Ann Pediatr Endocrinol Metab.
2018 Sep;23(3):162-165. 10.6065/apem.2018.23.3.162.
Testicular microlithiasis in a boy with X-linked adrenal hypoplasia congenita
- Affiliations
-
- 14th Department of Pediatrics, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Papageorgiou General Hospital, Thessaloniki, Greece. gallitsin@gmail.com
- KMID: 2422482
- DOI: http://doi.org/10.6065/apem.2018.23.3.162
Abstract
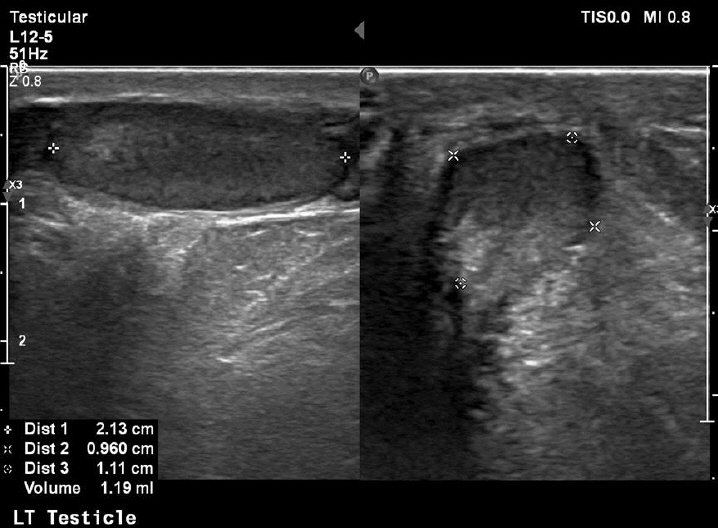
- X-linked adrenal hypoplasia congenita (AHC) is a rare disorder that usually presents clinically as adrenal insufficiency in early infancy. It is caused by mutations in the NR0B1 gene which is located on the short arm of chromosome X (Xp21). The NR0B1 gene plays an important role in normal development and function of both the adrenal and gonadal axes and some patients with the disease can present in adolescence with hypogonadotropic hypogonadism. Testicular microlithiasis is an ultrasonographic finding of unknown etiology that has been associated with several benign conditions such as cryptorchidism, congenital adrenal hyperplasia, varicoceles, and testicular malignancy. We report the case of an 11-year-old boy who was diagnosed at the age of 8 months with X-linked AHC due to adrenal failure and presented testicular microlithiasis during follow-up. To the best of our knowledge, this is the first case of an X-linked AHC patient diagnosed with testicular microlithiasis in follow-up.
MeSH Terms
Figure
Reference
-
References
1. Suntharalingham JP, Buonocore F, Duncan AJ, Achermann JC. DAX-1 (NR0B1) and steroidogenic factor-1 (SF-1, NR5A1) in human disease. Best Pract Res Clin Endocrinol Metab. 2015; 29:607–19.
Article2. Landau Z, Hanukoglu A, Sack J, Goldstein N, Weintrob N, Eliakim A, et al. Clinical and genetic heterogeneity of congenital adrenal hypoplasia due to NR0B1 gene mutations. Clin Endocrinol (Oxf). 2010; 72:448–54.3. Poyrazoglu S, Saka N, Agayev A, Yekeler E. Prevalence of testicular microlithiasis in males with congenital adrenal hyperplasia and its association with testicular adrenal rest tumors. Horm Res Paediatr. 2010; 73:443–8.
Article4. Backus ML, Mack LA, Middleton WD, King BF, Winter TC 3rd, True LD. Testicular microlithiasis: imaging appearances and pathologic correlation. Radiology. 1994; 192:781–5.
Article5. Phelan JK, McCabe ER. Mutations in NR0B1 (DAX1) and NR5A1 (SF1) responsible for adrenal hypoplasia congenita. Hum Mutat. 2001; 18:472–87.6. Lin L, Gu WX, Ozisik G, To WS, Owen CJ, Jameson JL, et al. Analysis of DAX1 (NR0B1) and steroidogenic factor-1 (NR5A1) in children and adults with primary adrenal failure: ten years' experience. J Clin Endocrinol Metab. 2006; 91:3048–54.
Article7. Habiby RL, Boepple P, Nachtigall L, Sluss PM, Crowley WF Jr, Jameson JL. Adrenal hypoplasia congenita with hypogonadotropic hypogonadism: evidence that DAX-1 mutations lead to combined hypothalmic and pituitary defects in gonadotropin production. J Clin Invest. 1996; 98:1055–62.
Article8. Seminara SB, Achermann JC, Genel M, Jameson JL, Crowley WF Jr. X-linked adrenal hypoplasia congenita: a mutation in DAX1 expands the phenotypic spectrum in males and females. J Clin Endocrinol Metab. 1999; 84:4501–9.9. Doherty FJ, Mullins TL, Sant GR, Drinkwater MA, Ucci AA Jr. Testicular microlithiasis. A unique sonographic appearance. J Ultrasound Med. 1987; 6:389–92.
Article10. Priebe CJ Jr, Garret R. Testicular calcification in a 4-year-old boy. Pediatrics. 1970; 46:785–8.
Article11. Goede J, Hack WW. Clinical aspects of testicular microlithiasis in boys: a review. J Pediatr Urol. 2012; 8:459–69.
Article12. Yesil S, Tanyildiz HG, Sahin G. How should we monitor boys with testicular microlithiasis? Pediatr Hematol Oncol. 2016; 33:171–7.
Article13. Kocaoğlu M, Bozlar U, Bulakbaşi N, Sağlam M, Uçöz T, Somuncu I. Testicular microlithiasis in pediatric age group: ultrasonography findings and literature review. Diagn Interv Radiol. 2005; 11:60–5.14. Yu MK, Jung MK, Kim KE, Kwon AR, Chae HW, Kim DH, et al. Clinical manifestations of testicular adrenal rest tumor in males with congenital adrenal hyperplasia. Ann Pediatr Endocrinol Metab. 2015; 20:155–61.
Article15. Aizenstein RI, DiDomenico D, Wilbur AC, O'Neil HK. Testicular microlithiasis: association with male infertility. J Clin Ultrasound. 1998; 26:195–8.
Article16. Meachem SJ, Nieschlag E, Simoni M. Inhibin B in male reproduction: pathophysiology and clinical relevance. Eur J Endocrinol. 2001; 145:561–71.
Article17. Lam DL, Gerscovich EO, Kuo MC, McGahan JP. Testicular microlithiasis: our experience of 10 years. J Ultrasound Med. 2007; 26:867–73.18. Miller FN, Rosairo S, Clarke JL, Sriprasad S, Muir GH, Sidhu PS. Testicular calcification and microlithiasis: association with primary intra-testicular malignancy in 3,477 patients. Eur Radiol. 2007; 17:363–9.
Article19. Silveri M, Bassani F, Colajacomo M, Orazi C, Adorisio O. Management and follow-up of pediatric asymptomatic testicular microlithiasis: are we doing it well? Urol J. 2011; 8:287–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central precocious puberty in a patient with X-linked adrenal hypoplasia congenita and Xp21 contiguous gene deletion syndrome
- A Case of 8 Year-old Boy with Testicular Microlithiasis Showing Bilateral Testicular Enlargement
- Identification of a novel point mutation in DAX-1 gene in a patient with adrenal hypoplasia congenita
- A novel mutation in the DAX1 gene in a newborn with adrenal hypoplasia congenita in Korea
- A novel variant in NR0B1 causing X-linked adrenal hypoplasia congenita