Clin Orthop Surg.
2013 Mar;5(1):44-48. 10.4055/cios.2013.5.1.44.
Transverse Process and Needles of Medial Branch Block to Facet Joint as Landmarks for Ultrasound-Guided Selective Nerve Root Block
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kwangju Christian Hospital, Gwangju, Korea. stemcellchoi@hanmail.net
- KMID: 1402325
- DOI: http://doi.org/10.4055/cios.2013.5.1.44
Abstract
- BACKGROUND
Selective lumbar nerve root block (SNRB) is generally accepted as an effective treatment method for back pain with sciatica. However, it requires devices producing radioactive materials such as C-arm fluoroscopy. This study evaluated the usefulness of the longitudinal view of transverse process and needles for medial branch block as landmarks under ultrasonography.
METHODS
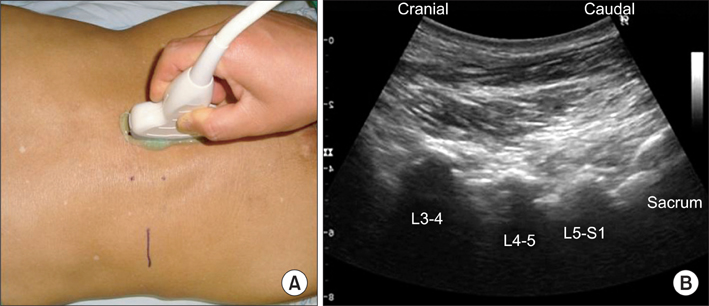
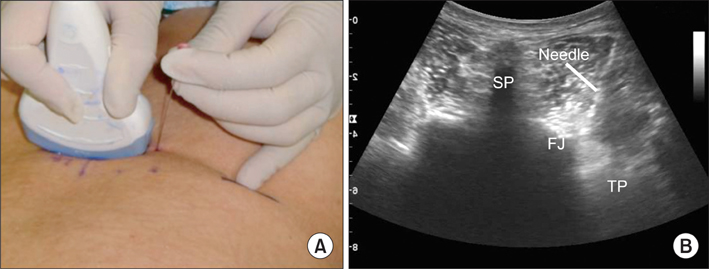
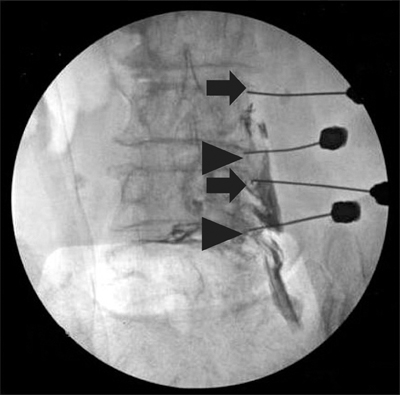
We performed selective nerve root block for 96 nerve roots in 61 patients under the guidance of ultrasound. A curved probe was used to identify the facet joints and transverse processes. Identifying the lumbar nerve roots under the skin surface and ultrasound landmarks, the cephalad and caudal medial branch blocks were undertaken under the transverse view of sonogram first. A needle for nerve root block was inserted between the two transverse processes under longitudinal view, while estimating the depth with the needle for medial branch block. We then injected 1.0 mL of contrast medium and checked the distribution of the nerve root with C-arm fluoroscopy to evaluate the accuracy. The visual analog scale (VAS) was used to access the clinical results.
RESULTS
Seven SNRBs were performed for the L2 nerve root, 15 for L3, 49 for L4, and 25 for L5, respectively. Eighty-six SNRBs (89.5%) showed successful positioning of the needles. We failed in the following cases: 1 case for the L2 nerve root; 2 for L3; 3 for L4; and 4 for L5. The failed needles were positioned at wrong leveled segments in 4 cases and inappropriate place in 6 cases. VAS was improved from 7.6 +/- 0.6 to 3.5 +/- 1.3 after the procedure.
CONCLUSIONS
For SNRB in lumbar spine, the transverse processes under longitudinal view as the ultrasound landmark and the needles of medial branch block to the facet joint can be a promising guidance.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Ultrasound-Guided Intervention in Lumbar Spine
Yong-Soo Choi, Ju-Yeong Heo
J Korean Orthop Assoc. 2015;50(2):107-115. doi: 10.4055/jkoa.2015.50.2.107.
Reference
-
1. Sato M, Simizu S, Kadota R, Takahasi H. Ultrasound and nerve stimulation-guided L5 nerve root block. Spine (Phila Pa 1976). 2009. 34(24):2669–2673.2. Riew KD, Park JB, Cho YS, et al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five-year follow-up. J Bone Joint Surg Am. 2006. 88(8):1722–1725.3. Gray AT. Ultrasound-guided regional anesthesia: current state of the art. Anesthesiology. 2006. 104(2):368–373.4. Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005. 94(1):7–17.5. Peterson MK, Millar FA, Sheppard DG. Ultrasound-guided nerve blocks. Br J Anaesth. 2002. 88(5):621–624.6. Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994. 78(3):507–513.7. Loizides A, Gruber H, Peer S, Brenner E, Galiano K, Obernauer J. A new simplified sonographic approach for pararadicular injections in the lumbar spine: a CT-controlled cadaver study. AJNR Am J Neuroradiol. 2011. 32(5):828–831.8. Chumnanvej S, Wetchagama N, Kounsongtham V. Accuracy of needle-tip localization by ultrasound guidance lumbar selective nerve root block: a prospective clinical study of 78 lumbar nerve roots block. J Med Assoc Thai. 2011. 94(12):1451–1456.9. Riew KD, Yin Y, Gilula L, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000. 82(11):1589–1593.10. Watson-Jones R. Fracture and joint injuries. 1982. New York: Churchill Livingstone;278–279.11. Lee EW, Chun JM, Ahn BW, Park YW, Lee SY, Paik NC. A study of hand lesion exposed by radiation. J Korean Orthop Assoc. 1991. 26(3):841–846.12. Hashimoto BE, Kramer DJ, Wiitala L. Applications of musculoskeletal sonography. J Clin Ultrasound. 1999. 27(6):293–318.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Validation of Ultrasound-Guided Lumbar Facet Nerve Blocks as Confirmed by Fluoroscopy
- Ultrasound Guided Therapeutic Medial Branch Block for the Facet Joint Pain
- Effect of Ultrasound-guided Lumbar Medial Branch Block in Chronic Low Back Pain
- Spinal interventions under ultrasound guidance
- Ultrasound-guided Distance Measurements of Vertebral Structures for Lumbar Medial Branch Block