Ann Rehabil Med.
2015 Oct;39(5):763-771. 10.5535/arm.2015.39.5.763.
Associations Between Prolonged Intubation and Developing Post-extubation Dysphagia and Aspiration Pneumonia in Non-neurologic Critically Ill Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. yh0316.park@samsung.com
- KMID: 2148207
- DOI: http://doi.org/10.5535/arm.2015.39.5.763
Abstract
OBJECTIVE
To identify the associations between the duration of endotracheal intubation and developing post-extubational supraglottic and infraglottic aspiration (PEA) and subsequent aspiration pneumonia.
METHODS
This was a retrospective observational study from January 2009 to November 2014 of all adult patients who had non-neurologic critical illness, required endotracheal intubation and were referred for videofluoroscopic swallowing study. Demographic information, intensive care unit (ICU) admission diagnosis, severity of critical illness, duration of endotracheal intubation, length of stay in ICU, presence of PEA and severity of dysphagia were reviewed.
RESULTS
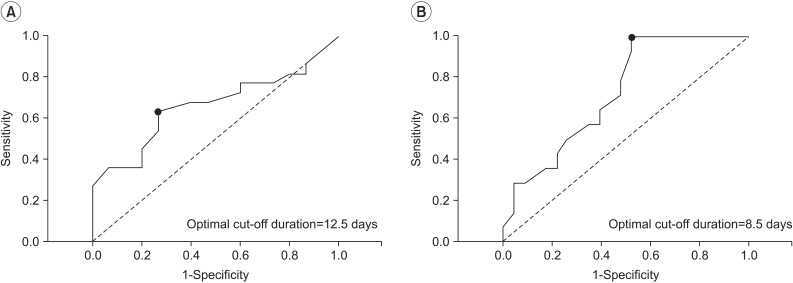
Seventy-four patients were enrolled and their PEA frequency was 59%. Patients with PEA had significantly longer endotracheal intubation durations than did those without (median [interquartile range]: 15 [9-21] vs. 10 [6-15] days; p=0.02). In multivariate logistic regression analysis, the endotracheal intubation duration was significantly associated with PEA (odds ratio, 1.09; 95% confidence interval [CI], 1.01-1.18; p=0.04). Spearman correlation analysis of intubation duration and dysphagia severity showed a positive linear association (r=0.282, p=0.02). The areas under the receiver operating characteristic curves (AUCs) of endotracheal intubation duration for developing PEA and aspiration pneumonia were 0.665 (95% CI, 0.542-0.788; p=0.02) and 0.727 (95% CI, 0.614-0.840; p=0.001), respectively.
CONCLUSION
In non-neurologic critically ill patients, the duration of endotracheal intubation was independently associated with PEA development. Additionally, the duration was positively correlated with dysphagia severity and may be helpful for identifying patients who require a swallowing evaluation after extubation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Association of Post-extubation Dysphagia With Tongue Weakness and Somatosensory Disturbance in Non-neurologic Critically Ill Patients
Hee Seon Park, Jung Hoi Koo, Sun Hong Song
Ann Rehabil Med. 2017;41(6):961-968. doi: 10.5535/arm.2017.41.6.961.
Reference
-
1. Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: a systematic review. Chest. 2010; 137:665–673. PMID: 20202948.2. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.3. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med. 1981; 70:65–76. PMID: 7457492.
Article4. Colice GL, Stukel TA, Dain B. Laryngeal complications of prolonged intubation. Chest. 1989; 96:877–884. PMID: 2791687.
Article5. Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003; 24:457–471. PMID: 14535220.
Article6. de Larminat V, Montravers P, Dureuil B, Desmonts JM. Alteration in swallowing reflex after extubation in intensive care unit patients. Crit Care Med. 1995; 23:486–490. PMID: 7874899.
Article7. Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: a prospective analysis of contributing factors. Laryngoscope. 2011; 121:596–600. PMID: 21344442.
Article8. Ajemian MS, Nirmul GB, Anderson MT, Zirlen DM, Kwasnik EM. Routine fiberoptic endoscopic evaluation of swallowing following prolonged intubation: implications for management. Arch Surg. 2001; 136:434–437. PMID: 11296115.9. Barker J, Martino R, Reichardt B, Hickey EJ, Ralph-Edwards A. Incidence and impact of dysphagia in patients receiving prolonged endotracheal intubation after cardiac surgery. Can J Surg. 2009; 52:119–124. PMID: 19399206.10. Barquist E, Brown M, Cohn S, Lundy D, Jackowski J. Postextubation fiberoptic endoscopic evaluation of swallowing after prolonged endotracheal intubation: a randomized, prospective trial. Crit Care Med. 2001; 29:1710–1713. PMID: 11546969.
Article11. El Solh A, Okada M, Bhat A, Pietrantoni C. Swallowing disorders post orotracheal intubation in the elderly. Intensive Care Med. 2003; 29:1451–1455. PMID: 12904855.
Article12. Hogue CW Jr, Lappas GD, Creswell LL, Ferguson TB Jr, Sample M, Pugh D, et al. Swallowing dysfunction after cardiac operations. Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995; 110:517–522. PMID: 7637370.
Article13. Rousou JA, Tighe DA, Garb JL, Krasner H, Engelman RM, Flack JE 3rd, et al. Risk of dysphagia after transesophageal echocardiography during cardiac operations. Ann Thorac Surg. 2000; 69:486–490. PMID: 10735685.
Article14. Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010; 136:784–789. PMID: 20713754.15. Macht M, King CJ, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, Moss M. Post-extubation dysphagia is associated with longer hospitalization in survivors of critical illness with neurologic impairment. Crit Care. 2013; 17:R119. PMID: 23786755.
Article16. Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, et al. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011; 15:R231. PMID: 21958475.
Article17. Brodsky MB, Gellar JE, Dinglas VD, Colantuoni E, Mendez-Tellez PA, Shanholtz C, et al. Duration of oral endotracheal intubation is associated with dysphagia symptoms in acute lung injury patients. J Crit Care. 2014; 29:574–579. PMID: 24631168.
Article18. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003; 124:328–336. PMID: 12853541.
Article19. Macht M, Wimbish T, Bodine C, Moss M. ICU-acquired swallowing disorders. Crit Care Med. 2013; 41:2396–2405. PMID: 23939361.
Article20. Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008; 19:769–785. PMID: 18940640.
Article21. Ferraris VA, Ferraris SP, Moritz DM, Welch S. Oropharyngeal dysphagia after cardiac operations. Ann Thorac Surg. 2001; 71:1792–1796. PMID: 11426749.
Article22. Keeling WB, Lewis V, Blazick E, Maxey TS, Garrett JR, Sommers KE. Routine evaluation for aspiration after thoracotomy for pulmonary resection. Ann Thorac Surg. 2007; 83:193–196. PMID: 17184659.
Article23. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article24. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article25. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/ North American multicenter study. JAMA. 1993; 270:2957–2963. PMID: 8254858.26. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–829. PMID: 3928249.27. Vincent JL, Moreno R, Takala J, Willatts S, De Mendona A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–710. PMID: 8844239.28. Lin CW, Chang YC, Chen WS, Chang K, Chang HY, Wang TG. Prolonged swallowing time in dysphagic Parkinsonism patients with aspiration pneumonia. Arch Phys Med Rehabil. 2012; 93:2080–2084. PMID: 22846454.
Article29. Seo WH, Oh JH, Nam YH, Sung IY. Clinical study of aspiration pneumonia in stroke patients. J Korean Acad Rehabil Med. 1994; 18:52–58.30. Komiya K, Ishii H, Kadota J. Healthcare-associated pneumonia and aspiration pneumonia. Aging Dis. 2014; 6:27–37. PMID: 25657850.
Article31. Druschky A, Herkert M, Radespiel-Troger M, Druschky K, Hund E, Becker CM, et al. Critical illness polyneuropathy: clinical findings and cell culture assay of neurotoxicity assessed by a prospective study. Intensive Care Med. 2001; 27:686–693. PMID: 11398694.
Article32. De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002; 288:2859–2867. PMID: 12472328.33. Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014; 370:1626–1635. PMID: 24758618.
Article34. Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, et al. Diagnosis and treatment of postextubation dysphagia: results from a national survey. J Crit Care. 2012; 27:578–586. PMID: 23084136.
Article35. McCullough GH, Wertz RT, Rosenbek JC, Mills RH, Ross KB, Ashford JR. Inter- and intrajudge reliability of a clinical examination of swallowing in adults. Dysphagia. 2000; 15:58–67. PMID: 10758187.
Article36. Ramsey DJ, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003; 34:1252–1257. PMID: 12677020.
Article37. Brodsky MB, Gonzalez-Fernandez M, Mendez-Tellez PA, Shanholtz C, Palmer JB, Needham DM. Factors associated with swallowing assessment after oral endotracheal intubation and mechanical ventilation for acute lung injury. Ann Am Thorac Soc. 2014; 11:1545–1552. PMID: 25387319.
Article38. Pikus L, Levine MS, Yang YX, Rubesin SE, Katzka DA, Laufer I, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol. 2003; 180:1613–1616. PMID: 12760930.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Post-extubation Dysphagia With Tongue Weakness and Somatosensory Disturbance in Non-neurologic Critically Ill Patients
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- The Comparison of Dysphagia between COVID-19 Pneumonia and Aspiration Pneumonia
- Association between clinical risk factors and severity of dysphagia after extubation based on a videofluoroscopic swallowing study
- Strategies of Oral Hygiene Care for Prevention of Aspiration Pneumonia in Dysphasia Patients