Yonsei Med J.
2015 Mar;56(2):535-542. 10.3349/ymj.2015.56.2.535.
Selective Spinal Anesthesia Using 1 mg of Bupivacaine with Opioid in Elderly Patients for Transurethral Resection of Prostate
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Severance Hospital, Seoul, Korea. hkkil@yuhs.ac
- 2Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2070035
- DOI: http://doi.org/10.3349/ymj.2015.56.2.535
Abstract
- PURPOSE
This study was to evaluate the characteristics of selective spinal anesthesia using 1 mg of bupivacaine combined with fentanyl or sufentanil in elderly patients undergoing transurethral resection of prostate.
MATERIALS AND METHODS
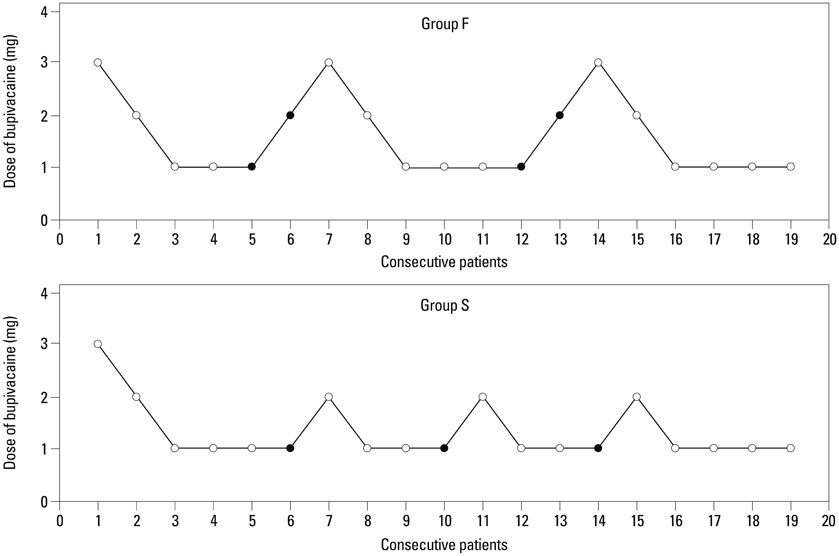
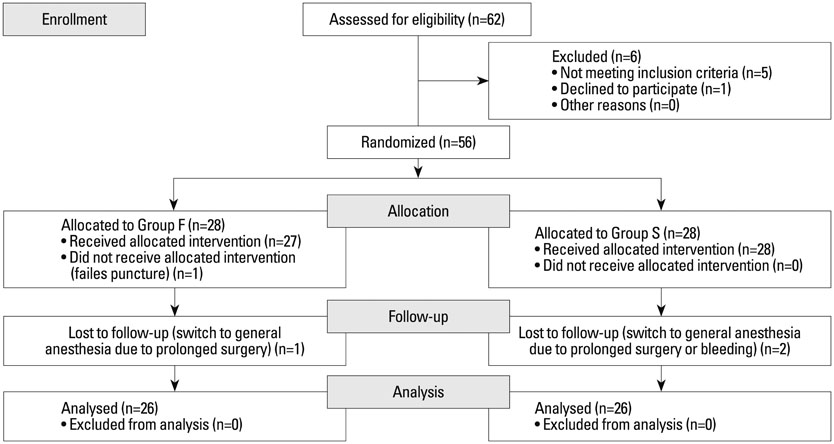
Fifty-six patients were randomized into two groups. The Fentanyl group received 0.5% hyperbaric bupivacaine 0.2 mL+fentanyl 20 microg+5% dextrose 1.4 mL, and the Sufentanil group received 0.5% hyperbaric bupivacaine 0.2 mL+sufentanil 5 microg+5% dextrose 1.7 mL intrathecally. Intraoperative and postoperative characteristics were evaluated. Patient satisfaction was assessed postoperatively.
RESULTS
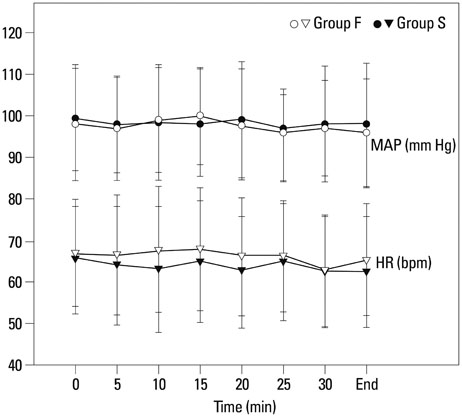
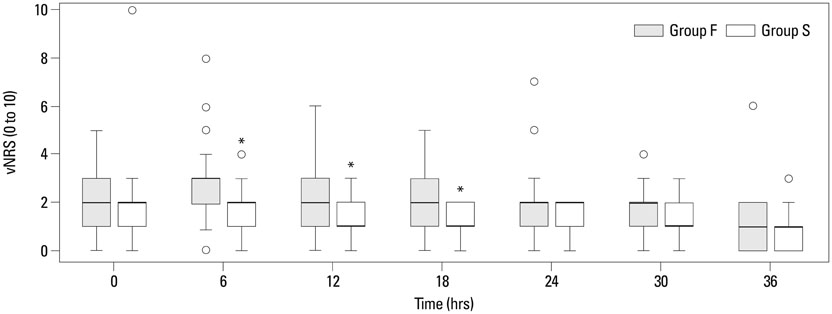
Twenty-six patients in each group completed the study. The median peak sensory block level was similar between two groups, but sensory regression time was longer in the Sufentanil group than the Fentanyl group (p=0.017). All patients were able to move themselves to the bed without any aid when they arrived at the admission room. Pain scores were lower in the Sufentanil group than the Fentanyl group at postoperative 6, 12, and 18 hours (p=0.001). Compared to the Fentanyl group, the Sufentanil group required less postoperative analgesia (p=0.023) and the time to the first analgesic request was longer (p=0.025). Twenty-four of 26 patients (92.3%) in each group showed "good" satisfaction level.
CONCLUSION
Selective spinal anesthesia using 1 mg of bupivacaine with fentanyl or sufentanil provided appropriate sensory block level with spared motor function for transurethral resection of the prostate in elderly patients. Intrathecal sufentanil was superior to fentanyl in postoperative analgesic quality.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Analgesics, Opioid/*administration & dosage
Anesthesia, Spinal/*methods
Anesthetics, Local/*administration & dosage
Bupivacaine/*administration & dosage
Double-Blind Method
Drug Therapy, Combination
Fentanyl/*administration & dosage
Humans
Injections, Spinal
Male
Patient Satisfaction
Postoperative Period
Prospective Studies
Prostate/*surgery
Sufentanil/*administration & dosage
Time Factors
*Transurethral Resection of Prostate
Treatment Outcome
Analgesics, Opioid
Anesthetics, Local
Bupivacaine
Fentanyl
Sufentanil
Figure
Reference
-
1. Arrighi HM, Metter EJ, Guess HA, Fozzard JL. Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. Urology. 1991; 38:1 Suppl. 4–8.
Article2. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479.
Article3. Li MK, Garcia L, Patron N, Moh LC, Sundram M, Leungwattanakij S, et al. An Asian multinational prospective observational registry of patients with benign prostatic hyperplasia, with a focus on comorbidities, lower urinary tract symptoms and sexual function. BJU Int. 2008; 101:197–202.
Article4. Kim SY, Cho JE, Hong JY, Koo BN, Kim JM, Kil HK. Comparison of intrathecal fentanyl and sufentanil in low-dose dilute bupivacaine spinal anaesthesia for transurethral prostatectomy. Br J Anaesth. 2009; 103:750–754.
Article5. Hong JY, Yang SC, Ahn S, Kil HK. Preoperative comorbidities and relationship of comorbidities with postoperative complications in patients undergoing transurethral prostate resection. J Urol. 2011; 185:1374–1378.
Article6. Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008; 180:246–249.
Article7. Vaghadia H, Neilson G, Lennox PH. Selective spinal anesthesia for outpatient transurethral prostatectomy (TURP): randomized controlled comparison of chloroprocaine with lidocaine. Acta Anaesthesiol Scand. 2012; 56:217–223.
Article8. Malhotra V, Sudheendra V, O'Hara J, Diwan S. Anesthesia and the renal and genitourinary systems. In : Miller RD, editor. Miller's anesthesia. Philadelphia: Churchill Livingstone/Elsevier;2010. p. 2105–2134.9. Chung BI, Sommer G, Brooks JD. Anatomy of the lower urinary tract and male genitalia. In : Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh Urology. 10th ed. Philadelphia, PA: Saunders/Elsevier;2012. p. 33–70.10. Beers RA, Kane PB, Nsouli I, Krauss D. Does a mid-lumbar block level provide adequate anaesthesia for transurethral prostatectomy? Can J Anaesth. 1994; 41:807–812.
Article11. Racle JP, Benkhadra A, Poy JY, Gleizal B. Spinal analgesia with hyperbaric bupivacaine: influence of age. Br J Anaesth. 1988; 60:508–514.
Article12. Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 1992; 76:906–916.
Article13. Rocco AG, Raymond SA, Murray E, Dhingra U, Freiberger D. Differential spread of blockade of touch, cold, and pinprick during spinal anesthesia. Anesth Analg. 1985; 64:917–923.
Article14. Chamberlain DP, Chamberlain BD. Changes in the skin temperature of the trunk and their relationship to sympathetic blockade during spinal anesthesia. Anesthesiology. 1986; 65:139–143.
Article15. Vaghadia H. Spinal anaesthesia for outpatients: controversies and new techniques. Can J Anaesth. 1998; 45(5 Pt 2):R64–R75.
Article16. Fleisher LA, Mantha S, Roizen MF. Medical technology assessment: an overview. Anesth Analg. 1998; 87:1271–1282.17. Wassef MR, Michaels EI, Rangel JM, Tsyrlin AT. Spinal perianal block: a prospective, randomized, double-blind comparison with spinal saddle block. Anesth Analg. 2007; 104:1594–1596.
Article18. Carron M, Freo U, Veronese S, Innocente F, Ori C. Spinal block with 1.5 mg hyperbaric bupivacaine: not successful for everyone. Anesth Analg. 2007; 105:1515–1516.
Article19. Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Low-dose bupivacaine-fentanyl spinal anaesthesia for transurethral prostatectomy. Anaesthesia. 2003; 58:526–530.
Article20. Ben-David B, Solomon E, Levin H, Admoni H, Goldik Z. Intrathecal fentanyl with small-dose dilute bupivacaine: better anesthesia without prolonging recovery. Anesth Analg. 1997; 85:560–565.21. Hamber EA, Viscomi CM. Intrathecal lipophilic opioids as adjuncts to surgical spinal anesthesia. Reg Anesth Pain Med. 1999; 24:255–263.
Article22. de Santiago J, Santos-Yglesias J, Giron J, Montes de Oca F, Jimenez A, Diaz P. Low-dose 3 mg levobupivacaine plus 10 microg fentanyl selective spinal anesthesia for gynecological outpatient laparoscopy. Anesth Analg. 2009; 109:1456–1461.
Article23. Imarengiaye CO, Song D, Prabhu AJ, Chung F. Spinal anesthesia: functional balance is impaired after clinical recovery. Anesthesiology. 2003; 98:511–515.24. Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000; 91:1452–1456.
Article25. Zohar E, Noga Y, Rislick U, Leibovitch I, Fredman B. Intrathecal anesthesia for elderly patients undergoing short transurethral procedures: a dose-finding study. Anesth Analg. 2007; 104:552–554.
Article26. Richardson MG, Wissler RN. Densities of dextrose-free intrathecal local anesthetics, opioids, and combinations measured at 37 degrees C. Anesth Analg. 1997; 84:95–99.
Article27. Stienstra R, Gielen M, Kroon JW, Van Poorten F. The influence of temperature and speed of injection on the distribution of a solution containing bupivacaine and methylene blue in a spinal canal model. Reg Anesth. 1990; 15:6–11.28. Nelson KE, Rauch T, Terebuh V, D'Angelo R. A comparison of intrathecal fentanyl and sufentanil for labor analgesia. Anesthesiology. 2002; 96:1070–1073.
Article29. Standl TG, Horn E, Luckmann M, Burmeister M, Wilhelm S, Schulte am Esch J. Subarachnoid sufentanil for early postoperative pain management in orthopedic patients: a placebo-controlled, double-blind study using spinal microcatheters. Anesthesiology. 2001; 94:230–238.
Article30. Landau R, Kern C, Columb MO, Smiley RM, Blouin JL. Genetic variability of the mu-opioid receptor influences intrathecal fentanyl analgesia requirements in laboring women. Pain. 2008; 139:5–14.
Article31. Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004; 93:568–578.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Effect of Low Dose Bupivacaine Added with Fentanyl and Conventional Dose Bupivacaine in Spinal Anesthesia for a Transurethral Resection of the Prostate
- Combined Spinal-Epidural Anesthesia for Transurethral Resection of the Prostate
- Transient Neurological Syndrome after Bupivacaine Spinal Anesthesia: A case report
- Intrathecal meperidine reduces intraoperative shivering during transurethral prostatectomy in elderly patients
- Duration of Bupivacaine Mixed by Lidocaine in Hyperbaric Spinal Anesthesia