Korean J Pain.
2014 Apr;27(2):133-138. 10.3344/kjp.2014.27.2.133.
Survey of Sonoanatomic Distances For Lumbar Medial Branch Nerve Blocks in Healthy Volunteers
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Boali Hospital, Tehran, Iran. helengharaee@yahoo.com
- 2Department of Anesthesiology and Pain Medicine, Rasoul-Akram Hospital, Tehran, Iran.
- 3Minimally Invasive Surgery Research Centre, Tehran University of Medical Sciences, Tehran, Iran.
- KMID: 2074059
- DOI: http://doi.org/10.3344/kjp.2014.27.2.133
Abstract
- BACKGROUND
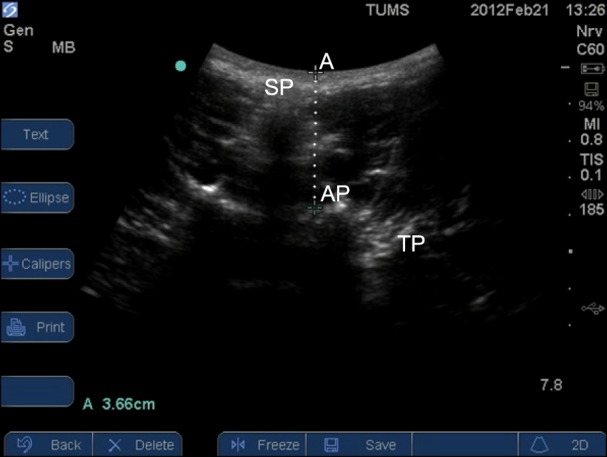
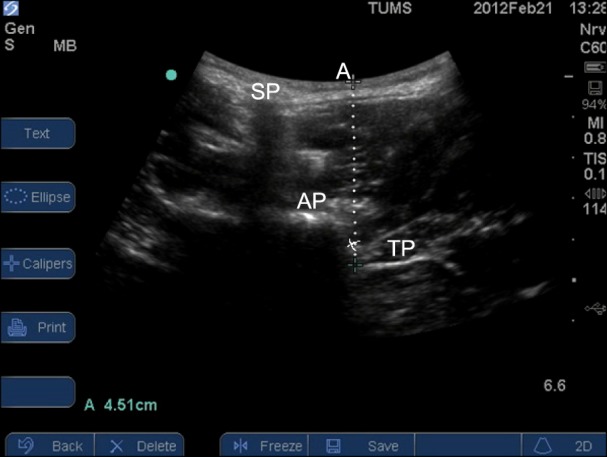
The precise knowledge of anatomy and the region of transverse process (TP) and superior articular processes (AP) and their distance from the skin are important in blocking and treating lumbar facet syndrome. Evaluation of these anatomic distances from 3rd and 5th lumbar vertebrae in both sides and in different body mass index (BMI) in healthy volunteers might improve knowledge of ultrasound (US) lumbar medial branch nerve blocks (LMBB).
METHODS
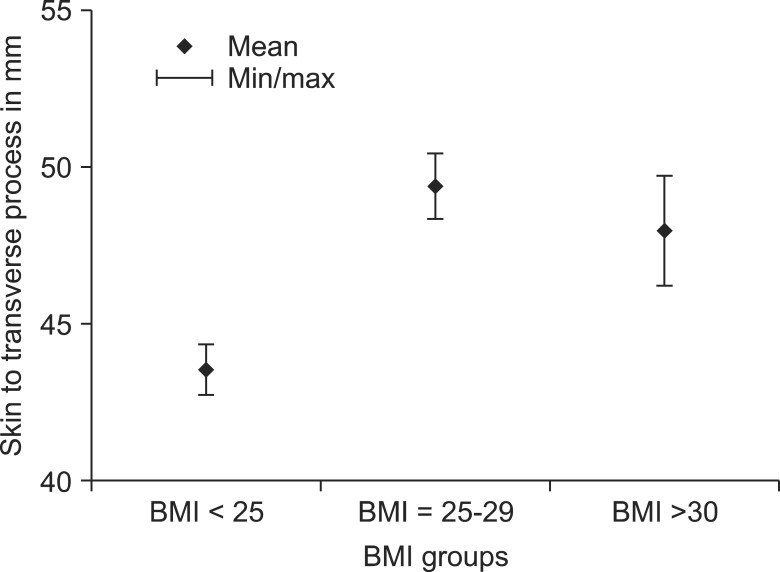
Bilateral US in the 3rd and 5th lumbar vertebrae of 64 volunteers carried out and the distance between skin to TP and skin to AP was measured. These distances were compared on both sides and in different BMI groups. The analysis was done using SPSS 11. Analysis of variance was used to compare the means at three vertebral levels (L3-L5) and different BMI groups. P values less than 0.05 were considered statistically significant. The paired t-test was used to compare the mean distance between skin to TP and skin to AP on both sides.
RESULTS
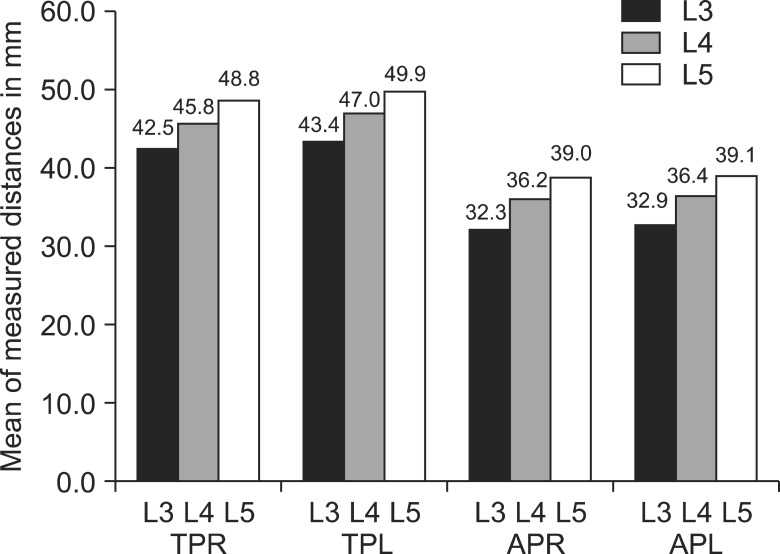
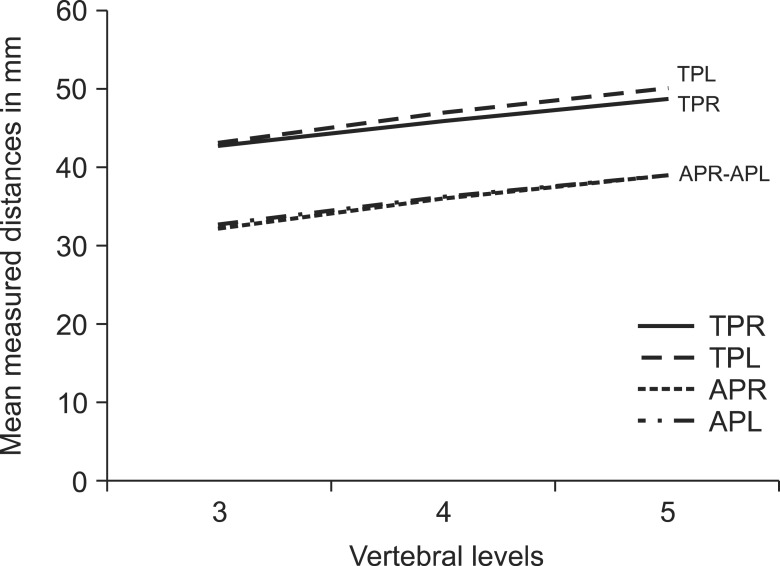
The distance between skin to TP and skin to AP of 3rd vertebrae to 5th vertebrae was increased in both right and left sides (P < 0.001) from up to down. The mean distance from skin to TP were greater on the left side compared to the right in all three vertebral levels from L3 to L5 (P values 0.014, 0.024, and 0.006 respectively). The mean distance from skin to TP and the skin to AP was statistically significant in different BMI groups (P < 0.001).
CONCLUSIONS
We found many anatomic distances which may increase awareness of US guided LMBB.
MeSH Terms
Figure
Reference
-
1. Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine (Phila Pa 1976). 2002; 27:2538–2545. PMID: 12435989.
Article2. Fujiwara Y, Komatsu T, Gofeld M. Ultrasound-guided lumbar (L1-L4) zygapophysial medial branch and L5 dorsal ramus block. In : Bigeleisen P, Orebaugh S, Moayeri N, Groen G, Breneman S, Chelly J, editors. Ultrasound-guided regional anesthesia and pain medicine. Philadelphia (PA): Lippincott Williams & Wilkin;2010. p. 240–251.3. Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007; 32:317–322. PMID: 17720116.
Article4. Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005; 24:33–38. PMID: 15615926.
Article5. Kirchmair L, Entner T, Wissel J, Moriggl B, Kapral S, Mitterschiffthaler G. A study of the paravertebral anatomy for ultrasound-guided posterior lumbar plexus block. Anesth Analg. 2001; 93:477–481. PMID: 11473883.
Article6. Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100:1242–1248. PMID: 15114223.7. Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Ultrasound guidance for facet joint injections in the lumbar spine: a computed tomography-controlled feasibility study. Anesth Analg. 2005; 101:579–583. PMID: 16037179.
Article8. Irwin DM, Gofeld M. Ultrasound-guided lumbar zygapophysial (Facet) nerve block. In : Narouze SN, editor. Atlas of ultrasound-guided procedures in interventional pain management. New York (NY): Springer;2011. p. 149–156.9. Shim JK, Moon JC, Yoon KB, Kim WO, Yoon DM. Ultrasound-guided lumbar medial-branch block: a clinical study with fluoroscopy control. Reg Anesth Pain Med. 2006; 31:451–454. PMID: 16952818.
Article10. Greher M, Kirchmair L, Enna B, Kovacs P, Gustorff B, Kapral S, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004; 101:1195–1200. PMID: 15505456.11. Rauch S, Kasuya Y, Turan A, Neamtu A, Vinayakan A, Sessler DI. Ultrasound-guided lumbar medial branch block in obese patients: a fluoroscopically confirmed clinical feasibility study. Reg Anesth Pain Med. 2009; 34:340–342. PMID: 19585701.12. Moon JC, Shim JK, Jo KY, Yoon KB, Kim WO, Yoon DM. Ultrasound-guided distance measurements of vertebral structures for lumbar medial branch block. Korean J Pain. 2007; 20:111–115.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonoanatomic Variation of Pes Anserine Bursa
- Determination of the False Positive Rate of Uncontrolled Diagnostic Block for Lumbar Medial Branch of Dorsal Rami
- Ultrasonographic Finding of the Ulnar Nerve with Change of Elbow Joint
- Transverse Process and Needles of Medial Branch Block to Facet Joint as Landmarks for Ultrasound-Guided Selective Nerve Root Block
- Motor Innervation and Nerve Pathway of Glabellar Expression Muscles