Korean J Pain.
2013 Jul;26(3):255-264. 10.3344/kjp.2013.26.3.255.
The Effects of Pre-emptive Administration of Ketamine and norBNI on Pain Behavior, c-Fos, and Prodynorphin Protein Expression in the Rat Spinal Cord after Formalin-induced Pain Is Modulated by the DREAM Protein
- Affiliations
-
- 1BRAINetwork Centre for Neurocognitive Science, School of Health Sciences, Health Campus, Universiti Sains Malaysia, Kelantan, Malaysia. idris@kk.usm.my
- KMID: 2074026
- DOI: http://doi.org/10.3344/kjp.2013.26.3.255
Abstract
- BACKGROUND
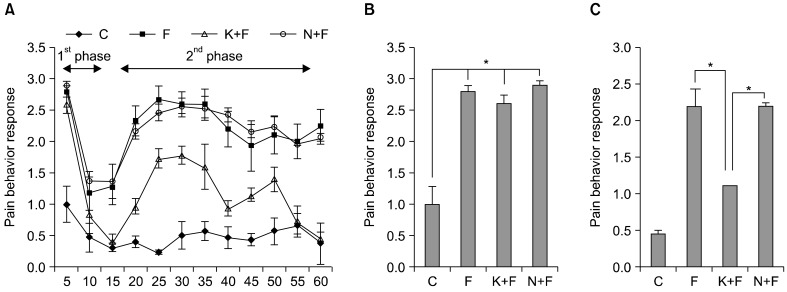
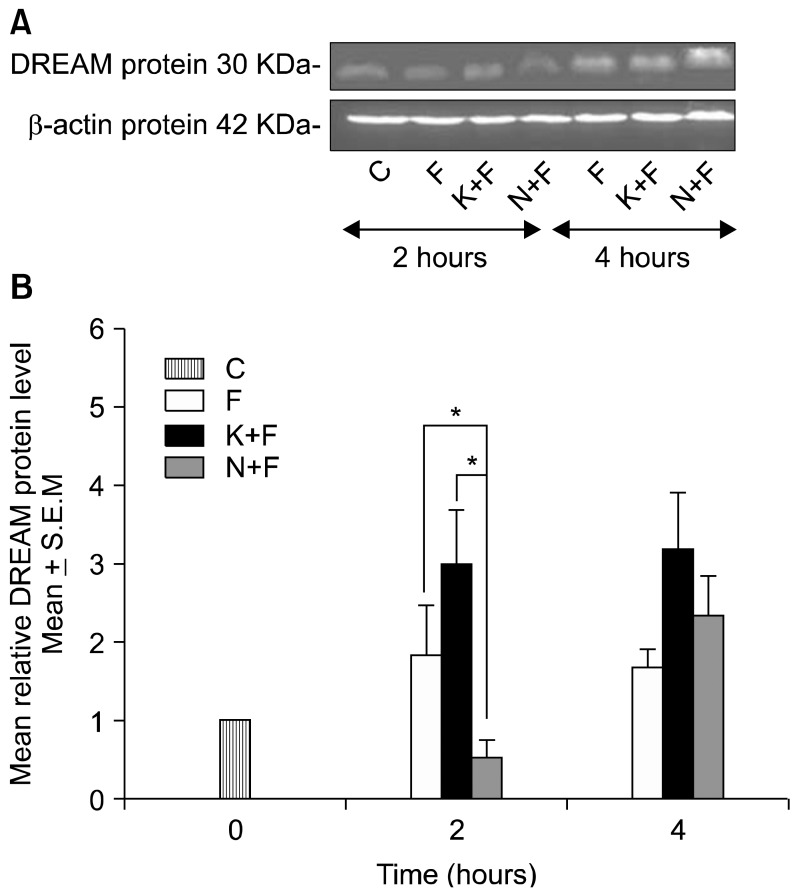
We investigated the effects of pre-emptive administration of ketamine and norBNI on pain behavior and the expression of DREAM, c-Fos, and prodynorphin proteins on the ipsilateral side of the rat spinal cord at 2 and 4 hours after formalin injection.
METHODS
Eighty-four male Sprague Dawley rats were divided into 4 major groups consisting of control rats (C) (n = 12), rats given only formalin injections (F) (n = 24), and rats treated with pre-emptive administration of either ketamine (K+F) (n = 24) or norBNI (N+F) (n = 24). The non-control groups were further divided into subgroups consisting of rats that were sacrificed at 2 and 4 hours (n = 12 for each group) after formalin injection. Pain behavior was recorded for 1 hour. After 2 and 4 hours, the rats were sacrificed and the spinal cords (L4-L5 sections) were removed for immunohistochemistry and Western blot analysis.
RESULTS
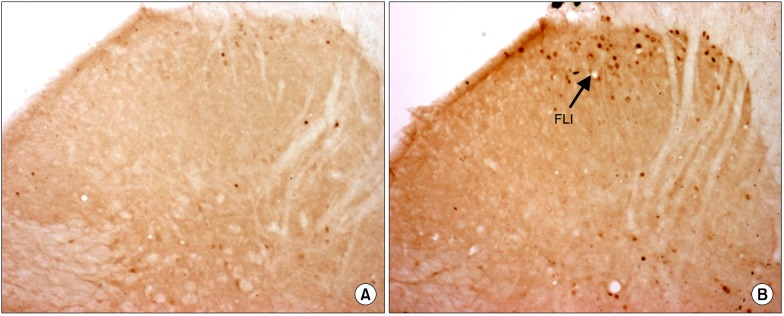
The pain behavior response was reduced in the K+F group compared to the other groups during the second phase of the formalin pain response. We detected an increase in the nuclear DREAM protein level in the K+F group at 2 and 4 hours and a transient decrease in the N+F group at 2 hours; however, it increased at 4 hours after injection. Fos-like immunoreactivity (FLI) and Prodynorphin-like immunoreactivity (PLI) neurons decreased in the K+F group but increased in the N+F group at 2 hours after injection. While FLI decreased, PLI increased in all groups at 4 hours after injection.
CONCLUSIONS
We suggest that NMDA and kappa opioid receptors can modulate DREAM protein expression, which can affect pain behavior and protein transcriptional processes at 2 hours and bring about either harmful or protective effects at 4 hours after formalin injection.
MeSH Terms
-
Animals
Blotting, Western
Enkephalins
Formaldehyde
Humans
Immunohistochemistry
Ketamine
Male
N-Methylaspartate
Neurons
Pain Measurement
Protein Precursors
Proteins
Rats
Rats, Sprague-Dawley
Receptors, Opioid, kappa
Spinal Cord
Enkephalins
Formaldehyde
Ketamine
N-Methylaspartate
Protein Precursors
Proteins
Receptors, Opioid, kappa
Figure
Reference
-
1. Carrión AM, Link WA, Ledo F, Mellström B, Naranjo JR. DREAM is a Ca2+-regulated transcriptional repressor. Nature. 1999; 398:80–84. PMID: 10078534.
Article2. Cheng HY, Pitcher GM, Laviolette SR, Whishaw IQ, Tong KI, Kockeritz LK, et al. DREAM is a critical transcriptional repressor for pain modulation. Cell. 2002; 108:31–43. PMID: 11792319.
Article3. Lilliehook C, Bozdagi O, Yao J, Gomez-Ramirez M, Zaidi NF, Wasco W, et al. Altered Abeta formation and long-term potentiation in a calsenilin knock-out. J Neurosci. 2003; 23:9097–9106. PMID: 14534243.4. Obara I, Mika J, Schafer MK, Przewlocka B. Antagonists of the kappa-opioid receptor enhance allodynia in rats and mice after sciatic nerve ligation. Br J Pharmacol. 2003; 140:538–546. PMID: 12970097.
Article5. Sevostianova N, Danysz W, Bespalov AY. Analgesic effects of morphine and loperamide in the rat formalin test: interactions with NMDA receptor antagonists. Eur J Pharmacol. 2005; 525:83–90. PMID: 16297905.
Article6. Snijdelaar DG, van Rijn CM, Vinken P, Meert TF. Effects of pre-treatment with amantadine on morphine induced antinociception during second phase formalin responses in rats. Pain. 2005; 119:159–167. PMID: 16297559.
Article7. Fukuda T, Nishimoto C, Shiga Y, Toyooka H. The formalin test: effects of formalin concentration and short-term halothane inhalation. Reg Anesth Pain Med. 2001; 26:407–413. PMID: 11561259.
Article8. Lee IO, Jeong YS. Effects of different concentrations of formalin on paw edema and pain behaviors in rats. J Korean Med Sci. 2002; 17:81–85. PMID: 11850594.
Article9. Kim MJ, Hong BH, Zhang EJ, Ko YK, Lee WH. Antinociceptive effects of intraperitoneal and intrathecal vitamin E in the rat formalin test. Korean J Pain. 2012; 25:238–244. PMID: 23091684.
Article10. Hayati AA, Zalina I, Myo T, Badariah AA, Azhar A, Idris L. Modulation of formalin-induced fos-like immunoreactivity in the spinal cord by swim stress-induced analgesia, morphine and ketamine. Ger Med Sci. 2008; 6:Doc05. PMID: 19675733.11. Grossman A, Clement-Jones V. Opiate receptors: enkephalins and endorphins. Clin Endocrinol Metab. 1983; 12:31–56. PMID: 6303648.12. Horan P, Taylor J, Yamamura HI, Porreca F. Extremely long-lasting antagonistic actions of nor-binaltorphimine (nor-BNI) in the mouse tail-flick test. J Pharmacol Exp Ther. 1992; 260:1237–1243. PMID: 1312164.13. Spanagel R, Almeida OF, Shippenberg TS. Evidence thatnor-binaltorphimine can function as an antagonist at multiple opioid receptor subtypes. Eur J Pharmacol. 1994; 264:157–162. PMID: 7851478.
Article14. Endoh T, Matsuura H, Tanaka C, Nagase H. Nor-binaltorphimine: a potent and selective kappa-opioid receptor antagonist with long-lasting activity in vivo. Arch Int Pharmacodyn Ther. 1992; 316:30–42. PMID: 1326932.15. Broadbear JH, Negus SS, Butelman ER, de Costa BR, Woods JH. Differential effects of systemically administered nor-binaltorphimine (nor-BNI) on kappa-opioid agonists in the mouse writhing assay. Psychopharmacology (Berl). 1994; 115:311–319. PMID: 7871070.
Article16. Dubuisson D, Dennis SG. The formalin test: a quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain. 1977; 4:161–174. PMID: 564014.
Article17. Hao S, Takahata O, Mamiya K, Iwasaki H. Sevoflurane suppresses noxious stimulus-evoked expression of Fos-like immunoreactivity in the rat spinal cord via activation of endogenous opioid systems. Life Sci. 2002; 71:571–580. PMID: 12052441.
Article18. Molander C, Xu Q, Grant G. The cytoarchitectonic organization of the spinal cord in the rat. I. The lower thoracic and lumbosacral cord. J Comp Neurol. 1984; 230:133–141. PMID: 6512014.
Article19. Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci U S A. 1979; 76:4350–4354. PMID: 388439.
Article20. Berrino L, Oliva P, Massimo F, Aurilio C, Maione S, Grella A, et al. Antinociceptive effect in mice of intraperitoneal N-methyl-D-aspartate receptor antagonists in the formalin test. Eur J Pain. 2003; 7:131–137. PMID: 12600794.
Article21. Ossipov MH, Kovelowski CJ, Wheeler-Aceto H, Cowan A, Hunter JC, Lai J, et al. Opioid antagonists and antisera to endogenous opioids increase the nociceptive response to formalin: demonstration of an opioid kappa and delta inhibitory tone. J Pharmacol Exp Ther. 1996; 277:784–788. PMID: 8627559.22. Coderre TJ, Fundytus ME, McKenna JE, Dalal S, Melzack R. The formalin test: a validation of the weighted-scores method of behavioural pain rating. Pain. 1993; 54:43–50. PMID: 8378102.
Article23. Wu HE, Hung KC, Mizoguchi H, Nagase H, Tseng LF. Roles of endogenous opioid peptides in modulation of nocifensive response to formalin. J Pharmacol Exp Ther. 2002; 300:647–654. PMID: 11805228.
Article24. Choi SS, Han KJ, Lee HK, Han EJ, Suh HW. Possible antinociceptive mechanisms of opioid receptor antagonists in the mouse formalin test. Pharmacol Biochem Behav. 2003; 75:447–457. PMID: 12873637.
Article25. Ikeda H, Stark J, Fischer H, Wagner M, Drdla R, Jäger T, et al. Synaptic amplifier of inflammatory pain in the spinal dorsal horn. Science. 2006; 312:1659–1662. PMID: 16778058.
Article26. Ledo F, Carrión AM, Link WA, Mellström B, Naranjo JR. DREAM-alphaCREM interaction via leucine-charged domains derepresses downstream regulatory element-dependent transcription. Mol Cell Biol. 2000; 20:9120–9126. PMID: 11094064.
Article27. Zaidi NF, Thomson EE, Choi EK, Buxbaum JD, Wasco W. Intracellular calcium modulates the nuclear translocation of calsenilin. J Neurochem. 2004; 89:593–601. PMID: 15086516.
Article28. Zhang Y, Li Y, Yang YR, Zhu HH, Han JS, Wang Y. Distribution of downstream regulatory element antagonist modulator (DREAM) in rat spinal cord and upregulation of its expression during inflammatory pain. Neurochem Res. 2007; 32:1592–1599. PMID: 17562172.
Article29. Long I, Suppian R, Ismail Z. Increases in mRNA and DREAM protein expression in the rat spinal cord after formalin induced pain. Neurochem Res. 2011; 36:533–539. PMID: 21188515.
Article30. Edling Y, Ingelman-Sundberg M, Simi A. Glutamate activates c-fos in glial cells via a novel mechanism involving the glutamate receptor subtype mGlu5 and the transcriptional repressor DREAM. Glia. 2007; 55:328–340. PMID: 17120244.
Article31. Chavira-Suárez E, Ramírez M, Lamas M. D-Serine/N-methyl-D-aspartate receptor signaling decreases DNA-binding activity of the transcriptional repressor DREAM in Müller glia from the retina. Neurosci Lett. 2008; 432:121–126. PMID: 18191896.
Article32. Coderre TJ, Melzack R. The role of NMDA receptor-operated calcium channels in persistent nociception after formalin-induced tissue injury. J Neurosci. 1992; 12:3671–3675. PMID: 1326611.
Article33. Lee J, Kim I, Oh SR, Ko SJ, Lim MK, Kim DG, et al. Regulation of DREAM expression by group I mGluR. Korean J Physiol Pharmacol. 2011; 15:95–100. PMID: 21660149.
Article34. Hunt SP, Pini A, Evan G. Induction of c-fos-like protein in spinal cord neurons following sensory stimulation. Nature. 1987; 328:632–634. PMID: 3112583.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preemptive Effect of Ketamine on Inflammatory Pain and Spinal c-fos Expression Induced by Formalin in the Rat
- The Effects of Intrathecal Ketamine Isomers on Formalin-Evoked Behavior and Spinal c-fos Expression in Rat
- Spinal c-fos Expression in a Rat Model of Incisional Pain
- Changes of c-Fos Immunoreactivity in Rat Brain Neurons According to Ages After Induced Pain
- Effects of Naloxone on Morphine Analgesia and Spinal c-fos Expression in Rat Formalin Test