J Korean Med Sci.
2015 Aug;30(8):1175-1182. 10.3346/jkms.2015.30.8.1175.
Analysis of Predisposing Factors for Hearing Loss in Adults
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Anyang, Korea. hjk1000@hallym.ac.kr
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Kyungpook National University College of Medicine, Daegu, Korea.
- 3Department of Statistics, Hallym University, Chuncheon, Korea.
- KMID: 2164514
- DOI: http://doi.org/10.3346/jkms.2015.30.8.1175
Abstract
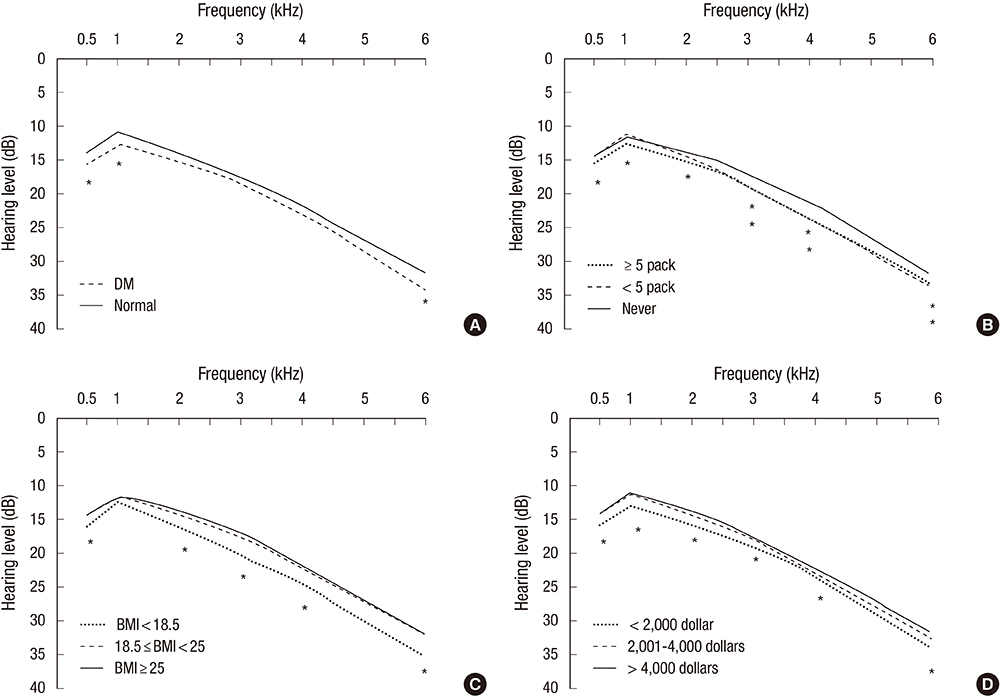
- We aimed to estimate the effects of various risk factors on hearing level in Korean adults, using data from the Korea National Health and Nutrition Examination Survey. We examined data from 13,369 participants collected between 2009 and 2011. Average hearing thresholds at low (0.5, 1, and 2 kHz) and high frequencies (3, 4, and 6 kHz), were investigated in accordance with various known risk factors via multiple regression analysis featuring complex sampling. We additionally evaluated data from 4,810 participants who completed a questionnaire concerned with different types of noise exposure. Low body mass index, absence of hyperlipidemia, history of diabetes mellitus, low incomes, low educational status, and smoking were associated with elevated low frequency hearing thresholds. In addition, male sex, low body mass index, absence of hyperlipidemia, low income, low educational status, smoking, and heavy alcohol consumption were associated with elevated high frequency hearing thresholds. Participants with a history of earphone use in noisy circumstances demonstrated hearing thresholds which were 1.024 dB (95% CI: 0.176 to 1.871; P = 0.018) higher, at low-frequencies, compared to participants without a history of earphone use. Our study suggests that low BMI, absence of hyperlipidemia, low household income, and low educational status are related with hearing loss in Korean adults. Male sex, smoking, and heavy alcohol use are related with high frequency hearing loss. A history of earphone use in noisy circumstances is also related with hearing loss.
Keyword
MeSH Terms
-
Adult
Alcohol Drinking/*epidemiology
Causality
Comorbidity
Diabetes Mellitus
Disease Susceptibility
Educational Status
Employment/statistics & numerical data
Female
Hearing Loss/*diagnosis/*epidemiology
Hearing Tests/statistics & numerical data
Humans
Income/statistics & numerical data
Male
*Noise
Occupational Exposure/*statistics & numerical data
Republic of Korea/epidemiology
Risk Factors
Sex Distribution
Smoking/*epidemiology
Surveys and Questionnaires
Figure
Cited by 1 articles
-
Hearing Impairment Increases Economic Inequality
So Young Kim, Chanyang Min, Dae Myoung Yoo, Jiwon Chang, Hyo-Jeong Lee, Bumjung Park, Hyo Geun Choi
Clin Exp Otorhinolaryngol. 2021;14(3):278-286. doi: 10.21053/ceo.2021.00325.
Reference
-
1. Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, Nondahl DM. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. Am J Epidemiol. 1998; 148:879–886.2. Wallhagen MI, Strawbridge WJ, Cohen RD, Kaplan GA. An increasing prevalence of hearing impairment and associated risk factors over three decades of the Alameda County Study. Am J Public Health. 1997; 87:440–442.3. Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003; 43:661–668.4. Ebert DA, Heckerling PS. Communication with deaf patients. Knowledge, beliefs, and practices of physicians. JAMA. 1995; 273:227–229.5. Gates GA, Cobb JL, D'Agostino RB, Wolf PA. The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch Otolaryngol Head Neck Surg. 1993; 119:156–161.6. Barnett S, Franks P. Deafness and mortality: analyses of linked data from the National Health Interview Survey and National Death Index. Public Health Rep. 1999; 114:330–336.7. Cruickshanks KJ, Klein R, Klein BE, Wiley TL, Nondahl DM, Tweed TS. Cigarette smoking and hearing loss: the epidemiology of hearing loss study. JAMA. 1998; 279:1715–1719.8. Fransen E, Topsakal V, Hendrickx JJ, Van Laer L, Huyghe JR, Van Eyken E, Lemkens N, Hannula S, Mäki-Torkko E, Jensen M, et al. Occupational noise, smoking, and a high body mass index are risk factors for age-related hearing impairment and moderate alcohol consumption is protective: a European population-based multicenter study. J Assoc Res Otolaryngol. 2008; 9:264–276. discussion 1-39. Kakarlapudi V, Sawyer R, Staecker H. The effect of diabetes on sensorineural hearing loss. Otol Neurotol. 2003; 24:382–386.10. Díaz de León-Morales LV, Jáuregui-Renaud K, Garay-Sevilla ME, Hernández-Prado J, Malacara-Hernández JM. Auditory impairment in patients with type 2 diabetes mellitus. Arch Med Res. 2005; 36:507–510.11. Gopinath B, Flood VM, McMahon CM, Burlutsky G, Smith W, Mitchell P. The effects of smoking and alcohol consumption on age-related hearing loss: the Blue Mountains Hearing Study. Ear Hear. 2010; 31:277–282.12. Lalwani AK, Katz K, Liu YH, Kim S, Weitzman M. Obesity is associated with sensorineural hearing loss in adolescents. Laryngoscope. 2013; 123:3178–3184.13. Mościcki EK, Elkins EF, Baum HM, McNamara PM. Hearing loss in the elderly: an epidemiologic study of the Framingham Heart Study Cohort. Ear Hear. 1985; 6:184–190.14. Siegelaub AB, Friedman GD, Adour K, Seltzer CC. Hearing loss in adults: relation to age, sex, exposure to loud noise, and cigarette smoking. Arch Environ Health. 1974; 29:107–109.15. Rosen S, Olin P. Hearing loss and coronary heart disease. Arch Otolaryngol. 1965; 82:236–243.16. Shargorodsky J, Curhan SG, Eavey R, Curhan GC. A prospective study of cardiovascular risk factors and incident hearing loss in men. Laryngoscope. 2010; 120:1887–1891.17. Thakur JS, Mohindroo NK, Vasanthalakshmi MS, Kashyap N, Azad RK, Sharma DR. Auditory brainstem evoked responses in hyperlipidaemia: effect of various lipid fractions on auditory function. J Laryngol Otol. 2012; 126:249–256.18. Karlidağ T, Açik Y, Kaygusuz I, Yalçin S, Güngör MY, Demirbağ E. The effect of hyperlipidemia on hearing function. Kulak Burun Bogaz Ihtis Derg. 2002; 9:112–116.19. Friedrich G, Pilger E. Lipoproteins in cochleovestibular disorders (author's transl). Arch Otorhinolaryngol. 1981; 232:101–105.20. Kojima Y, Ito S, Furuya N. Hearing improvement after therapy for hyperlipidemia in patients with chronic-phase sudden deafness. Ann Otol Rhinol Laryngol. 2001; 110:105–108.21. Hirano K, Ikeda K, Kawase T, Oshima T, Kekehata S, Takahashi S, Sato T, Kobayashi T, Takasaka T. Prognosis of sudden deafness with special reference to risk factors of microvascular pathology. Auris Nasus Larynx. 1999; 26:111–115.22. Hwang JH, Wu CC, Hsu CJ, Liu TC, Yang WS. Association of central obesity with the severity and audiometric configurations of age-related hearing impairment. Obesity (Silver Spring). 2009; 17:1796–1801.23. Lasisi AO, Fehintola FA, Yusuf OB. Age-related hearing loss, vitamin B12, and folate in the elderly. Otolaryngol Head Neck Surg. 2010; 143:826–830.24. Gopinath B, Flood VM, McMahon CM, Burlutsky G, Spankovich C, Hood LJ, Mitchell P. Dietary antioxidant intake is associated with the prevalence but not incidence of age-related hearing loss. J Nutr Health Aging. 2011; 15:896–900.25. Rosenhall U, Sixt E, Sundh V, Svanborg A. Correlations between presbyacusis and extrinsic noxious factors. Audiology. 1993; 32:234–243.26. Sunkum AJ, Pingile S. A clinical study of audiological profile in diabetes mellitus patients. Eur Arch Otorhinolaryngol. 2013; 270:875–879.27. Parving A, Elberling C, Balle V, Parbo J, Dejgaard A, Parving HH. Hearing disorders in patients with insulin-dependent diabetes mellitus. Audiology. 1990; 29:113–121.28. Bainbridge KE, Hoffman HJ, Cowie CC. Diabetes and hearing impairment in the United States: audiometric evidence from the National Health and Nutrition Examination Survey, 1999 to 2004. Ann Intern Med. 2008; 149:1–10.29. Tay HL, Ray N, Ohri R, Frootko NJ. Diabetes mellitus and hearing loss. Clin Otolaryngol Allied Sci. 1995; 20:130–134.30. Fukushima H, Cureoglu S, Schachern PA, Kusunoki T, Oktay MF, Fukushima N, Paparella MM, Harada T. Cochlear changes in patients with type 1 diabetes mellitus. Otolaryngol Head Neck Surg. 2005; 133:100–106.31. Fukushima H, Cureoglu S, Schachern PA, Paparella MM, Harada T, Oktay MF. Effects of type 2 diabetes mellitus on cochlear structure in humans. Arch Otolaryngol Head Neck Surg. 2006; 132:934–938.32. Sung JH, Sim CS, Lee CR, Yoo CI, Lee H, Kim Y, Lee J. Relationship of cigarette smoking and hearing loss in workers exposed to occupational noise. Ann Occup Environ Med. 2013; 25:8.33. Nakanishi N, Okamoto M, Nakamura K, Suzuki K, Tatara K. Cigarette smoking and risk for hearing impairment: a longitudinal study in Japanese male office workers. J Occup Environ Med. 2000; 42:1045–1049.34. Pouryaghoub G, Mehrdad R, Mohammadi S. Interaction of smoking and occupational noise exposure on hearing loss: a cross-sectional study. BMC Public Health. 2007; 7:137.35. Browning GG, Gatehouse S, Lowe GD. Blood viscosity as a factor in sensorineural hearing impairment. Lancet. 1986; 1:121–123.36. Kim MG, Hong SM, Shim HJ, Kim YD, Cha CI, Yeo SG. Hearing threshold of Korean adolescents associated with the use of personal music players. Yonsei Med J. 2009; 50:771–776.37. Fausti SA, Erickson DA, Frey RH, Rappaport BZ, Schechter MA. The effects of noise upon human hearing sensitivity from 8000 to 20 000 Hz. J Acoust Soc Am. 1981; 69:1343–1347.38. Breinbauer HA, Anabalón JL, Gutierrez D, Cárcamo R, Olivares C, Caro J. Output capabilities of personal music players and assessment of preferred listening levels of test subjects: outlining recommendations for preventing music-induced hearing loss. Laryngoscope. 2012; 122:2549–2556.39. Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009; 30:139–145.40. Bainbridge KE, Hoffman HJ, Cowie CC. Risk factors for hearing impairment among U.S. adults with diabetes: National Health and Nutrition Examination Survey 1999-2004. Diabetes Care. 2011; 34:1540–1545.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined effect of anemia and chronic rhinitis on hearing loss in Korean adults: a nationwide observational study
- Association Between Hearing Level and Mental Health and Quality of Life in Adults Aged >40 Years
- Influence of Cochlear Implantation on Cognitive Function in Elderly Patients
- Rehabilitation of Age-Related Hearing Loss Patients
- The Study of High Frequence Hearing Loss in Pilots