The Dose-Related Effects of Extracorporeal Shock Wave Therapy for Knee Osteoarthritis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Gwangju Veterans Hospital, Gwangju, Korea. standupmd@hanmail.net
- KMID: 2148233
- DOI: http://doi.org/10.5535/arm.2015.39.4.616
Abstract
OBJECTIVE
To investigate the dose-related effects of extracorporeal shock wave therapy (ESWT) for knee osteoarthritis.
METHODS
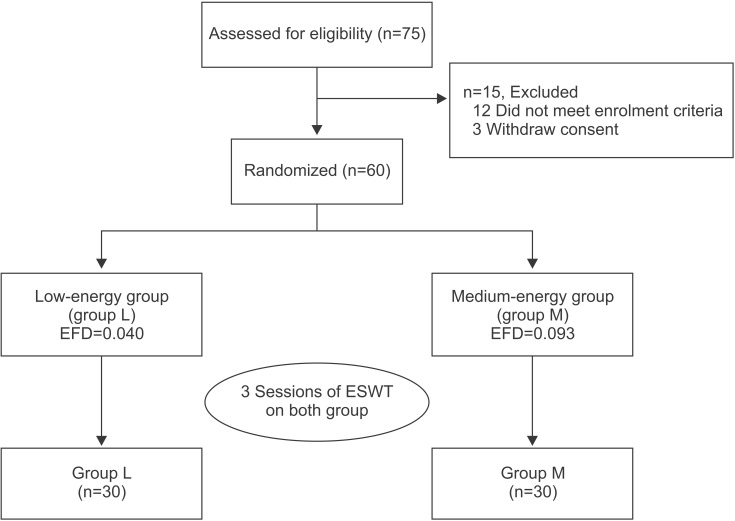
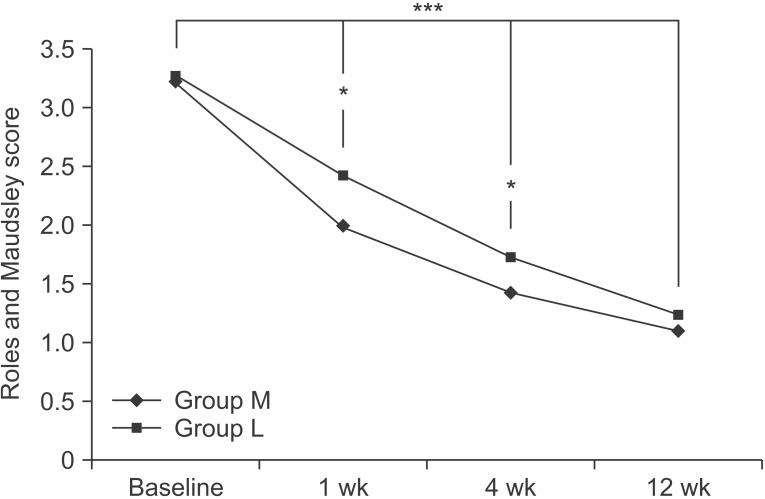
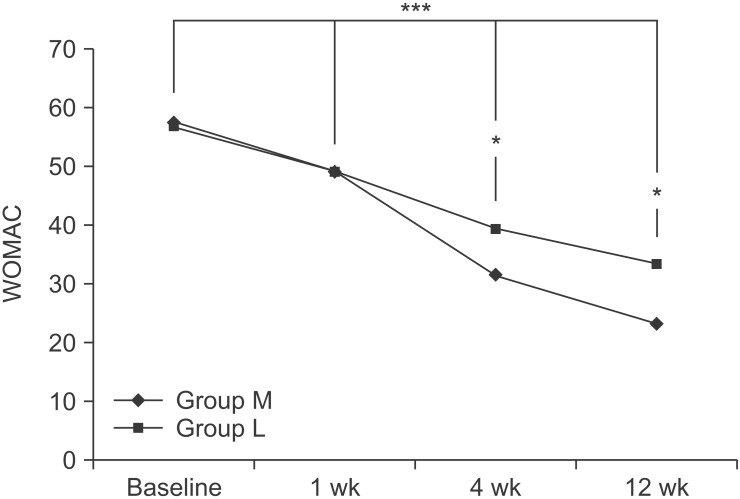
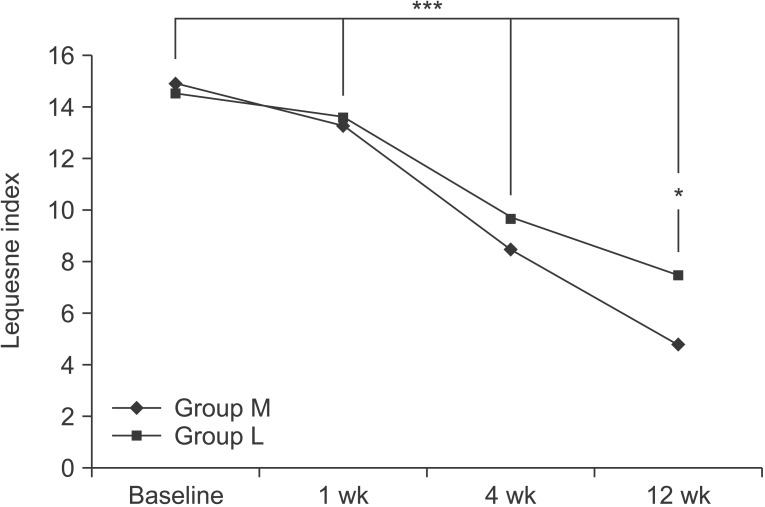
Seventy-five subjects were recruited, 60 of which met the inclusion criteria. The patients were randomly classified into two groups: group L, which was a low-energy group (n=30; 1,000 shocks/session; energy flux density [EFD], 0.040 mJ/mm2) and group M, which was a medium-energy group (n=30; 1,000 shocks/session; EFD, 0.093 mJ/mm2). For each group, 1,000 shock waves were delivered to the medial tibial plateau area, once a week, for 3 weeks. The main outcome measures were the visual analogue scale (VAS), the Roles and Maudsley (RM) score, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and the Lequesne index. Each assessment was performed at the baseline and at 1, 4, and 12 weeks after ESWT.
RESULTS
In both groups, the VAS, the RM and WOMAC scores, and the Lequesne index were significantly improved over time (p<0.001), and group M showed greater improvement over group L at the 1, 4 and 12 weeks assessments.
CONCLUSION
In this study, medium-energy group (group M) showed greater improvement in regard to relieving pain and restoring functional outcome than the low-energy group (group L). Therefore, EFD can be considered to have significant influence when treating with ESWT for knee osteoarthritis.
MeSH Terms
Figure
Cited by 4 articles
-
Effects of Extracorporeal Shockwave Therapy in Chronic Stroke Patients With Knee Osteoarthritis: A Pilot Study
Sung Jun Cho, Ja Ryung Yang, Hee Seung Yang, Hea-Eun Yang
Ann Rehabil Med. 2016;40(5):862-870. doi: 10.5535/arm.2016.40.5.862.Effect of Extracorporeal Shockwave Therapy Versus Intra-articular Injections of Hyaluronic Acid for the Treatment of Knee Osteoarthritis
June-Kyung Lee, Bong-Yeon Lee, Woo-Yong Shin, Min-Ji An, Kwang-Ik Jung, Seo-Ra Yoon
Ann Rehabil Med. 2017;41(5):828-835. doi: 10.5535/arm.2017.41.5.828.Comparison Between Extracorporeal Shock Wave Therapy and Intra-articular Hyaluronic Acid Injections in the Treatment of First Carpometacarpal Joint Osteoarthritis
Francesco Ioppolo, Fabiana Saracino, Rosaria Sabrina Rizzo, Giampaolo Monacelli, Danilo Lanni, Luca Di Sante, Angelo Cacchio, Valter Santilli, Teresa Venditto
Ann Rehabil Med. 2018;42(1):92-100. doi: 10.5535/arm.2018.42.1.92.Duration of Treatment Effect of Extracorporeal Shock Wave on Spasticity and Subgroup-Analysis According to Number of Shocks and Application Site: A Meta-Analysis
Jae Ho Oh, Hee Dong Park, Seung Hee Han, Ga Yang Shim, Kyung Yeul Choi
Ann Rehabil Med. 2019;43(2):163-177. doi: 10.5535/arm.2019.43.2.163.
Reference
-
1. Dunlop DD, Manheim LM, Song J, Chang RW. Arthritis prevalence and activity limitations in older adults. Arthritis Rheum. 2001; 44:212–221.
Article2. Dawson J, Linsell L, Zondervan K, Rose P, Randall T, Carr A, et al. Epidemiology of hip and knee and its impact on overall health status in older adults. Rheumatology (Oxford). 2004; 43:497–504. PMID: 14762225.3. Peat G, McCamey R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary healthcare. Ann Rheum Dis. 2001; 60:91–97.4. Sofat N, Ejindu V, Kiely P. What makes osteoarthritis painful? The evidence for local and central pain processing. Rheumatology (Oxford). 2011; 50:2157–2165. PMID: 21954151.
Article5. McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014; 22:363–388. PMID: 24462672.
Article6. Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res. 2012; 7:11. PMID: 22433113.
Article7. Wang CJ, Yang KD, Wang FS, Chen HH, Wang JW. Shock wave therapy for calcific tendinitis of the shoulder: a prospective clinical study with two-year follow-up. AM J Sports Med. 2003; 31:425–430. PMID: 12750138.8. Rompe JD, Theis C, Maffulli N. Shock wave treatment for tennis elbow. Orthopade. 2005; 34:567–570. PMID: 15886855.9. Rompe JD. Shock-wave therapy for plantar fasciitis. J Bone Joint Surg Am. 2005; 87:681–682. PMID: 15786568.
Article10. Revenaugh MS. Extracorporeal shock wave therapy for treatment of osteoarthritis in the horse: clinical applications. Vet Clin North Am Equine Pract. 2005; 21:609–625. PMID: 16297724.
Article11. Frisbie DD, Kawcak CE, McIlwraith CW. Evaluation of the effect of extracorporeal shock wave treatment on experimentally induced osteoarthritis in middle carpal joints of horses. AM J Vet Res. 2009; 70:449–454. PMID: 19335099.
Article12. Ochiai N, Ohtori S, Sasho T, Nakagawa K, Takahashi K, Takahashi N, et al. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthr Cartil. 2007; 15:1093–1096. PMID: 17466542.
Article13. Zhao Z, Ji H, Jing R, Liu C, Wang M, Zhai L, et al. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Arch Orthop Trauma Surg. 2012; 132:1547–1553. PMID: 22825641.
Article14. Zhao Z, Jing R, Shi Z, Zhao B, Ai Q, Xing G. Efficacy of extracorporeal shockwave therapy for knee osteoarthritis: a randomized controlled trial. J Surg Res. 2013; 185:661–666. PMID: 23953895.
Article15. Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum. 1986; 29:1039–1049. PMID: 3741515.
Article16. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957; 16:494–502. PMID: 13498604.
Article17. Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983; 16:87–101. PMID: 6602967.
Article18. Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972; 54:499–508. PMID: 4340924.19. Bellamy N, Campbell J, Stevens J, Pilch L, Stewart C, Mahmood Z. Validation study of a computerized version of the Western Ontario and McMaster Universities VA3.0 Osteoarthritis Index. J Rheumatol. 1997; 24:2413–2415. PMID: 9415651.20. Lequesne M. Clinical feature, diagnostic criteria, functional assessments and radiological classifications of osteoarthritis. Rheumatology. 1982; 7:1–10.21. Kon E, Filardo G, Drobnic M, Madry H, Jelic M, Dijk N, et al. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012; 20:436–449. PMID: 22037809.
Article22. Takahashi N, Ohtori S, Saisu T, Moriya H, Wada Y. Second application of low-energy shock waves has a cumulative effect on free nerve endings. Clin Orthop Relat Res. 2006; 443:315–319. PMID: 16462457.
Article23. Speed CA. Extracorporeal shock-wave therapy in the management of chronic soft-tissue conditions. J Bone Joint Surg. 2004; 86:165–171.
Article24. Thiel M. Application of shock waves in medicine. Clin Orthop Relat Res. 2001; 387:18–21. PMID: 11400881.
Article25. Wang CJ, Wang FS, Yang KD, Weng LH, Hsu CC, Huang CS, et al. Shock wave therapy induces neovascularization at the tendon-bone junction: a study in rabbits. J Orthop Res. 2003; 21:984–989. PMID: 14554209.
Article26. Wang CJ, Weng LH, Ko JY, Wang JW, Chen JM, Sun YC, et al. Extracorporeal shockwave shows regression of osteoarthritis of the knee in rats. J Surg Res. 2011; 171:601–608. PMID: 20851422.
Article27. Wang CJ, Sun YC, Wong T, Hsu SL, Chou WY, Chang HW. Extracorporeal shockwave therapy shows timedependent chondroprotective effects in osteoarthritis of the knee in rats. J Surg Res. 2012; 178:196–205. PMID: 22608545.
Article28. Rompe JD, Furia J, Weil L, Maffulli N. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007; 81-82:183–208. PMID: 17456546.
Article29. Gollwitzer H, Diehl P, von Korff A, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg. 2007; 46:348–357. PMID: 17761319.
Article30. Metzner G, Dohnalek C, Aigner E. High-energy extracorporeal shock-wave therapy for the treatment of chronic plantar fasciitis. Foot Ankle Int. 2010; 31:790–796. PMID: 20880482.31. Rompe JD, Meurer A, Nafe B, Hofmann A, Gerdesmeyer L. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fasciiitis. J Orthop Res. 2005; 23:931–941. PMID: 16023010.32. Renz H, Rupp S. Effects of shock waves on chondrocytes and their relevance in clinical practice. Arch Orthop Trauma Surg. 2009; 129:641–647. PMID: 18560852.
Article33. Mayer-Wagner S, Ernst J, Maier M, Chiquet M, Joos H, Muller PE, et al. The effect of high-energy extracorporeal shock waves on hyaline cartilage of adult rats in vivo. J Orthop Res. 2010; 28:1050–1056. PMID: 20135673.
Article34. Ohtori S, Inoue G, Mannoji C, Saisu T, Takahashi K, Mitsuhashi S, et al. Shock wave application to rat skin induces degeneration and reinnervation of sensory nerve fibers. Neurosci Lett. 2001; 315:57–60. PMID: 11711214.35. McClure S, Dorfmuller C. Extracorporeal shock wave therapy: theory and equipment. Clin Tech Equine Pract. 2003; 2:348–357.
Article36. Rompe JD, Kirkpatrick CJ, Kullmer K, Schwitalle M, Krischek O. Dose-related effects of shock waves on rabbit tendo achillis: a sonographic and histological study. J Bone Joint Surg Br. 1998; 80:546–552. PMID: 9619954.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Extracorporeal Shock Wave Therapy for Knee Osteoarthritis
- Current Concepts in Extracorporeal Shock Wave Therapy
- Effect of Radial Extracorporeal Shock Wave Therapy in Patients With Fabella Syndrome
- Suggestions for Effective Extracorporeal Shock Wave Treatment Methods for Lateral Epicondylitis
- Dose Related Effect of Extracorporeal Shock Wave Therapy in Lateral Epicondylitis