal elimination of materials from the upper dermis. APD can be divided into four diseases: Kyrle's disease, perforating folliculitis, elastosis perforans serpiginosa, and reactive perforating collagenosis. APD is usually associated with systemic diseases, especially diabetes mellitus or chronic renal failure. So far, there have only been a few Korean studies of APD, which have a limited number of patients.
OBJECTIVE
The aim of this study is to evaluate the clinical and histopathologic characteristics of 30 cases of APD and to examine the association with systemic diseases.
METHODS
We retrospectively reviewed the medical records and biopsy specimens of 30 patients who were diagnosed with APD.
RESULTS
The mean age was 55.5 years, and the average duration of the lesion was 7.8 months. The lower extremities (73.3%) were the most frequently occurring sites of the lesion. Twenty-five patients (83.3%) had pruritus, and Koebner's phenomenon was present in 11 patients. Patients of 63.3% had at least one systemic disease. Diabetes mellitus (n=17, 56.7%) and chronic renal failure (n=10, 33.3%) were the most commonly associated conditions. Most patients received topical steroids (93.3%) and antihistamines (80.0%). The most common histopathologic type was reactive perforating collagenosis (n=23, 73.3%).
CONCLUSION
In this study, most patients had a systemic association to the diseases. Therefore, we suggest that further evaluation is necessary for patients who present with APD. This includes reviewing patient's comprehensive past medical history, clinical exam, and additional diagnostic testing to check for the possibility of associated systemic diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Miller MK, Friedman RJ, Naik NS, Heilman ER, Nousari CH. Degenerative diseases and perforating disorders. In : Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2009. p. 391–396.2. Poliak SC, Lebwohl MG, Parris A, Prioleau PG. Reactive perforating collagenosis associated with diabetes mellitus. N Engl J Med. 1982; 306:81–84.
Article3. Cochran RJ, Tucker SB, Wilkin JK. Reactive perforating collagenosis of diabetes mellitus and renal failure. Cutis. 1983; 31:55–58.4. Iyoda M, Hayashi F, Kuroki A, Shibata T, Kitazawa K, Sugisaki T, et al. Acquired reactive perforating collagenosis in a nondiabetic hemodialysis patient: successful treatment with allopurinol. Am J Kidney Dis. 2003; 42:E11–E13.
Article5. Faver IR, Daoud MS, Su WP. Acquired reactive perforating collagenosis. Report of six cases and review of the literature. J Am Acad Dermatol. 1994; 30:575–580.6. Kiliç A, Gönül M, Cakmak SK, Gül U, Demiriz M. Acquired reactive perforating collagenosis as a presenting sign of hepatocellular carcinoma. Eur J Dermatol. 2006; 16:447.7. Eigentler TK, Metzler G, Brossart P, Fierlbeck G. Acquired perforating collagenosis in Hodgkin's disease. J Am Acad Dermatol. 2005; 52:922.
Article8. Karpouzis A, Tsatalas C, Sivridis E, Kotsianidis I, Margaritis D, Kouskoukis C, et al. Acquired reactive perforating collagenosis associated with myelodysplastic syndrome evolving to acute myelogenous leukaemia. Australas J Dermatol. 2004; 45:78–79.
Article9. Bank DE, Cohen PR, Kohn SR. Reactive perforating collagenosis in a setting of double disaster: acquired immunodeficiency syndrome and end-stage renal disease. J Am Acad Dermatol. 1989; 21:371–374.
Article10. Zelger B, Hintner H, Auböck J, Fritsch PO. Acquired perforating dermatosis. Transepidermal elimination of DNA material and possible role of leukocytes in pathogenesis. Arch Dermatol. 1991; 127:695–700.
Article11. Kim JH, Kang WH. Acquired reactive perforating collagenosis in a diabetic patient with pulmonary aspergillosis. Cutis. 2000; 66:425–430.12. Thiele-Ochel S, Schneider LA, Reinhold K, Hunzelmann N, Krieg T, Scharffetter-Kochanek K. Acquired perforating collagenosis: is it due to damage by scratching? Br J Dermatol. 2001; 145:173–174.
Article13. Hinrichs W, Breuckmann F, Altmeyer P, Kreuter A. Acquired perforating dermatosis: a report on 4 cases associated with scabies infection. J Am Acad Dermatol. 2004; 51:665–667.
Article14. Healy R, Cerio R, Hollingsworth A, Bewley A. Acquired perforating dermatosis associated with pregnancy. Clin Exp Dermatol. 2010; 35:621–623.
Article15. Rapini RP, Herbert AA, Drucker CR. Acquired perforating dermatosis. Evidence for combined transepidermal elimination of both collagen and elastic fibers. Arch Dermatol. 1989; 125:1074–1078.
Article16. Alyahya GA, Heegaard S, Prause JU. Ocular changes in a case of Kyrle's disease. 20-year follow-up. Acta Ophthalmol Scand. 2000; 78:585–558.
Article17. Saray Y, Seçkin D, Bilezikçi B. Acquired perforating dermatosis: clinicopathological features in twenty-two cases. J Eur Acad Dermatol Venereol. 2006; 20:679–688.
Article18. Hong SB, Park JH, Ihm CG, Kim NI. Acquired perforating dermatosis in patients with chronic renal failure and diabetes mellitus. J Korean Med Sci. 2004; 19:283–288.
Article19. Satti MB, Aref AH, Raddadi AA, Al-Ghamdi FA. Acquired reactive perforating collagenosis: a clinicopathologic study of 15 cases from Saudi Arabia. J Eur Acad Dermatol Venereol. 2010; 24:223–227.
Article20. Mehregan AH, Schwartz OD, Livingood CS. Reactive perforating collagenosis. Arch Dermatol. 1967; 96:277–282.
Article21. Morton CA, Henderson IS, Jones MC, Lowe JG. Acquired perforating dermatosis in a British dialysis population. Br J Dermatol. 1996; 135:671–677.
Article22. Minocha JS, Schlosser BJ. Acquired perforating disorders. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill Medical;2012. p. 727–773.23. Cohen RW, Auerbach R. Acquired reactive perforating collagenosis. J Am Acad Dermatol. 1989; 20:287–289.
Article24. Hood AF, Hardegen GL, Zarate AR, Nigra TP, Gelfand MC. Kyrle's disease in patients with chronic renal failure. Arch Dermatol. 1982; 118:85–88.
Article25. Stone RA. Kyrle-like lesions in two patients with renal failure undergoing dialysis. J Am Acad Dermatol. 1981; 5:707–709.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Acquired Perforating Dermatosis in Chronic Renal Failure with Allopurinol
- A Case of Acquired Perforating Dermatosis Associated with Hepatocellular Carcinoma and Diabetic Nephropathy
- Acquired Perforating Dermatosis in Renal Failure
- A Giant Variant of Acquired Perforating Collagenosis in Chronic Renal Failure
- Crusted Scabies Misdiagnosed as a Cutaneous Side Reaction due to Allopurinol in a Patient with Acquired Perforating Dermatosis