Ewha Med J.
2016 Jan;39(1):10-13. 10.12771/emj.2016.39.1.10.
Cutaneous Mucormycosis in a Patient with Diabetes Mellitus
- Affiliations
-
- 1Department of Internal Medicine, Hongik Hospital, Seoul, Korea. yeonigge00@naver.com
- KMID: 2152751
- DOI: http://doi.org/10.12771/emj.2016.39.1.10
Abstract
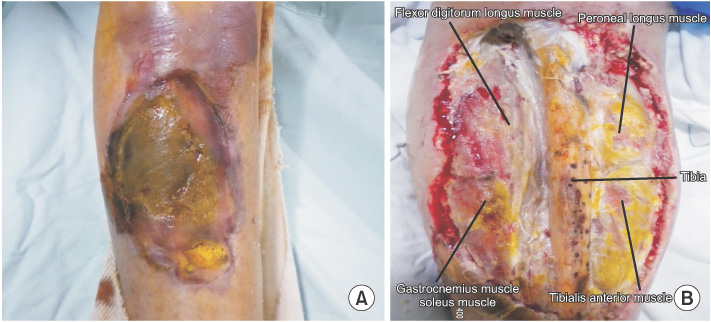
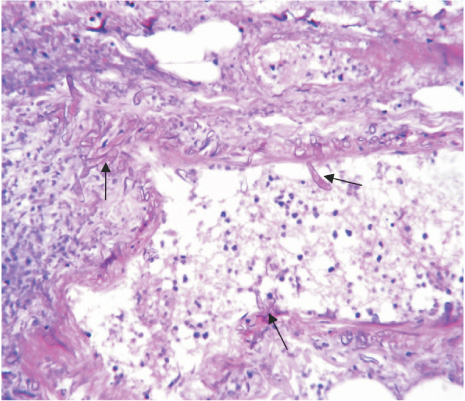
- Mucormycosis is a rare disease caused by fungi. Most commonly involved sites of mucormycosis infection are sinuses, lungs, skin and soft tissues. Systemic risk factors for mucormycosis are diabetes mellitus, neutropenia, corticosteroid use, hematological malignancies, organ transplantation, metabolic acidosis, deferoxamine use and advanced age. Local risk factors are history of trauma, burns, surgery and motor vehicle accidents. We present a case of cutaneous mucormycosis in a patient with diabetes mellitus. A 66-year-old female with uncontrolled diabetes mellitus, admitted with necrotizing lesion after minor abrasions on leg. We took a culture of the lesion and it is diagnosed with mucormycosis. Disease progressed despite administration of systemic amphotericin B. We performed above-knee amputation and changed antifungal agents into liposomal amphotericin B. A tissue biopsy showed nonseptate, irregularly wide fungal hyphae with frequent right-angle branching. Our case report suggests that patients with risk factors should be observed carefully.
MeSH Terms
Figure
Reference
-
1. Camara-Lemarroy CR, Gonzalez-Moreno EI, Rodriguez-Gutierrez R, Rendon-Ramirez EJ, Ayala-Cortes AS, Fraga-Hernandez ML, et al. Clinical features and outcome of mucormycosis. Interdiscip Perspect Infect Dis. 2014; 2014:562610.2. Mantadakis E, Samonis G. Clinical presentation of zygomycosis. Clin Microbiol Infect. 2009; 15:Suppl 5. 15–20.3. Ingram PR, Suthananthan AE, Rajan R, Pryce TM, Sieunarine K, Gardam DJ, et al. Cutaneous mucormycosis and motor vehicle accidents: findings from an Australian case series. Med Mycol. 2014; 52:819–825.4. Zaman K, Kaur H, Rudramurthy SM, Singh M, Parashar A, Chakrabarti A. Cutaneous mucormycosis of scalp and eyelids in a child with type I diabetes mellitus. Indian J Dermatol Venereol Leprol. 2015; 81:275–278.5. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005; 41:634–653.6. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012; 54:Suppl 1. S23–S34.7. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000; 13:236–301.8. Iida T, Sawada N, Takahashi M, Zendejas IR, Kayler LK, Magliocca JF, et al. Successful treatment of invasive mucormycosis in a liver transplant patient by arm amputation. Transplant Proc. 2010; 42:2794–2796.9. Su WP, Davis MD, Weenig RH, Powell FC, Perry HO. Pyoderma gangrenosum: clinicopathologic correlation and proposed diagnostic criteria. Int J Dermatol. 2004; 43:790–800.10. Kerr OA, Bong C, Wallis C, Tidman MJ. Primary cutaneous mucormycosis masquerading as pyoderma gangrenosum. Br J Dermatol. 2004; 150:1212–1213.11. Geller JD, Peters MS, Su WP. Cutaneous mucormycosis resembling superficial granulomatous pyoderma in an immunocompetent host. J Am Acad Dermatol. 1993; 29:462–465.12. Luo Y, Zeng F, Huang X, Li Q, Tan G, Xi L, et al. Successful treatment of a necrotizing fasciitis patient caused by Mucor indicus with amphotericin B and skin grafting. Mycopathologia. 2014; 177:187–192.13. de Oliveira-Neto MP, Da Silva M, Fialho Monteiro PC, Lazera M, de Almeida Paes R, Novellino AB, et al. Cutaneous mucormycosis in a young, immunocompetent girl. Med Mycol. 2006; 44:567–570.14. Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect. 2014; 20:Suppl 3. 5–26.15. Ahmadinejad Z, Khazraiyan H, Ghanbari F, Ahmadi B, Gerami Shoar M. Cutaneous Mucormycosis in a Diabetic Patient following Traditional Dressing. Case Rep Dermatol Med. 2013; 2013:894927.