Ann Dermatol.
2015 Aug;27(4):423-430. 10.5021/ad.2015.27.4.423.
Vitamin D as a Marker for Disease Severity in Chronic Urticaria and Its Possible Role in Pathogenesis
- Affiliations
-
- 1Department of Dermatology, Eulji University School of Medicine, Daejeon, Korea. sun_lee@eulji.ac.kr
- KMID: 2171500
- DOI: http://doi.org/10.5021/ad.2015.27.4.423
Abstract
- BACKGROUND
Chronic urticaria is defined as repeated episodes of wheals lasting for 6 weeks or longer. Nowadays, the role of vitamin D in various chronic diseases is a matter of great interest, but limited data is available on the vitamin D status in patients with chronic urticaria.
OBJECTIVE
The goal of this study was to investigate the relationship between vitamin D status and clinical characteristics of chronic urticaria.
METHODS
The clinical records of 72 patients with chronic urticaria, 26 with acute urticaria and 26 with atopic dermatitis, along with 72 healthy controls, were retrospectively reviewed.
RESULTS
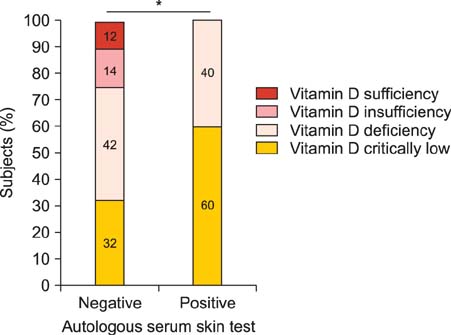
The serum 25-(OH)D3 level was found to be significantly reduced in patients with chronic urticaria compared to those in the other groups. In particular, the proportion of patients with critically low vitamin D levels (<10 ng/ml) was significantly higher in the chronic urticaria group than in the other groups. The serum vitamin D levels showed significant negative associations with urticaria activity score and disease duration. In addition, serum vitamin D levels were significantly lower in subjects with a positive autologous serum skin test than in subjects with a negative result.
CONCLUSION
In conclusion, the serum vitamin D level was more likely to be critically low in patients with chronic urticaria, and an inverse relationship with disease severity and disease duration was observed. These findings may open up the possibility of the clinical use of vitamin D as a contributing factor in the pathogenesis of chronic urticaria and a predictive marker for disease activity in chronic urticaria.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Autologous serum and plasma skin test to predict 2-year outcome in chronic spontaneous urticaria
Tadech Boonpiyathad, Atik Sangasapaviliya
Asia Pac Allergy. 2016;6(4):226-235. doi: 10.5415/apallergy.2016.6.4.226.Prevalence and Risk Factors of Urticaria With a Focus on Chronic Urticaria in Children
Seung Jin Lee, Eun Kyo Ha, Hye Mi Jee, Kyung Suk Lee, Seung Won Lee, Mi Ae Kim, Dong Hyun Kim, Young-Ho Jung, Youn Ho Sheen, Myong Soon Sung, Man Yong Han
Allergy Asthma Immunol Res. 2017;9(3):212-219. doi: 10.4168/aair.2017.9.3.212.
Reference
-
1. Sachdeva S, Gupta V, Amin SS, Tahseen M. Chronic urticaria. Indian J Dermatol. 2011; 56:622–628.
Article2. Powell RJ, Du Toit GL, Siddique N, Leech SC, Dixon TA, Clark AT, et al. British Society for Allergy and Clinical Immunology (BSACI). BSACI guidelines for the management of chronic urticaria and angio-oedema. Clin Exp Allergy. 2007; 37:631–650.
Article3. Greaves MW. Chronic urticaria. N Engl J Med. 1995; 332:1767–1772.
Article4. Gaig P, Olona M, Muñoz Lejarazu D, Caballero MT, Domínguez FJ, Echechipia S, et al. Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol. 2004; 14:214–220.5. Khan DA. Chronic urticaria: diagnosis and management. Allergy Asthma Proc. 2008; 29:439–446.
Article6. Sánchez-Borges M, Asero R, Ansotegui IJ, Baiardini I, Bernstein JA, Canonica GW, et al. WAO Scientific and Clinical Issues Council. Diagnosis and treatment of urticaria and angioedema: a worldwide perspective. World Allergy Organ J. 2012; 5:125–147.
Article7. Kaplan AP, Greaves M. Pathogenesis of chronic urticaria. Clin Exp Allergy. 2009; 39:777–787.
Article8. Sabroe RA, Francis DM, Barr RM, Black AK, Greaves MW. Anti-Fc(episilon)RI auto antibodies and basophil histamine releasability in chronic idiopathic urticaria. J Allergy Clin Immunol. 1998; 102:651–658.
Article9. Futata E, Azor M, Dos Santos J, Maruta C, Sotto M, Guedes F, et al. Impaired IFN-α secretion by plasmacytoid dendritic cells induced by TLR9 activation in chronic idiopathic urticaria. Br J Dermatol. 2011; 164:1271–1279.
Article10. Dos Santos JC, Azor MH, Nojima VY, Lourenço FD, Prearo E, Maruta CW, et al. Increased circulating pro-inflammatory cytokines and imbalanced regulatory T-cell cytokines production in chronic idiopathic urticaria. Int Immunopharmacol. 2008; 8:1433–1440.
Article11. Santos JC, de Brito CA, Futata EA, Azor MH, Orii NM, Maruta CW, et al. Up-regulation of chemokine C-C ligand 2 (CCL2) and C-X-C chemokine 8 (CXCL8) expression by monocytes in chronic idiopathic urticaria. Clin Exp Immunol. 2012; 167:129–136.
Article12. Dickie LJ, Church LD, Coulthard LR, Mathews RJ, Emery P, McDermott MF. Vitamin D3 down-regulates intracellular Toll-like receptor 9 expression and Toll-like receptor 9-induced IL-6 production in human monocytes. Rheumatology (Oxford). 2010; 49:1466–1471.
Article13. Kasperska-Zajac A, Sztylc J, Machura E, Jop G. Plasma IL-6 concentration correlates with clinical disease activity and serum C-reactive protein concentration in chronic urticaria patients. Clin Exp Allergy. 2011; 41:1386–1391.
Article14. Hide M, Francis DM, Grattan CE, Hakimi J, Kochan JP, Greaves MW. Autoantibodies against the high-affinity IgE receptor as a cause of histamine release in chronic urticaria. N Engl J Med. 1993; 328:1599–1604.
Article15. Jain S. Pathogenesis of chronic urticaria: an overview. Dermatol Res Pract. 2014; 2014:674709.
Article16. Piemonti L, Monti P, Sironi M, Fraticelli P, Leone BE, Dal Cin E, et al. Vitamin D3 affects differentiation, maturation, and function of human monocyte-derived dendritic cells. J Immunol. 2000; 164:4443–4451.
Article17. Holick MF. Vitamin D deficiency. N Engl J Med. 2007; 357:266–281.
Article18. Brehm JM, Celedón JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E, et al. Serum vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med. 2009; 179:765–771.
Article19. Vähävihu K, Ala-Houhala M, Peric M, Karisola P, Kautiainen H, Hasan T, et al. Narrowband ultraviolet B treatment improves vitamin D balance and alters antimicrobial peptide expression in skin lesions of psoriasis and atopic dermatitis. Br J Dermatol. 2010; 163:321–328.
Article20. Amestejani M, Salehi BS, Vasigh M, Sobhkhiz A, Karami M, Alinia H, et al. Vitamin D supplementation in the treatment of atopic dermatitis: a clinical trial study. J Drugs Dermatol. 2012; 11:327–330.21. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau A, et al. Dermatology Section of the European Academy of Allergology and Clinical Immunology. Global Allergy and Asthma European Network. European Dermatology Forum. World Allergy Organization. EAACI/GA(2)LEN/EDF/WAO guideline: definition, classification and diagnosis of urticaria. Allergy. 2009; 64:1417–1426.
Article22. Kamen DL, Cooper GS, Bouali H, Shaftman SR, Hollis BW, Gilkeson GS. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev. 2006; 5:114–117.
Article23. Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010; 30:397–409.
Article24. Peroni DG, Piacentini GL, Cametti E, Chinellato I, Boner AL. Correlation between serum 25-hydroxyvitamin D levels and severity of atopic dermatitis in children. Br J Dermatol. 2011; 164:1078–1082.
Article25. Thorp WA, Goldner W, Meza J, Poole JA. Reduced vitamin D levels in adult subjects with chronic urticaria. J Allergy Clin Immunol. 2010; 126:413. author reply 413-414.
Article26. Chandrashekar L, Rajappa M, Munisamy M, Ananthanarayanan PH, Thappa DM, Arumugam B. 25-Hydroxy vitamin D levels in chronic urticaria and its correlation with disease severity from a tertiary care centre in South India. Clin Chem Lab Med. 2014; 52:e115–e118.
Article27. Grzanka A, Machura E, Mazur B, Misiolek M, Jochem J, Kasperski J, et al. Relationship between vitamin D status and the inflammatory state in patients with chronic spontaneous urticaria. J Inflamm (Lond). 2014; 11:2.
Article28. Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea--a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab. 2011; 96:643–651.
Article29. Waldron JL, Ashby HL, Cornes MP, Bechervaise J, Razavi C, Thomas OL, et al. Vitamin D: a negative acute phase reactant. J Clin Pathol. 2013; 66:620–622.
Article30. Sindher SB, Jariwala S, Gilbert J, Rosenstreich D. Resolution of chronic urticaria coincident with vitamin D supplementation. Ann Allergy Asthma Immunol. 2012; 109:359–360.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vitamin D Status and Its Relationship with Disease Severity/activity in Patients with Atopic Dermatitis, Psoriasis, and Chronic Idiopathic Urticaria in Korea
- Allergen sensitization and vitamin D status in young Korean children with urticaria
- A Study on Clinical and Etiological Aspects of Chronic Urticaria by Questionnaire
- Dermographism ( III ): Dermographism in Acute and Chronic Urticaria
- Clinical Predictors of Disease Progression in New-Onset Urticaria