J Gynecol Oncol.
2015 Apr;26(2):90-99. 10.3802/jgo.2015.26.2.90.
Efficacy and oncologic safety of nerve-sparing radical hysterectomy for cervical cancer: a randomized controlled trial
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea.
- 2Center for Uterine Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea. parksang@ncc.re.kr
- 3Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Department of Urology, Center for Prostate Cancer, National Cancer Center, Goyang, Korea.
- 5Department of Pathology, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2160791
- DOI: http://doi.org/10.3802/jgo.2015.26.2.90
Abstract
OBJECTIVE
A prospective, randomized controlled trial was conducted to evaluate the efficacy of nerve-sparing radical hysterectomy (NSRH) in preserving bladder function and its oncologic safety in the treatment of cervical cancer.
METHODS
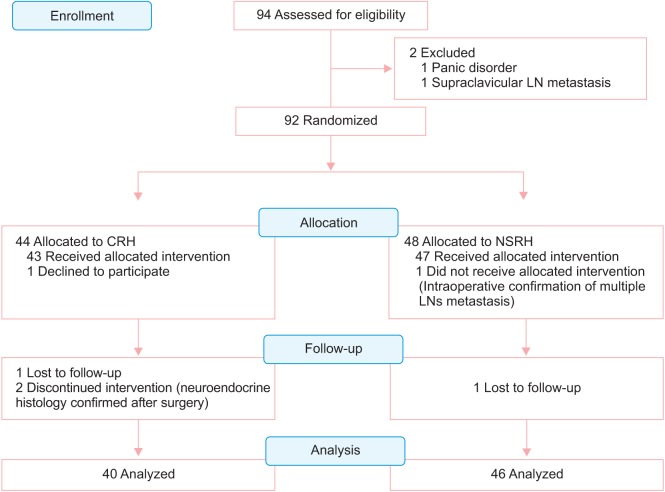
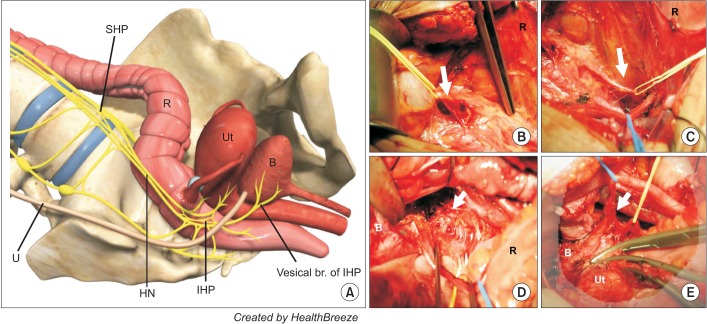
From March 2003 to November 2005, 92 patients with cervical cancer stage IA2 to IIA were randomly assigned for surgical treatment with conventional radical hysterectomy (CRH) or NSRH, and 86 patients finally included in the analysis. Adequacy of nerve sparing, radicality, bladder function, and oncologic safety were assessed by quantifying the nerve fibers in the paracervix, measuring the extent of paracervix and harvested lymph nodes (LNs), urodynamic study (UDS) with International Prostate Symptom Score (IPSS), and 10-year disease-free survival (DFS), respectively.
RESULTS
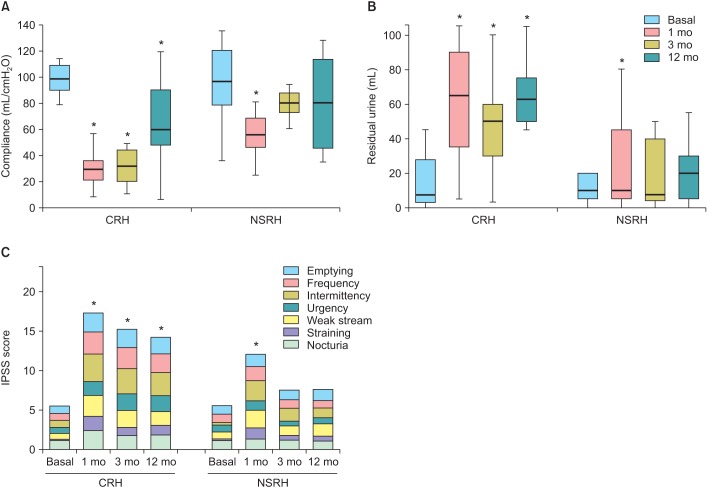
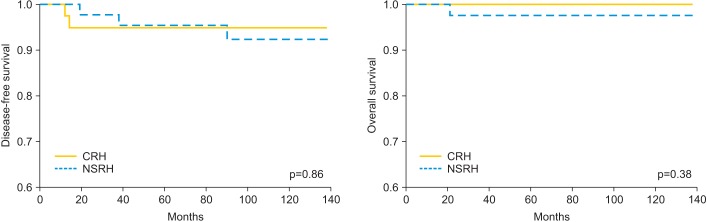
There were no differences in clinicopathologic characteristics between two groups. The median number of nerve fiber was 12 (range, 6 to 21) and 30 (range, 17 to 45) in the NSRH and CRH, respectively (p<0.001). The extent of resected paracervix and number of LNs were not different between the two groups. Volume of residual urine and bladder compliance were significantly deteriorated at 12 months after CRH. On the contrary, all parameters of UDS were recovered no later than 3 months after NSRH. Evaluation of the IPSS showed that the frequency of long-term urinary symptom was higher in CRH than in the NSRH group. The median duration before the postvoid residual urine volume became less than 50 mL was 11 days (range, 7 to 26 days) in NSRH group and was 18 days (range, 10 to 85 days) in CRH group (p<0.001). No significant difference was observed in the 10-year DFS between two groups.
CONCLUSION
NSRH appears to be effective in preserving bladder function without sacrificing oncologic safety.
Keyword
MeSH Terms
-
Adenocarcinoma/mortality/pathology/surgery
Adult
Carcinoma, Adenosquamous/mortality/pathology/surgery
Carcinoma, Squamous Cell/mortality/pathology/surgery
Female
Humans
Hysterectomy/adverse effects/*methods
Middle Aged
*Organ Sparing Treatments/adverse effects/methods
Pelvis/*innervation/surgery
Recovery of Function
Survival Analysis
Treatment Outcome
Urinary Bladder/*innervation/physiology/surgery
Uterine Cervical Neoplasms/mortality/pathology/*surgery
Uterus/*innervation/surgery
Figure
Cited by 2 articles
-
Factors associated with parametrial involvement in patients with stage IB1 cervical cancer: Who is suitable for less radical surgery?
Seung-Ho Lee, Kyoung-Joo Cho, Mi-Hyang Ko, Hyun-Yee Cho, Kwang-Beom Lee, Soyi Lim
Obstet Gynecol Sci. 2018;61(1):88-94. doi: 10.5468/ogs.2018.61.1.88.Oncologic effectiveness of nerve-sparing radical hysterectomy in cervical cancer
Antonino Ditto, Giorgio Bogani, Umberto Leone Roberti Maggiore, Fabio Martinelli, Valentina Chiappa, Carlos Lopez, Stefania Perotto, Domenica Lorusso, Francesco Raspagliesi
J Gynecol Oncol. 2018;29(3):. doi: 10.3802/jgo.2018.29.e41.
Reference
-
1. Donato DM. Surgical management of stage IB-IIA cervical carcinoma. Semin Surg Oncol. 1999; 16:232–235. PMID: 10225301.
Article2. Zullo MA, Manci N, Angioli R, Muzii L, Panici PB. Vesical dysfunctions after radical hysterectomy for cervical cancer: a critical review. Crit Rev Oncol Hematol. 2003; 48:287–293. PMID: 14693341.
Article3. Ercoli A, Delmas V, Gadonneix P, Fanfani F, Villet R, Paparella P, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the risk of injury to the autonomous pelvic nerves. Surg Radiol Anat. 2003; 25:200–206. PMID: 12910382.
Article4. Maas CP, Trimbos JB, DeRuiter MC, van de Velde CJ, Kenter GG. Nerve sparing radical hysterectomy: latest developments and historical perspective. Crit Rev Oncol Hematol. 2003; 48:271–279. PMID: 14693339.
Article5. Landoni F, Maneo A, Cormio G, Perego P, Milani R, Caruso O, et al. Class II versus class III radical hysterectomy in stage IB-IIA cervical cancer: a prospective randomized study. Gynecol Oncol. 2001; 80:3–12. PMID: 11136561.
Article6. Hockel M, Konerding MA, Heussel CP. Liposuction-assisted nerve-sparing extended radical hysterectomy: oncologic rationale, surgical anatomy, and feasibility study. Am J Obstet Gynecol. 1998; 178:971–976. PMID: 9609569.7. Possover M, Stober S, Plaul K, Schneider A. Identification and preservation of the motoric innervation of the bladder in radical hysterectomy type III. Gynecol Oncol. 2000; 79:154–157. PMID: 11063637.
Article8. Trimbos JB, Maas CP, Deruiter MC, Peters AA, Kenter GG. A nerve-sparing radical hysterectomy: guidelines and feasibility in Western patients. Int J Gynecol Cancer. 2001; 11:180–186. PMID: 11437922.
Article9. Yabuki Y, Asamoto A, Hoshiba T, Nishimoto H, Nishikawa Y, Nakajima T. Radical hysterectomy: an anatomic evaluation of parametrial dissection. Gynecol Oncol. 2000; 77:155–163. PMID: 10739705.
Article10. Chen C, Li W, Li F, Liu P, Zhou J, Lu L, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the nerve trauma in cardinal ligament. Gynecol Oncol. 2012; 125:245–251. PMID: 22209773.
Article11. Wu J, Liu X, Hua K, Hu C, Chen X, Lu X. Effect of nerve-sparing radical hysterectomy on bladder function recovery and quality of life in patients with cervical carcinoma. Int J Gynecol Cancer. 2010; 20:905–909. PMID: 20606542.
Article12. Chen L, Zhang WN, Zhang SM, Yang ZH, Zhang P. Effect of laparoscopic nerve-sparing radical hysterectomy on bladder function, intestinal function recovery and quality of sexual life in patients with cervical carcinoma. Asian Pac J Cancer Prev. 2014; 15:10971–10975. PMID: 25605211.
Article13. Hockel M, Horn LC, Hentschel B, Hockel S, Naumann G. Total mesometrial resection: high resolution nerve-sparing radical hysterectomy based on developmentally defined surgical anatomy. Int J Gynecol Cancer. 2003; 13:791–803. PMID: 14675316.
Article14. Possover M. Technical modification of the nerve-sparing laparoscopy-assisted vaginal radical hysterectomy type 3 for better reproducibility of this procedure. Gynecol Oncol. 2003; 90:245–247. PMID: 12893183.
Article15. Scotti RJ, Bergman A, Bhatia NN, Ostergard DR. Urodynamic changes in urethrovesical function after radical hysterectomy. Obstet Gynecol. 1986; 68:111–120. PMID: 3725241.16. Fishman IJ, Shabsigh R, Kaplan AL. Lower urinary tract dysfunction after radical hysterectomy for carcinoma of cervix. Urology. 1986; 28:462–468. PMID: 3787918.
Article17. Raspagliesi F, Ditto A, Fontanelli R, Solima E, Hanozet F, Zanaboni F, et al. Nerve-sparing radical hysterectomy: a surgical technique for preserving the autonomic hypogastric nerve. Gynecol Oncol. 2004; 93:307–314. PMID: 15099938.
Article18. Fujii S, Takakura K, Matsumura N, Higuchi T, Yura S, Mandai M, et al. Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol Oncol. 2007; 107:4–13. PMID: 17905140.
Article19. Charoenkwan K, Srisomboon J, Suprasert P, Tantipalakorn C, Kietpeerakool C. Nerve-sparing class III radical hysterectomy: a modified technique to spare the pelvic autonomic nerves without compromising radicality. Int J Gynecol Cancer. 2006; 16:1705–1712. PMID: 16884390.
Article20. Katahira A, Niikura H, Kaiho Y, Nakagawa H, Kurokawa K, Arai Y, et al. Intraoperative electrical stimulation of the pelvic splanchnic nerves during nerve-sparing radical hysterectomy. Gynecol Oncol. 2005; 98:462–466. PMID: 15979695.
Article21. Lin LY, Wu JH, Yang CW, Sheu BC, Lin HH. Impact of radical hysterectomy for cervical cancer on urodynamic findings. Int Urogynecol J Pelvic Floor Dysfunct. 2004; 15:418–421. PMID: 15549261.
Article22. Kanao H, Fujiwara K, Ebisawa K, Hada T, Ota Y, Andou M. Various types of total laparoscopic nerve-sparing radical hysterectomies and their effects on bladder function. J Gynecol Oncol. 2014; 25:198–205. PMID: 25045432.
Article23. Ralph G, Tamussino K, Lichtenegger W. Urological complications after radical abdominal hysterectomy for cervical cancer. Baillieres Clin Obstet Gynaecol. 1988; 2:943–952. PMID: 3229062.24. Todo Y, Kuwabara M, Watari H, Ebina Y, Takeda M, Kudo M, et al. Urodynamic study on postsurgical bladder function in cervical cancer treated with systematic nerve-sparing radical hysterectomy. Int J Gynecol Cancer. 2006; 16:369–375. PMID: 16445660.
Article25. Plotti F, Zullo MA, Montera R, Angioli R, Pierluigi BP. Bladder function after laparoscopic nerve-sparing radical hysterectomy. Gynecol Oncol. 2011; 120:315. PMID: 21129769.
Article26. Long Y, Yao DS, Pan XW, Ou TY. Clinical efficacy and safety of nerve-sparing radical hysterectomy for cervical cancer: a systematic review and meta-analysis. PLoS One. 2014; 9:e94116. PMID: 24748015.
Article27. Basaran D, Dusek L, Majek O, Cibula D. Oncological outcomes of nerve-sparing radical hysterectomy for cervical cancer: a systematic review. Ann Surg Oncol. 2015; 1. 23. http://dx.doi.org/10.1245/s10434-015-4377-7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improved bladder function in radical hysterectomy without worsening oncologic outcome: resection of the posterior layer of the vesicouterine ligament with the procedure limited to the vesical veins
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- Impact of peritoneal vaginoplasty combined with radical hysterectomy on the quality of sexual life for patients with early-stage cervical cancer: trial protocol for a multi-center superiority randomized controlled trial
- Minimally invasive surgery improves short-term outcomes of nerve-sparing radical hysterectomy in patients with cervical cancer: a propensity-matched analysis with open abdominal surgery
- Nerve-sparing radical hysterectomy: time for a new standard of care for cervical cancer?