Allergy Asthma Respir Dis.
2015 May;3(3):194-199. 10.4168/aard.2015.3.3.194.
Food-dependent exercise-induced anaphylaxis in Korean children: a single-center retrospective case study
- Affiliations
-
- 1Department of Pediatrics, Childhood Asthma Atopy Center, Research Center for Standardization of Allergic Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sjhong@amc.seoul.kr
- 2Division of Allergy and Clinical Immunology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2168489
- DOI: http://doi.org/10.4168/aard.2015.3.3.194
Abstract
- PURPOSE
Food-dependent exercise-induced anaphylaxis (FDEIA) is a specific clinical syndrome requiring both ingestion of an allergenic food and exercise to induce anaphylaxis. It may be underdiagnosed due to insufficient history taking in terms of the causes of anaphylaxis. This study aims to describe clinical characteristics and diagnostic results of FDEIA in children.
METHODS
We retrospectively reviewed the medical records of patients under 18 years old who were diagnosed with FDEIA at Asan Medical Center between January 2003 and August 2014.
RESULTS
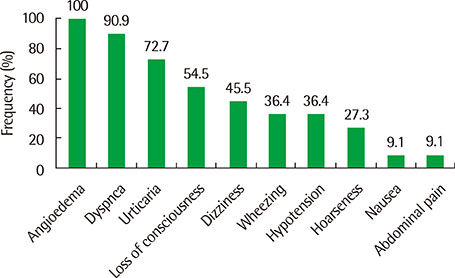
Of the 170 children with anaphylaxis, 11 (6.5%) had FDEIA. The mean age at the onset of symptoms was 14.8+/-1.5 years. The causative foods were: wheat (n=4), meat (n=1), mung beans (n=1), rice (n=1), celery (n=1), cabbage (n=1), fish (n=1), and soy (n=1). The numbers of symptom development were: 7 (n=1), 6 (n=1), 3 (n=4), 2 (n=2), and 1 (n=3). The geometric mean (range of 1 standard deviation) of total serum IgE levels was 131.6 kU/L (53.5-324.2 kU/L). The skin prick test and immununoCAP were positive for causative foods in 3 of 6 patients (50.0%) and 7 of 10 patients (70.0%), respectively. The provocation test was performed in 8 of 11 patients and showed positive results except 1 patient. The interval between exercise and symptoms was 21.6+/-7.3 minutes.
CONCLUSION
It is important to suspect FDEIA and take a detailed history in children with anaphylaxis. Provocation test should be considered to confirm the diagnosis. Further studies on disease course and long-term prognosis are warranted.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The past, present, and future of research on anaphylaxis in Korean children
Sooyoung Lee
Allergy Asthma Respir Dis. 2018;6(Suppl 1):S21-S30. doi: 10.4168/aard.2018.6.S1.S21.
Reference
-
1. Simons FE, Ardusso LR, Dimov V, Ebisawa M, El-Gamal YM, Lockey RF, et al. World Allergy Organization Anaphylaxis Guidelines: 2013 update of the evidence base. Int Arch Allergy Immunol. 2013; 162:193–204.
Article2. Morita E, Kunie K, Matsuo H. Food-dependent exercise-induced anaphylaxis. J Dermatol Sci. 2007; 47:109–117.
Article3. Tanaka S. An epidemiological survey on food-dependent exercise-induced anaphylaxis in kindergartners, schoolchildren and junior high school students. Asia Pac J Public Health. 1994; 7:26–30.
Article4. Aihara Y, Takahashi Y, Kotoyori T, Mitsuda T, Ito R, Aihara M, et al. Frequency of food-dependent, exercise-induced anaphylaxis in Japanese junior-high-school students. J Allergy Clin Immunol. 2001; 108:1035–1039.
Article5. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36.
Article6. Im JH, Kwon HY, Ye YM, Park HS, Kim TB, Choi GS, et al. Food-dependent exercise-induced anaphylaxis in Korea: a multicenter retrospective case study. Allergy Asthma Respir Dis. 2013; 1:203–210.
Article7. Lee HB, Ahn IS, Choi JH, Park CW. A case of wheat-dependent exercise-induced anaphylaxis. Ann Dermatol. 2009; 21:447–449.
Article8. Jo EJ, Yang MS, Kim YJ, Kim HS, Kim MY, Kim SH, et al. Food-dependent exercise-induced anaphylaxis occurred only in a warm but not in a cold environment. Asia Pac Allergy. 2012; 2:161–164.
Article9. Pang SJ, No SJ, Kim DW, Lee SM, Lee EJ, Kim CH, et al. A case report of food-dependent exercise-induced anaphylaxis in a patient who was sensitive to pork. Pediatr Allergy Respir Dis. 2012; 22:116–121.
Article10. Simons FE, Ardusso LR, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World allergy organization guidelines for the assessment and management of anaphylaxis. World Allergy Organ J. 2011; 4:13–37.
Article11. Romano A, Di Fonso M, Giuffreda F, Papa G, Artesani MC, Viola M, et al. Food-dependent exercise-induced anaphylaxis: clinical and laboratory findings in 54 subjects. Int Arch Allergy Immunol. 2001; 125:264–272.
Article12. Watanabe T, Sakamoto Y, Tomonaga H, Inuyama M, Sasayama H, Hara K, et al. A case of food-dependent exercise-induced anaphylaxis. Arerugi. 1990; 39:1523–1528.13. Barg W, Medrala W, Wolanczyk-Medrala A. Exercise-induced anaphylaxis: an update on diagnosis and treatment. Curr Allergy Asthma Rep. 2011; 11:45–51.
Article14. Kim JH, Lee JI, Yang BY, Ahn SJ, Park SJ, Kim SY, Lee GJ. A case of food-dependent exercise-induced anaphylaxis developed only in winter. Korean J Med. 2005; 69:331–334.15. Robson-Ansley P, Toit GD. Pathophysiology, diagnosis and management of exercise-induced anaphylaxis. Curr Opin Allergy Clin Immunol. 2010; 10:312–317.
Article16. Palosuo K, Varjonen E, Nurkkala J, Kalkkinen N, Harvima R, Reunala T, et al. Transglutaminase-mediated cross-linking of a peptic fraction of omega-5 gliadin enhances IgE reactivity in wheat-dependent, exercise-induced anaphylaxis. J Allergy Clin Immunol. 2003; 111:1386–1392.
Article17. Matsuo H, Morimoto K, Akaki T, Kaneko S, Kusatake K, Kuroda T, et al. Exercise and aspirin increase levels of circulating gliadin peptides in patients with wheat-dependent exercise-induced anaphylaxis. Clin Exp Allergy. 2005; 35:461–466.
Article18. Kozai H, Yano H, Matsuda T, Kato Y. Wheat-dependent exercise-induced anaphylaxis in mice is caused by gliadin and glutenin treatments. Immunol Lett. 2006; 102:83–90.
Article19. Morita E, Chinuki Y, Takahashi H. Recent advances of in vitro tests for the diagnosis of food-dependent exercise-induced anaphylaxis. J Dermatol Sci. 2013; 71:155–159.
Article20. Pacharn P, Jirapongsananuruk O, Daengsuwan T, Vichyanond P, Visitsunthorn N. Wheat-dependent, exercise-induced anaphylaxis in Thai children: a report of 5 cases. Asian Pac J Allergy Immunol. 2009; 27:115–120.21. Dohi M, Suko M, Sugiyama H, Yamashita N, Tadokoro K, Juji F, et al. Food-dependent, exercise-induced anaphylaxis: a study on 11 Japanese cases. J Allergy Clin Immunol. 1991; 87(1 Pt 1):34–40.
Article22. Romano A, Di Fonso M, Giuffreda F, Quaratino D, Papa G, Palmieri V, et al. Diagnostic work-up for food-dependent, exercise-induced anaphylaxis. Allergy. 1995; 50:817–824.
Article23. Jacquenet S, Morisset M, Battais F, Denery-Papini S, Croizier A, Baudouin E, et al. Interest of ImmunoCAP system to recombinant omega-5 gliadin for the diagnosis of exercise-induced wheat allergy. Int Arch Allergy Immunol. 2009; 149:74–80.
Article24. Matsuo H, Dahlstrom J, Tanaka A, Kohno K, Takahashi H, Furumura M, et al. Sensitivity and specificity of recombinant omega-5 gliadin-specific IgE measurement for the diagnosis of wheat-dependent exercise-induced anaphylaxis. Allergy. 2008; 63:233–236.
Article25. Park HJ, Kim JH, Kim JE, Jin HJ, Choi GS, Ye YM, et al. Diagnostic value of the serum-specific IgE ratio of ω-5 gliadin to wheat in adult patients with wheat-induced anaphylaxis. Int Arch Allergy Immunol. 2012; 157:147–150.
Article26. Chong SU, Worm M, Zuberbier T. Role of adverse reactions to food in urticaria and exercise-induced anaphylaxis. Int Arch Allergy Immunol. 2002; 129:19–26.
Article27. Tewari A, Du Toit G, Lack G. The difficulties of diagnosing food-dependent exercise-induced anaphylaxis in childhood: a case study and review. Pediatr Allergy Immunol. 2006; 17:157–160.
Article28. Noimark L, Wales J, Du Toit G, Pastacaldi C, Haddad D, Gardner J, et al. The use of adrenaline autoinjectors by children and teenagers. Clin Exp Allergy. 2012; 42:284–292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Food allergies and food-induced anaphylaxis: role of cofactors
- A Case of Wheat-Dependent Exercise-Induced Anaphylaxis
- Wheat-dependent, Exercise-induced Anaphylaxis: A Successful Case of Prevention with Ketotifen
- Three Cases of Food-dependent Exercise-induced Anaphylaxis
- A case of food-dependent exercise-induced anaphylaxis developed only in winter