Korean J Urol.
2015 Apr;56(4):318-323. 10.4111/kju.2015.56.4.318.
Changes of calcific density in pediatric patients with testicular microlithiasis
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kskim2@amc.seoul.kr
- 2Department of Urology, Kangwon National University Hospital, Chuncheon, Korea.
- KMID: 2155308
- DOI: http://doi.org/10.4111/kju.2015.56.4.318
Abstract
- PURPOSE
Testicular microlithiasis (TM) is a relatively rare clinical entity of controversial significance characterized by the existence of hydroxyapatite microliths located in the seminiferous tubules. The aim of this study was to observe the natural course of changes in the calcific density of pediatric TM.
MATERIALS AND METHODS
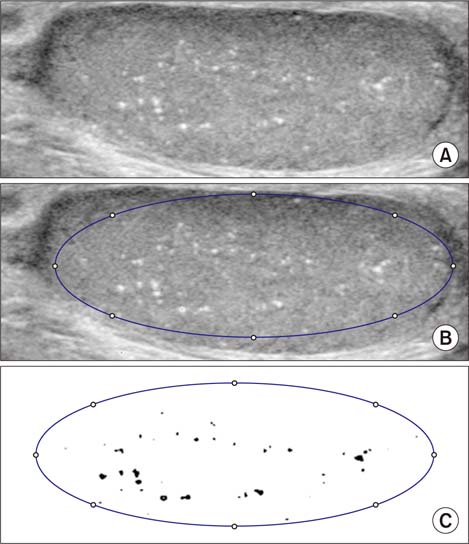
We included a total of 23 TM patients undergoing scrotal ultrasound (US) on at least two occasions from July 1997 to August 2014. We retrospectively analyzed the patient characteristics, clinical manifestations, specific pathological features, and clinical outcomes. We measured the calcified area and compared the calcific density between the initial and final USs.
RESULTS
The mean age at diagnosis was 11.3+/-4.6 years, and the follow-up period was 79.1+/-38.8 months (range, 25.4-152.9 months). During the follow-up period, no patients developed testicular cancer. Calcific density on US was increased in the last versus the initial US, but not to a statistically significant degree (3.74%+/-6.0% vs. 3.06%+/-4.38%, respectively, p=0.147). When we defined groups with increased and decreased calcification, we found that diffuse TM was categorized into the increased group to a greater degree than focal TM (10/20 vs. 4/23, respectively, p=0.049). In addition, five of eight cases of cryptorchidism (including two cases of bilateral cryptorchidism) were categorized in the increased calcification group.
CONCLUSIONS
Diffuse TM and cryptorchidism tend to increase calcific density. Close observation is therefore recommended for cases of TM combined with cryptorchidism and cases of diffuse TM.
MeSH Terms
-
Adolescent
Calcification, Physiologic
*Calculi/complications/epidemiology/pathology/physiopathology
Child
Cryptorchidism/diagnosis/etiology
Densitometry/methods
Follow-Up Studies
Gonadoblastoma/diagnosis/etiology
Humans
Male
Republic of Korea
Scrotum/*ultrasonography
Seminiferous Tubules/*pathology
*Testicular Diseases/complications/epidemiology/pathology/physiopathology
*Testicular Neoplasms/diagnosis/epidemiology/etiology
Figure
Reference
-
1. Doherty FJ, Mullins TL, Sant GR, Drinkwater MA, Ucci AA Jr. Testicular microlithiasis. A unique sonographic appearance. J Ultrasound Med. 1987; 6:389–392.2. Hobarth K, Szabo N, Klingler HC, Kratzik C. Sonographic appearance of testicular microlithiasis. Eur Urol. 1993; 24:251–255.3. Goede J, Hack WW, van der Voort-Doedens LM, Sijstermans K, Pierik FH. Prevalence of testicular microlithiasis in asymptomatic males 0 to 19 years old. J Urol. 2009; 182:1516–1520.4. Serter S, Gumus B, Unlu M, Tuncyurek O, Tarhan S, Ayyildiz V, et al. Prevalence of testicular microlithiasis in an asymptomatic population. Scand J Urol Nephrol. 2006; 40:212–214.5. Hobarth K, Susani M, Szabo N, Kratzik C. Incidence of testicular microlithiasis. Urology. 1992; 40:464–467.6. Yee WS, Kim YS, Kim SJ, Choi JB, Kim SI, Ahn HS. Testicular microlithiasis: prevalence and clinical significance in a population referred for scrotal ultrasonography. Korean J Urol. 2011; 52:172–177.7. Rashid HH, Cos LR, Weinberg E, Messing EM. Testicular microlithiasis: a review and its association with testicular cancer. Urol Oncol. 2004; 22:285–289.8. Ikinger U, Wurster K, Terwey B, Mohring K. Microcalcifications in testicular malignancy: diagnostic tool in occult tumor? Urology. 1982; 19:525–528.9. Chen JL, Chou YH, Tiu CM, Chiou HJ, Wang HK, Chiou SY, et al. Testicular microlithiasis: analysis of prevalence and associated testicular cancer in Taiwanese men. J Clin Ultrasound. 2010; 38:309–313.10. Ganem JP, Workman KR, Shaban SF. Testicular microlithiasis is associated with testicular pathology. Urology. 1999; 53:209–213.11. Bennett HF, Middleton WD, Bullock AD, Teefey SA. Testicular microlithiasis: US follow-up. Radiology. 2001; 218:359–363.12. Skyrme RJ, Fenn NJ, Jones AR, Bowsher WG. Testicular microlithiasis in a UK population: its incidence, associations and follow-up. BJU Int. 2000; 86:482–485.13. Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur Urol. 2012; 62:324–332.14. Montgomery JS, Bloom DA. The diagnosis and management of scrotal masses. Med Clin North Am. 2011; 95:235–244.15. Elzinga-Tinke JE, Sirre ME, Looijenga LH, van Casteren N, Wildhagen MF, Dohle GR. The predictive value of testicular ultrasound abnormalities for carcinoma in situ of the testis in men at risk for testicular cancer. Int J Androl. 2010; 33:597–603.16. McEniff N, Doherty F, Katz J, Schrager CA, Klauber G. Yolk sac tumor of the testis discovered on a routine annual sonogram in a boy with testicular microlithiasis. AJR Am J Roentgenol. 1995; 164:971–972.17. Winter TC 3rd, Zunkel DE, Mack LA. Testicular carcinoma in a patient with previously demonstrated testicular microlithiasis. J Urol. 1996; 155:648.18. Dagash H, Mackinnon EA. Testicular microlithiasis: what does it mean clinically? BJU Int. 2007; 99:157–160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of 8 Year-old Boy with Testicular Microlithiasis Showing Bilateral Testicular Enlargement
- Testicular microlithiasis in a boy with X-linked adrenal hypoplasia congenita
- Sonographically Detected Testicular Microlithiasis
- Fifteen Cases of Testicular Microlithiasis
- The Clinical Significance of Pediatric Testicular Microlithiasis in Relation to Testicular Tumors