Imaging Sci Dent.
2013 Sep;43(3):145-151. 10.5624/isd.2013.43.3.145.
Radiopacity of restorative composites by conventional radiograph and digital images with different resolutions
- Affiliations
-
- 1Graduate Program in Dentistry, Federal University of Pelotas, Pelotas, Brazil. raquelvenancio@hotmail.com
- 2Department of Operative Dentistry, Federal University of Paraiba, Pelotas, Brazil.
- KMID: 2167451
- DOI: http://doi.org/10.5624/isd.2013.43.3.145
Abstract
- PURPOSE
This study was performed to evaluate and compare the radiopacity of dentin, enamel, and 8 restorative composites on conventional radiograph and digital images with different resolutions.
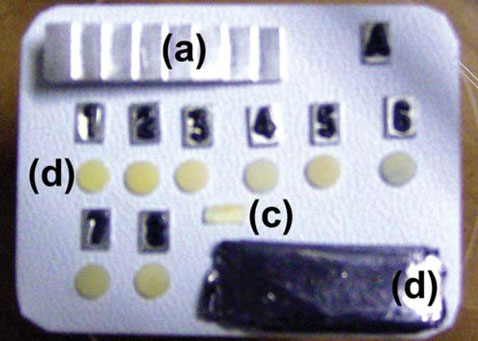
MATERIALS AND METHODS
Specimens were fabricated from 8 materials and human molars were longitudinally sectioned 1.0 mm thick to include both enamel and dentin. The specimens and tooth sections were imaged by conventional radiograph using #4 sized intraoral film and digital images were taken in high speed and high resolution modes using a phosphor storage plate. Densitometric evaluation of the enamel, dentin, restorative materials, a lead sheet, and an aluminum step wedge was performed on the radiographic images. For the evaluation, the Al equivalent (mm) for each material was calculated. The data were analyzed using one-way ANOVA and Tukey's test (p<0.05), considering the material factor and then the radiographic method factor, individually.
RESULTS
The high speed mode allowed the highest radiopacity, while the high resolution mode generated the lowest values. Furthermore, the high resolution mode was the most efficient method for radiographic differentiation between restorative composites and dentin. The conventional radiograph was the most effective in enabling differentiation between enamel and composites. The high speed mode was the least effective in enabling radiographic differentiation between the dental tissues and restorative composites.
CONCLUSION
The high speed mode of digital imaging was not effective for differentiation between enamel and composites. This made it less effective than the high resolution mode and conventional radiographs. All of the composites evaluated showed radiopacity values that fit the ISO 4049 recommendations.
Keyword
MeSH Terms
Figure
Reference
-
1. Rasimick BJ, Gu S, Deutsch AS, Musikant BL. Measuring the radiopacity of luting cements, dowels, and core build-up materials with a digital radiography system using a CCD sensor. J Prosthodont. 2007; 16:357–364.
Article2. Attar N, Tam LE, McComb D. Flow, strength, stiffness and radiopacity of flowable resin composites. J Can Dent Assoc. 2003; 69:516–521.3. Tsuge T. Radiopacity of conventional, resin-modified glass ionomer, and resin-based luting materials. J Oral Sci. 2009; 51:223–230.
Article4. Tagger M, Katz A. Radiopacity of endodontic sealers: development of a new method for direct measurement. J Endod. 2003; 29:751–755.
Article5. Sabbagh J, Vreven J, Leloup G. Radiopacity of resin-based materials measured in film radiographs and storage phosphor plate (Digora). Oper Dent. 2004; 29:677–684.6. Wadhwani C, Hess T, Faber T, Piñeyro A, Chen CS. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010; 103:295–302.
Article7. Dukic W, Delija B, Derossi D, Dadic I. Radiopacity of composite dental materials using a digital X-ray system. Dent Mater J. 2012; 31:47–53.
Article8. Nomoto R, Mishima A, Kobayashi K, McCabe JF, Darvell BW, Watts DC, et al. Quantitative determination of radio-opacity: equivalence of digital and film X-ray systems. Dent Mater. 2008; 24:141–147.
Article9. Zdesar U, Fortuna T, Valantic B, Skrk D. Is digital better in dental radiography? Radiat Prot Dosimetry. 2008; 129:138–139.
Article10. Oliveira AE, de Almeida SM, Paganini GA, Haiter Neto F, Bóscolo FN. Comparative study of two digital radiographic storage phosphor systems. Braz Dent J. 2000; 11:111–116.11. International Organization for Standardization. ISO 4049: 2009. Dentistry-Polymer based restorative materials. 4th ed. Geneva: ISO;2009.12. Tanomaru-Filho M, Laitano SC, Gonçalves M, Tanomaru JM. Evaluation of the radiopacity of root-end filling materials by digitization of radiographic images. Braz J Oral Sci. 2006; 5:1018–1021.13. Ergücü Z, Türkün LS, Onem E, Güneri P. Comparative radiopacity of six flowable resin composites. Oper Dent. 2010; 35:436–440.
Article14. The desirability of using radiopaque plastics in dentistry: a status report. Council on Dental Materials, Instruments, and Equipment. J Am Dent Assoc. 1981; 102:347–349.15. Imperiano MT, Khoury HJ, Pontual ML, Montes MA, Silveira MM. Comparative radiopacity of four low-viscosity composites. Braz J Oral Sci. 2007; 6:1278–1282.16. Poorsattar Bejeh Mir A, Poorsattar Bejeh Mir M. Assessment of radiopacity of restorative composite resins with various target distances and exposure times and a modified aluminum step wedge. Imaging Sci Dent. 2012; 42:163–167.
Article17. Murchison DF, Charlton DG, Moore WS. Comparative radiopacity of flowable resin composites. Quintessence Int. 1999; 30:179–184.18. Lopes SL, Cruz AD, Ferreira RI, Bóscolo FN, Almeida SM. Image quality in partially erased DenOptix storage phosphor plates. Braz Oral Res. 2008; 22:78–83.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the radiopacity of restorative materials with different structures and thicknesses using a digital radiography system
- How does duration of curing affect the radiopacity of dental materials?
- Digital contrast subtraction radiography for proximal caries diagnosis
- Color Stability of Bulk-Fill Resin Composites after Immersion in Different Media
- Comparative study of the radiopacity of resin cements used in aesthetic dentistry