Analysis of Anesthesia-related Medical Disputes in the 2009-2014 Period Using the Korean Society of Anesthesiologists Database
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, The Catholic University of Daegu, Daegu, Korea.
- 2Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dikei@hanmail.net
- 3Department of Anesthesiology and Pain Medicine, School of Dentistry, Kyungpook National University, Daegu, Korea.
- 4Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 5Department of Anesthesiology and Pain Medicine, College of Medicine, Dong-A University, Busan, Korea.
- 6Department of Anesthesiology and Pain Medicine, College of Medicine, Chungnam National University, Daejeon, Korea.
- 7Department of Anesthesiology and Pain Medicine, School of Medicine, Keimyung University, Daegu, Korea.
- KMID: 2129653
- DOI: http://doi.org/10.3346/jkms.2015.30.2.207
Abstract
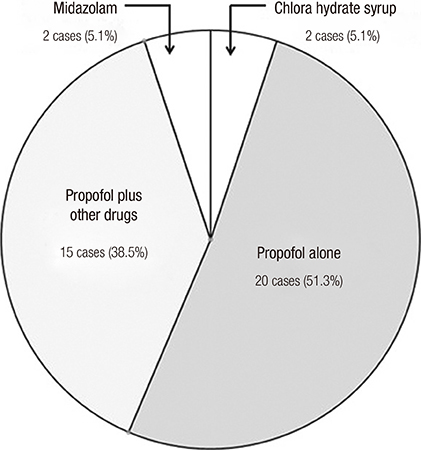
- Using the Korean Society of Anesthesiologists database of anesthesia-related medical disputes (July 2009-June 2014), causative mechanisms and injury patterns were analyzed. In total, 105 cases were analyzed. Most patients were aged < 60 yr (82.9%) and were classified as American Society of Anesthesiologists physical status < or = II (90.5%). In 42.9% of all cases, the injuries were determined to be 'avoidable' if the appropriate standard of care had been applied. Sedation was the sec most common type of anesthesia (37.1% of all cases), following by general anesthesia. Most sedation cases (27/39, 69.2%) showed a common lack of vigilance: no pre-procedural testing (82.1%), absence of anesthesia record (89.7%), and non-use of intra-procedural monitoring (15.4%). Most sedation (92.3%) was provided simultaneously by the non-anesthesiologists who performed the procedures. After the resulting injuries were grouped into four categories (temporary, permanent/minor, permanent/major, and death), their causative mechanisms were analyzed in cases with permanent injuries (n=20) and death (n=82). A 'respiratory events' was the leading causative mechanism (56/102, 54.9%). Of these, the most common specific mechanism was hypoxia secondary to airway obstruction or respiratory depression (n=31). The sec most common damaging event was a 'cardiovascular events' (26/102, 25.5%), in which myocardial infarction was the most common specific mechanism (n=12). Our database analysis demonstrated several typical injury profiles (a lack of vigilance in seemingly safe procedures or sedation, non-compliance with the airway management guidelines, and the prevalence of myocardial infarction) and can be helpful to improve patient safety.
Keyword
MeSH Terms
Figure
Cited by 9 articles
-
Preparation, Evaluation, and Recovery before and after Conscious Sedative Endoscopy
Hong Jun Park, Byoung Kwan Son, Hoon Sup Koo, Byung-Wook Kim
Korean J Gastroenterol. 2017;69(1):59-63. doi: 10.4166/kjg.2017.69.1.59.Analysis of closed medical litigation in urology
Su Hwan Shin, So Yoon Kim, Seung Gyeong Jang, Won Lee
Investig Clin Urol. 2017;58(5):317-323. doi: 10.4111/icu.2017.58.5.317.Sedation in Pediatric Esophagogastroduodenoscopy
Seak Hee Oh
Clin Endosc. 2018;51(2):120-128. doi: 10.5946/ce.2018.028.Sedation for Gastrointestinal Endoscopy: Practical Issues in Patient Safety and Quality Management
Seung Bae Yoon, Young-Seok Cho
Clin Endosc. 2016;49(1):1-3. doi: 10.5946/ce.2016.49.1.1.Anesthesia and sedation outside of the operating room
Ann Misun Youn, Young-Kwon Ko, Yoon-Hee Kim
Korean J Anesthesiol. 2015;68(4):323-331. doi: 10.4097/kjae.2015.68.4.323.Practice guidelines for propofol sedation by non-anesthesiologists: the Korean Society of Anesthesiologists Task Force recommendations on propofol sedation
Hyun Kang, Duk Kyung Kim, Yong-Seon Choi, Young-Chul Yoo, Hyun Sik Chung
Korean J Anesthesiol. 2016;69(6):545-554. doi: 10.4097/kjae.2016.69.6.545.Analysis of endotracheal intubation-related judicial precedents in South Korea
Hye-Yeon Cho, SuHwan Shin, SangJin Lee, Susie Yoon, Ho-Jin Lee
Korean J Anesthesiol. 2021;74(6):506-513. doi: 10.4097/kja.21020.Difficult intubation: lessons learned from the courts of South Korea
Jae Hoon Lee
Korean J Anesthesiol. 2021;74(6):463-464. doi: 10.4097/kja.21448.Trends in medical disputes involving anesthesia during July 2009–June 2018: an analysis of the Korean Society of Anesthesiologists database
Ji Won Choi, Duk Kyung Kim, Choon Kyu Cho, Soo Jung Park, Yong Hun Son
Korean J Anesthesiol. 2019;72(2):156-163. doi: 10.4097/kja.d.18.00198.
Reference
-
1. Cheney FW. The American Society of Anesthesiologists Closed Claims Project: what have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999; 91:552–556.2. Cheney FW, Posner KL, Lee LA, Caplan RA, Domino KB. Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology. 2006; 105:1081–1086.3. Lee KH, An TH, Choi JH, Lim DG, Lee YJ, Kim DK. Analysis of expert consultation referrals for anesthesia-related issues (December 2008-July 2010): KSA legislation committee report. Korean J Anesthesiol. 2011; 60:260–265.4. Hong SJ, Kang YJ, Jeon YH, Son JS, Song JH, Yoo CS, Kim DK. Analysis of expert consultation referrals to the Korean Society of Anesthesiologists (KSA): a comparison of procedural sedation and general anesthesia. J Anesth. 2013; 27:218–223.5. Posner KL, Sampson PD, Caplan RA, Ward RJ, Cheney FW. Measuring interrater reliability among multiple raters: an example of methods for nominal data. Stat Med. 1990; 9:1103–1115.6. Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Lee LA, Goodkin R. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Musculoskelet Disord. 2006; 7:53.7. Kim YH, Hwang CJ. Patterns of medical accidents and disputes in the orthodontic field in Korea. Korean J Orthod. 2014; 44:5–12.8. Kwon MI. The analysis of 137 anesthesia-related adverse outcome cases in Korea. Korean J Anesthesiol. 2004; 46:83–90.9. Perel A. Non-anaesthesiologists should not be allowed to administer propofol for procedural sedation: a Consensus Statement of 21 European National Societies of Anaesthesia. Eur J Anaesthesiol. 2011; 28:580–584.10. American Society of Anesthesiologists. Standards, Guidelines, Statements and Other Documents: UPDATED - Monitored Anesthesia Care, Position on (2013). accessed on 7 June 2014. Available at https://www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx.11. Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S, Dominitz JA, Fanelli RD, Gan SI, Harrison ME, et al. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008; 68:815–826.12. Iverson RE. Sedation and analgesia in ambulatory settings. American Society of Plastic and Reconstructive Surgeons. Task Force on Sedation and Analgesia in Ambulatory Settings. Plast Reconstr Surg. 1999; 104:1559–1564.13. Godwin SA, Caro DA, Wolf SJ, Jagoda AS, Charles R, Marett BE, Moore J. American College of Emergency Physicians. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2005; 45:177–196.14. American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003; 98:1269–1277.15. Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004; 99:607–613.16. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005; 103:33–39.17. American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011; 114:495–511.18. Bartels K, Karhausen J, Clambey ET, Grenz A, Eltzschig HK. Perioperative organ injury. Anesthesiology. 2013; 119:1474–1489.19. Eagle KA, Berger PB, Calkins H, Chaitman BR, Ewy GA, Fleischmann KE, Fleisher LA, Froehlich JB, Gusberg RJ, Leppo JA, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery---executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation. 2002; 105:1257–1267.20. Kim RB, Kim BG, Kim YM, Seo JW, Lim YS, Kim HS, Lee HJ, Moon JY, Kim KY, Shin JY, et al. Trends in the incidence of hospitalized acute myocardial infarction and stroke in Korea, 2006-2010. J Korean Med Sci. 2013; 28:16–24.21. Matsusaki T, Sakai T. The role of certified registered nurse anesthetists in the United States. J Anesth. 2011; 25:734–740.22. Cook TM, Bland L, Mihai R, Scott S. Litigation related to anaesthesia: an analysis of claims against the NHS in England 1995-2007. Anaesthesia. 2009; 64:706–718.23. Garnick DW, Hendricks AM, Brennan TA. Can practice guidelines reduce the number and costs of malpractice claims? JAMA. 1991; 266:2856–2860.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analysis of Anesthetic Legal Disputes between Older and Younger Patients Referred to the Korean Society of Anesthesiologists in 2009–2018
- Trends in medical disputes involving anesthesia during July 2009–June 2018: an analysis of the Korean Society of Anesthesiologists database
- Analysis of medical disputes regarding chronic pain management in the 2009–2016 period using the Korean Society of Anesthesiologists database
- The state of anesthesia in South Korea: a national survey of the status of anesthetic service activity in 2014–2016
- Easy sedation anesthesia guide for non-anesthetic medical personnel