J Korean Med Sci.
2012 Nov;27(11):1292-1299. 10.3346/jkms.2012.27.11.1292.
Identifying Genetic Susceptibility to Sensitization to Cephalosporins in Health Care Workers
- Affiliations
-
- 1Department of Allergy & Clinical Immunology, Ajou University School of Medicine, Suwon, Korea. hspark@ajou.ac.kr
- 2Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 3Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2157937
- DOI: http://doi.org/10.3346/jkms.2012.27.11.1292
Abstract
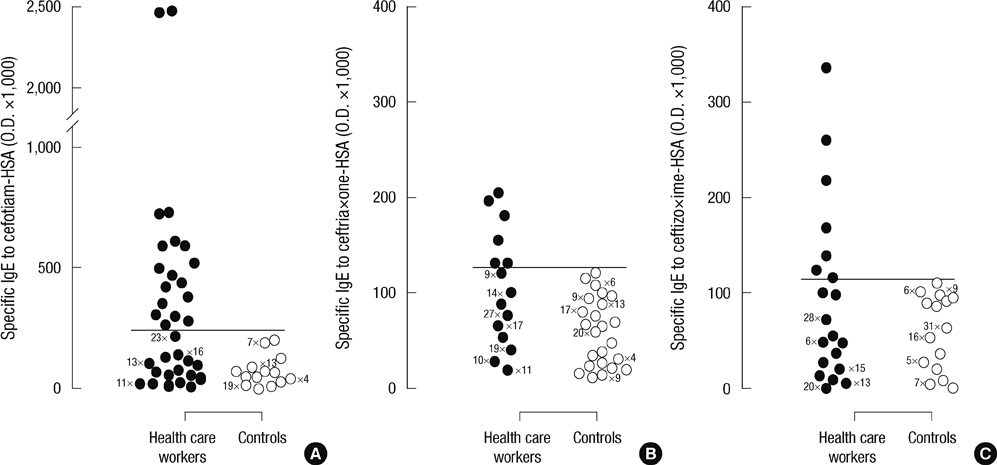
- Exposure to cephalosporins could cause occupational allergic diseases in health care workers (HCWs). We evaluated the prevalence of serum specific IgE and IgG antibodies to cephalosporin-human serum albumin (HSA) conjugate and to identify potential genetic risk factors associated with sensitization to cephalosporins in exposed HCWs. The study population consisted of 153 HCWs who had been exposed to antibiotics in a single university hospital and 86 unexposed healthy controls. A questionnaire survey of work-related symptoms (WRS) was administered. A skin-prick test (SPT) was performed, and serum-specific IgE and IgG antibodies to 3 commonly prescribed cephalosporins were measured by ELISA. Four single-nucleotide polymorphisms of the candidate genes related to IgE sensitization were genotyped. The prevalence of WRS to cephalosporins was 2.6%. The prevalence rates of serum-specific IgE and IgG antibodies to cephalosporins were 20.3% and 14.7%, respectively. The FcepsilonR1beta-109T > C polymorphism was significantly associated with IgE sensitization to cephalosporins in HCWs (P = 0.036, OR = 3.553; CI, 1.324-9.532). The in vitro functional assay demonstrated that the T allele of FcepsilonR1beta-109T had greater promoter activity than did the C allele (P < 0.001). The FcepsilonR1beta-109T > C polymorphism may be a potential genetic risk factor for increased IgE sensitization to cephalosporins.
MeSH Terms
-
Adult
Alleles
Anti-Bacterial Agents/analysis/*immunology
Cephalosporins/analysis/*immunology
Enzyme-Linked Immunosorbent Assay
Female
Genetic Predisposition to Disease
Health Personnel
Humans
Hypersensitivity/*diagnosis/epidemiology
Immunoglobulin E/blood
Immunoglobulin G/blood
Male
Occupational Diseases/*chemically induced/epidemiology
Occupational Exposure
Odds Ratio
Questionnaires
Receptors, IgE/genetics
Skin Tests
Young Adult
Anti-Bacterial Agents
Cephalosporins
Immunoglobulin G
Receptors, IgE
Immunoglobulin E
Figure
Cited by 1 articles
-
Immunologic Evaluation of Immediate Hypersensitivity to Cefaclor
Hye-Soo Yoo, Seung-Hyun Kim, Hyouk-Soo Kwon, Tae-Bum Kim, Young-Hee Nam, Young-Min Ye, Hae-Sim Park
Yonsei Med J. 2014;55(6):1473-1483. doi: 10.3349/ymj.2014.55.6.1473.
Reference
-
1. Ye YM, Kim SH, Kim SH, Kim SH, Park HS. Genetic polymorphisms of ADRB2 and IL10 may be associated with the risk of IgE sensitization to digestive powders in exposed medical personnel. Int Arch Allergy Immunol. 2010. 153:193–200.2. Choi IS, Han ER, Lim SW, Lim SR, Kim JN, Park SY, Chae SK, Lim HH, Seol YA, Bae YI, et al. Beta-lactam antibiotic sensitization and its relationship to allergic diseases in tertiary hospital nurses. Allergy Asthma Immunol Res. 2010. 2:114–122.3. Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Occupational asthma and IgE sensitization in a pharmaceutical company processing cefteram pivoxil. Korean J Med. 2003. 64:309–316.4. Yucesoy B, Johnson VJ. Genetic variability in susceptibility to occupational respiratory sensitization. J Allergy (Cairo). 2011. 2011:346719.5. Guéant JL, Guéant-Rodriguez RM, Viola M, Valluzzi RL, Romano A. IgE-mediated hypersensitivity to cephalosporins. Curr Pharm Des. 2006. 12:3335–3345.6. Aalberse RC, Schuurman J, van Ree R, Stapel S. IgG4 antibody assays in allergy diagnosis. Res Immunol. 1998. 149:263–266.7. Moscato G, Vandenplas O, Van Wijk RG, Malo JL, Perfetti L, Quirce S, Walusiak J, Castano R, Pala G, Gautrin D, et al. EAACI position paper on occupational rhinitis. Respir Res. 2009. 10:16.8. Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: prevalence, aetiology and determinants. Clin Exp Allergy. 2000. 30:1519–1534.9. Shirakawa T, Li A, Dubowitz M, Dekker JW, Shaw AE, Faux JA, Ra C, Cookson WO, Hopkin JM. Association between atopy and variants of the beta subunit of the high-affinity immunoglobulin E receptor. Nat Genet. 1994. 7:125–129.10. Qiao HL, Yang J, Zhang YW. Specific serum IgE levels and FceRIb genetic polymorphism in patients with penicillins allergy. Allergy. 2004. 59:1326–1332.11. Rosenwasser LJ, Klemm DJ, Dresback JK, Inamura H, Mascali JJ, Klinnert M, Borish L. Promoter polymorphisms in the chromosome 5 gene cluster in asthma and atopy. Clin Exp Allergy. 1995. 25:74–78.12. Apter AJ, Schelleman H, Walker A, Addya K, Rebbeck T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008. 122:152–158.13. Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Heterogeneity of IgE response to cefteram pivoxil was noted in 2 patients with cefteram-induced occupational asthma. J Allergy Clin Immunol. 2003. 112:209–210.14. Kim JE, Kim SH, Jin HJ, Hwang EK, Kim JH, Ye YM, Park HS. IgE Sensitization to cephalosporins in health care workers. Allergy Asthma Immunol Res. 2012. 4:85–91.15. Kim SH, Bae JS, Holloway J, Lee JT, Suh CH, Nahm DH, Park HS. A polymorphism of MS4A2 (-109T>C) encoding the β-chain of the high-affinity immunoglobulin E receptor (FcεR1β) is associated with a susceptibility to aspirin-intolerant asthma. Clin Exp Allergy. 2006. 36:877–883.16. Kim SH, Ye YM, Kim HM, Lee MK, Suh CH, Nahm DH, Park HS. Occupational allergy caused by inhalation of pancreatic extracts in the medical personnel and identification of the major allergens. Korean J Asthma Allergy Clin Immunol. 2007. 27:10–19.17. Nakamura S. Studies on asthma bronchiale. 6. On the occupational allergy caused by pancreatin among pharmacists. Arerugi. 1971. 20:361–364.18. Sastre J, Quirce S, Novalbos A, Lluch-Bernal M, Bombín C, Umpiérrez A. Occupational asthma induced by cephalosporins. Eur Respir J. 1999. 13:1189–1191.19. Kim JE, Kim SH, Choi GS, Ye YM, Park HS. Detection of specific IgE antibodies to cefotiam-HSA conjugate by ELISA in a nurse with occupational anaphylaxis. Allergy. 2010. 65:791–792.20. Tadokoro K, Niimi N, Ohtoshi T, Nakajima K, Takafuji S, Onodera K, Suzuki S, Muranaka M. Cefotiam-induced IgE-mediated occupational contact anaphylaxis of nurses: case reports, RAST analysis, and a review of the literature. Clin Exp Allergy. 1994. 24:127–133.21. Verna N, Di Giampaolo L, Renzetti A, Balatsinou L, Di Stefano F, Di Gioacchino G, Di Rocco P, Schiavone C, Boscolo P, Di Gioacchino M. Prevalence and risk factors for latex-related diseases among healthcare workers in an Italian general hospital. Ann Clin Lab Sci. 2003. 33:184–191.22. Donnay C, Denis MA, Magis R, Fevotte J, Massin N, Dumas O, Pin I, Choudat D, Kauffmann F, Le Moual N. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Environ Med. 2011. 68:611–617.23. Hur GY, Koh DH, Kim HA, Park HJ, Ye YM, Kim KS, Park HS. Prevalence of work-related symptoms and serum-specific antibodies to wheat flour in exposed workers in the bakery industry. Respir Med. 2008. 102:548–555.24. Wisnewski AV. Developments in laboratory diagnostics for isocyanate asthma. Curr Opin Allergy Clin Immunol. 2007. 7:138–145.25. Hur GY, Koh DH, Choi GS, Park HJ, Choi SJ, Ye YM, Kim KS, Park HS. Clinical and immunologic findings of methylene diphenyl diisocyanate-induced occupational asthma in a car upholstery factory. Clin Exp Allergy. 2008. 38:586–593.26. Mukai K, Obata K, Tsujimura Y, Karasuyama H. New insights into the roles for basophils in acute and chronic allergy. Allergol Int. 2009. 58:11–19.27. Ishizaka A, Sakiyama Y, Nakanishi M, Tomizawa K, Oshika E, Kojima K, Taguchi Y, Kandil E, Matsumoto S. The inductive effect of interleukin-4 on IgG4 and IgE synthesis in human peripheral blood lymphocytes. Clin Exp Immunol. 1990. 79:392–396.28. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011. 71:684–700.29. Filon FL, Radman G. Latex allergy: a follow up study of 1040 healthcare workers. Occup Environ Med. 2006. 63:121–125.30. Vandenplas O, Delwiche JP, Evrard G, Aimont P, van der Brempt X, Jamart J, Delaunois L. Prevalence of occupational asthma due to latex among hospital personnel. Am J Respir Crit Care Med. 1995. 151:54–60.31. Haddi E, Charpin D, Tafforeau M, Kulling G, Lanteaume A, Kleisbauer JP, Vervloet D. Atopy and systemic reactions to drugs. Allergy. 1990. 45:236–239.32. Hizawa N, Yamaguchi E, Jinushi E, Kawakami Y. A common FCER1B gene promoter polymorphism influences total serum IgE levels in a Japanese population. Am J Respir Crit Care Med. 2000. 161:906–909.33. Gervaziev YV, Kaznacheev VA, Gervazieva VB. Allelic polymorphisms in the interleukin-4 promoter regions and their association with bronchial asthma among the Russian population. Int Arch Allergy Immunol. 2006. 141:257–264.34. Dombrowicz D, Lin S, Flamand V, Brini AT, Koller BH, Kinet JP. Allergy-associated FcRbeta is a molecular amplifier of IgE- and IgG-mediated in vivo responses. Immunity. 1998. 8:517–529.35. Nishiyama C, Akizawa Y, Nishiyama M, Tokura T, Kawada H, Mitsuishi K, Hasegawa M, Ito T, Nakano N, Okamoto A, et al. Polymorphisms in the Fc epsilon RI beta promoter region affecting transcription activity: a possible promoter-dependent mechanism for association between Fc epsilon RI beta and atopy. J Immunol. 2004. 173:6458–6464.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- IgE Sensitization to Cephalosporins in Health Care Workers
- Effects of salicylates on the susceptibility of klebseilla pneumoniae to cephalosporins
- Exposure and Elevated Serum Total Immunoglobulin E Level are Major Risk Factors of Sensitization to Pancreatic Enzymes among Health Care Workers in a Single Hospital
- Clinical Use of Cephalosporins
- Plasmid Patterns end in Vitro Susceptibility of Neisseria Gonorrhoeae in Taegu