Allergy Asthma Immunol Res.
2011 Apr;3(2):141-144. 10.4168/aair.2011.3.2.141.
A Case of Autoimmune Progesterone Dermatitis Misdiagnosed as Allergic Contact Dermatitis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. sanghakim@yonsei.ac.kr
- KMID: 2130369
- DOI: http://doi.org/10.4168/aair.2011.3.2.141
Abstract
- Autoimmune progesterone dermatitis is a rare autoimmune response to endogenous progesterone that usually occurs in fertile females. Cutaneous or mucosal lesions develop cyclically during the luteal phase of the menstrual cycle when progesterone levels are elevated. Symptoms usually start 3-10 days before menstruation and resolve 1-2 days after menstruation ceases. We report the case of a 48-year-old woman with intermittent eczematous skin lesions of the legs, forearms, and buttocks. She was diagnosed with allergic contact dermatitis, and topical steroids were prescribed. Her skin eruptions waxed and waned for 6 years and were associated with her menstrual cycle. We performed an intradermal test using progesterone, which was positive, and prescribed gonadotropin-releasing hormone analogues monthly for 3 months. The patient's skin lesions improved, confirming the diagnosis. Autoimmune progesterone dermatitis should be included in the differential diagnosis of recurrent eczema that is refractory to treatment in women of child-bearing age.
Keyword
MeSH Terms
-
Autoimmune Diseases
Autoimmunity
Buttocks
Dermatitis
Dermatitis, Allergic Contact
Diagnosis, Differential
Eczema
Female
Forearm
Gonadotropin-Releasing Hormone
Humans
Intradermal Tests
Leg
Luteal Phase
Menstrual Cycle
Menstruation
Middle Aged
Progesterone
Skin
Steroids
Autoimmune Diseases
Gonadotropin-Releasing Hormone
Progesterone
Steroids
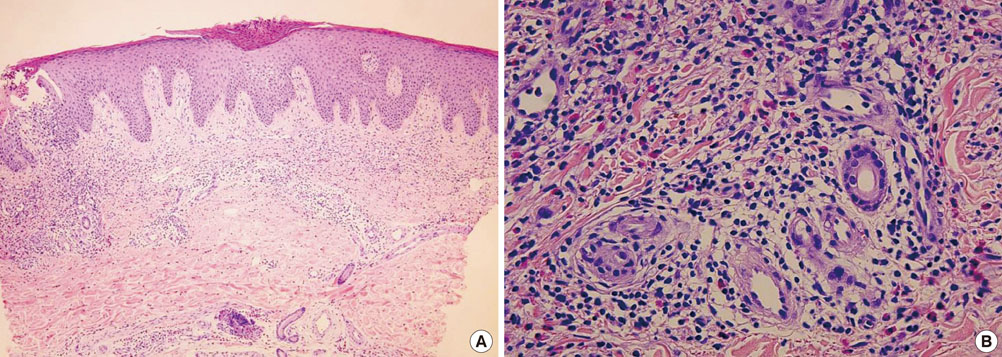
Figure
Cited by 1 articles
-
A case of oral desensitization for hypersensitivity to exogenous progesterone
Young-Chan Kim, Kook-Hwan Choi, Dong-Yoon Kang, Kyung Hee Sohn, Sang-Heon Cho, Kyung-Up Min, Hye-Ryun Kang
Allergy Asthma Respir Dis. 2017;5(5):294-297. doi: 10.4168/aard.2017.5.5.294.
Reference
-
1. Géber H. IV. Einige Daten zur Pathologie der Urticaria menstruationalis. Dermatologische Zeitschrift. 1921. 32:143–150.2. Snyder JL, Krishnaswamy G. Autoimmune progesterone dermatitis and its manifestation as anaphylaxis: a case report and literature review. Ann Allergy Asthma Immunol. 2003. 90:469–477.3. Hur W, Chun SI. Autoimmune progesterone dermatitis. Korean J Dermatol. 1993. 31:775–779.4. Lee CW, Yoon KB, Yi JU, Cho SH. Autoimmune progesterone dermatitis. J Dermatol. 1992. 19:629–631.5. Wilkinson SM, Beck MH, Kingston TP. Progesterone-induced urticaria--need it be autoimmune? Br J Dermatol. 1995. 133:792–794.6. Schoenmakers A, Vermorken A, Degreef H, Dooms-Goossens A. Corticosteroid or steroid allergy? Contact Dermatitis. 1992. 26:159–162.7. Mittman RJ, Bernstein DI, Steinberg DR, Enrione M, Bernstein IL. Progesterone-responsive urticaria and eosinophilia. J Allergy Clin Immunol. 1989. 84:304–310.8. Baptist AP, Baldwin JL. Autoimmune progesterone dermatitis in a patient with endometriosis: case report and review of the literature. Clin Mol Allergy. 2004. 2:10.9. Hart R. Autoimmune progesterone dermatitis. Arch Dermatol. 1977. 113:426–430.10. Miura T, Matsuda M, Yanbe H, Sugiyama S. Two cases of autoimmune progesterone dermatitis. Immunohistochemical and serological studies. Acta Derm Venereol. 1989. 69:308–310.11. Shelley WB, Preucel RW, Spoont SS. Autoimmune progesterone dermatitis. Cure by oophorectomy. JAMA. 1964. 190:35–38.12. Burstein M, Rubinow A, Shalit M. Cyclic anaphylaxis associated with menstruation. Ann Allergy. 1991. 66:36–38.13. Belsito DV. The diagnostic evaluation, treatment, and prevention of allergic contact dermatitis in the new millennium. J Allergy Clin Immunol. 2000. 105:409–420.14. Warin AP. Case 2. Diagnosis: erythema multiforme as a presentation of autoimmune progesterone dermatitis. Clin Exp Dermatol. 2001. 26:107–108.15. Stephens CJ, Wojnarowska FT, Wilkinson JD. Autoimmune progesterone dermatitis responding to Tamoxifen. Br J Dermatol. 1989. 121:135–137.16. Yee KC, Cunliffe WJ. Progesterone-induced urticaria: response to buserelin. Br J Dermatol. 1994. 130:121–123.17. Ródenas JM, Herranz MT, Tercedor J. Autoimmune progesterone dermatitis: treatment with oophorectomy. Br J Dermatol. 1998. 139:508–511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Cases of Autoimmune Progesterone Dermatitis
- A Case of Irritant Contact Dermafitis Due to Ranuculus japonicus
- Allergic Contact Dermatitis Caused by a Hearing Aid
- A Case of Allergic Contact Dermatitis due to Primula obconica
- A Case of Allergic Contact Dermatitis Caused by Topical Hydrocortisone Cream