J Korean Med Sci.
2015 Jan;30(1):110-114. 10.3346/jkms.2015.30.1.110.
Megalocytic Interstitial Nephritis Following Acute Pyelonephritis with Escherichia coli Bacteremia: A Case Report
- Affiliations
-
- 1Department of Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Division of Nephrology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. shinehr@gmail.com
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2155455
- DOI: http://doi.org/10.3346/jkms.2015.30.1.110
Abstract
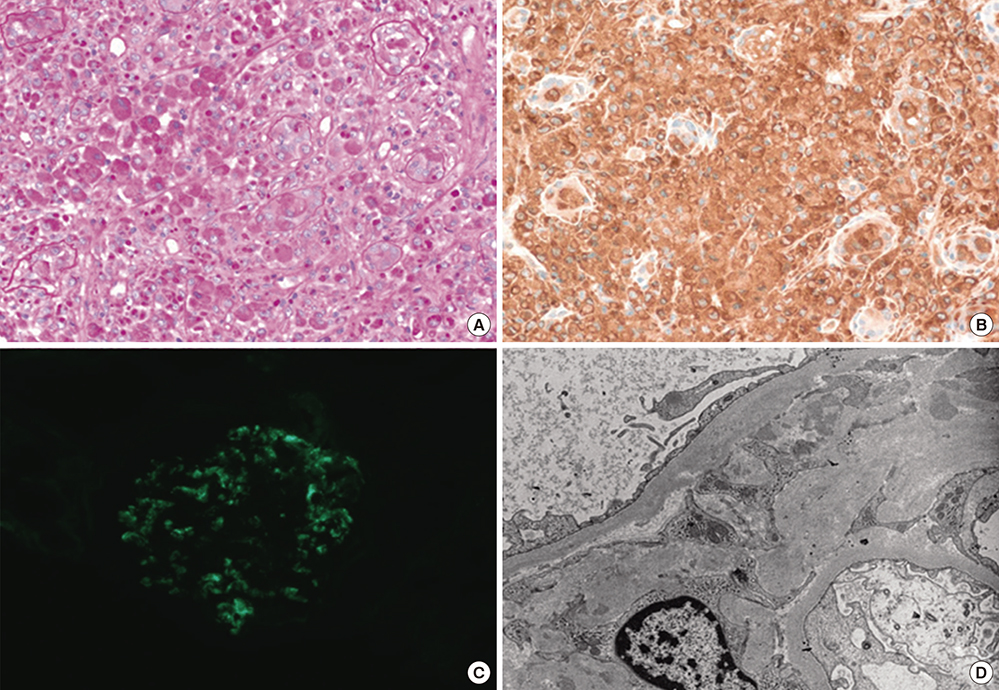
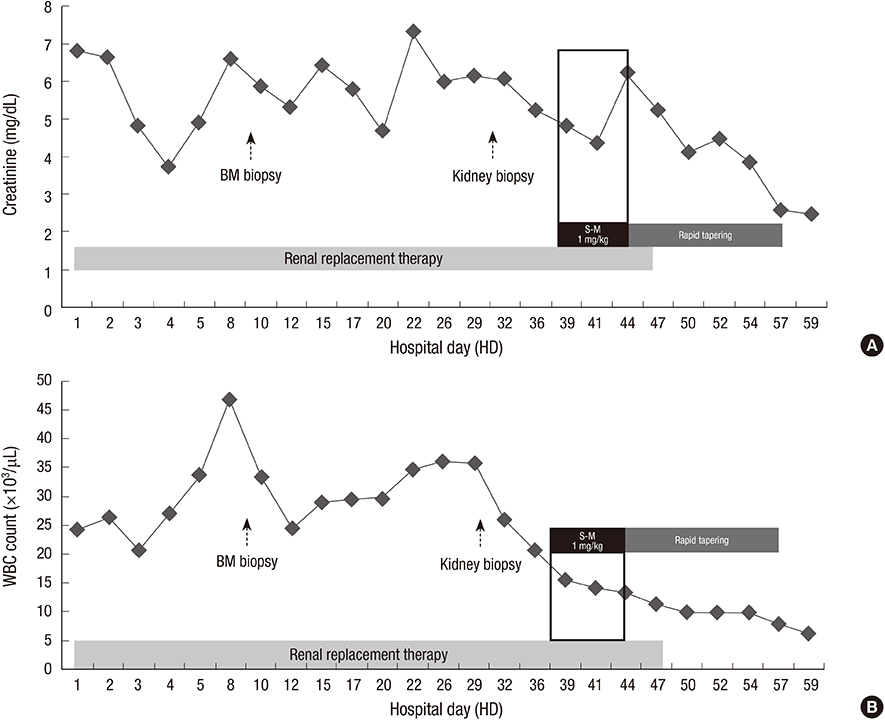
- Megalocytic interstitial nephritis is a rare form of kidney disease caused by chronic inflammation. We report a case of megalocytic interstitial nephritis occurring in a 45-yrold woman who presented with oliguric acute kidney injury and acute pyelonephritis accompanied by Escherichia coli bacteremia. Her renal function was not recovered despite adequate duration of susceptible antibiotic treatment, accompanied by negative conversion of bacteremia and bacteriuria. Kidney biopsy revealed an infiltration of numerous histiocytes without Michaelis-Gutmann bodies. The patient's renal function was markedly improved after short-term treatment with high-dose steroid.
MeSH Terms
-
Acute Disease
Acute Kidney Injury/complications/*drug therapy/pathology
Anti-Bacterial Agents/therapeutic use
Azithromycin/therapeutic use
Bacteremia/*drug therapy/microbiology/pathology
Cefotaxime/therapeutic use
Creatinine/blood
Escherichia coli
Escherichia coli Infections/*drug therapy/microbiology/pathology
Female
Humans
Kidney/pathology
Methylprednisolone/therapeutic use
Middle Aged
Nephritis, Interstitial/*drug therapy/immunology/pathology
Pyelonephritis/complications/*drug therapy/pathology
Renal Dialysis
Shock, Septic/drug therapy/microbiology
Anti-Bacterial Agents
Azithromycin
Cefotaxime
Creatinine
Methylprednisolone
Figure
Reference
-
1. Rubin RH, Contran RS, Tolkoff-Rubin NE. Urinary tract infection, pyelonephritis, and reflux nephropathy. In : Brenner BM, Levine SA, editors. Brenner and Rector's the kidney. 8th ed. Philadelphia: Saunders;2008. p. 313–331.2. Kobayashi A, Utsunomiya Y, Kono M, Ito Y, Yamamoto I, Osaka N, Hasegawa T, Hoshina S, Yamaguchi Y, Kawaguchi Y, et al. Malakoplakia of the kidney. Am J Kidney Dis. 2008; 51:326–330.3. YiXMLLink_XYZiter M, Ilgici D, Celik M, Arda IS, Hiçsönmez A. Renal parenchymal malacoplakia: a different stage of xanthogranulomatous pyelonephritis. J Pediatr Surg. 2007; 42:E35–E38.4. Mittal BV, Badhe BP. Xanthogranulomatous pyelonephritis: a clinicopathological study of 15 cases. J Postgrad Med. 1989; 35:209–214.5. al-Sulaiman MH, al-Khader AA, Mousa DH, al-Swailem RY, Dhar J, Haleem A. Renal parenchymal malacoplakia and megalocytic interstitial nephritis: clinical and histological features. Report of two cases and review of the literature. Am J Nephrol. 1993; 13:483–488.6. Esparza AR, McKay DB, Cronan JJ, Chazan JA. Renal parenchymal malakoplakia. Histologic spectrum and its relationship to megalocytic interstitial nephritis and xanthogranulomatous pyelonephritis. Am J Surg Pathol. 1989; 13:225–236.7. Bae GE, Yoon N, Park HY, Ha SY, Cho J, Lee Y, Kim KM, Park CK. Silent colonic malakoplakia in a living-donor kidney transplant recipient diagnosed during annual medical examination. Korean J Pathol. 2013; 47:163–166.8. Krupp G, Schneider W, Gobel U, Müller V, Haller H, Luft FC. Tumefactive megalocytic interstitial nephritis in a patient with Escherichia coli bacteremia. Am J Kidney Dis. 1995; 25:928–933.9. Jennette JC, Olson JL, Schwartz MM, Silva FG. Lippincott William. Heptinstall's pathology of the kidney. 6th ed. 2006. Philadelphia, PA: Lippincott Williams & Wilkins;p. 1546–1561.10. Hamvas A, Detre Z, Szinnay G. Malakoplakia of kidney and urinary tract. Report of a case of fatal outcome. Int Urol Nephrol. 1981; 13:55–63.11. Dasgupta P, Womack C, Turner AG, Blackford HN. Malacoplakia: von Hansemann's disease. BJU Int. 1999; 84:464–469.12. Kelly DR, Murad TM. Megalocytic interstitial nephritis, xanthogranulomatous pyelonephritis, and malakoplakia. An ultrastructural comparison. Am J Clin Pathol. 1981; 75:333–344.13. Mii A, Shimizu A, Masuda Y, Fujita E, Aki K, Ishizaki M, Sato S, Griesemer A, Fukuda Y. Current status and issues of C1q nephropathy. Clin Exp Nephrol. 2009; 13:263–274.14. Colvin RB. Diagnostic pathology: kidney diseases. Salt Lake City, Utah: Amirsys;2011. p. 84–86.15. Jo SK, Yun JW, Cha DR, Cho WY, Kim HK, Won NH. Anuric acute renal failure secondary to megalocytic interstitial nephritis in a patient with Behcet's disease. Clin Nephrol. 2000; 54:498–500.16. Tam VK, Kung WH, Li R, Chan KW. Renal parenchymal malacoplakia: a rare cause of ARF with a review of recent literature. Am J Kidney Dis. 2003; 41:E13–E17.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Escherichia Coli Empyema Preceded by Acute Pyelonephritis
- A Case of Huge Infected Adrenal Pseudocyst associated with Acute Pyelonephritis and E. coli Bacteremia
- A Case Report of Sepsis by Extended-Spectrum beta-Lactamase Producing Escherichia Coli
- Acute Appendicitis Presenting with Escherichia coli Bacteremia without Perforation in a Healthy Male
- A Case of Acute Renal Failure due to Bilateral Acute Pyelonephritis