Clin Orthop Surg.
2015 Mar;7(1):54-61. 10.4055/cios.2015.7.1.54.
Advantage of Minimal Anterior Knee Pain and Long-term Survivorship of Cemented Single Radius Posterior-Stabilized Total Knee Arthroplasty without Patella Resurfacing
- Affiliations
-
- 1Department of Orthopedic Surgery, Ajou University Medical Center, Seoul, Korea.
- 2Department of Orthopaedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea. hayongch@naver.com
- KMID: 2069875
- DOI: http://doi.org/10.4055/cios.2015.7.1.54
Abstract
- BACKGROUND
The single radius total knee prosthesis was introduced with the advantage of reduced patellar symptoms; however, there is no long-term follow-up study of the same. The purpose of this study was to determine the survival rate of single radius posterior-stabilized total knee arthroplasty and patellofemoral complication rates in a consecutive series.
METHODS
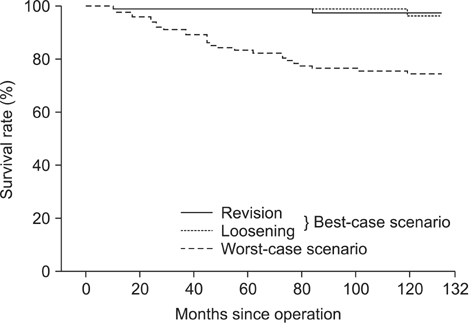
Seventy-one patients (103 knees) who underwent arthroplasty without patellar resurfacing using a single radius posterior-stabilized total knee prosthesis were followed up for a minimum 10 years. Clinical evaluation using Knee Society knee and function scores and radiologic evaluation were performed at regular intervals. Anterior knee pain as well as patellofemoral complications were evaluated with a simple questionnaire. The Kaplan-Meier product-limit method was used to estimate survival.
RESULTS
Seventeen patients (23 knees) were excluded due to death (12 knees) or lost to follow-up (11 knees). Of the 80 knees enrolled, all femoral components and 78 tibial components were well fixed without loosening at final follow-up. Two revisions were performed because of tibial component loosening and periprosthetic joint infection. One patient with tibial component loosening refused to have revision surgery. No obvious tibial insert polyethylene wear was observed. The survivorships at 132 months were 96.7% using revision or pending revision as end points. Anterior knee pain was present in 6 patients (6 knees, 7.5%) at the latest follow-up. No patellofemoral complication requiring revision was encountered.
CONCLUSIONS
The single radius posterior-stabilized total knee prosthesis demonstrated an excellent minimum 10-year survivorship. The low rates of implant loosening and 7.5% of anterior knee pain as a patellofemoral complication are comparable with those reported for other modern total knee prosthesis.
Keyword
MeSH Terms
Figure
Reference
-
1. Archibeck MJ, White RE Jr. What's new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2006; 88(7):1677–1686.
Article2. Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003; 85-A(2):259–265.
Article3. Callaghan JJ, Rosenberg AG, Rubash HE, Simonian PT, Wickiewicz TL, editors. The adult knee. Philadelphia: Lippincott Williams & Wilkins;2003.4. Abbas D, Gunn RS. Medium-term results of the Scorpio total knee replacement. Knee. 2006; 13(4):307–311.
Article5. Borrione F, Bonnevialle P, Mabit C, et al. Scorpio single radius total knee arthroplasty: a minimal five-year follow-up multicentric study. Int Orthop. 2011; 35(12):1777–1782.
Article6. D'Lima DD, Poole C, Chadha H, Hermida JC, Mahar A, Colwell CW Jr. Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clin Orthop Relat Res. 2001; (392):213–220.7. Gomez-Barrena E, Fernandez-Garcia C, Fernandez-Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Orthop Relat Res. 2010; 468(5):1214–1220.
Article8. Kolisek FR, Barnes CL. Scorpio posterior-stabilized knee system: 5-year clinical and functional results. J Arthroplasty. 2006; 21(8):1187–1192.
Article9. Mahoney OM, Kinsey TL. 5- to 9-year survivorship of single-radius, posterior-stabilized TKA. Clin Orthop Relat Res. 2008; 466(2):436–442.
Article10. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14.
Article11. Insall JN, Hood RW, Flawn LB, Sullivan DJ. The total condylar knee prosthesis in gonarthrosis: a five to nine-year follow-up of the first one hundred consecutive replacements. J Bone Joint Surg Am. 1983; 65(5):619–628.
Article12. Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP. A new patellofemoral scoring system for total knee arthroplasty. Clin Orthop Relat Res. 2006; 452:150–154.
Article13. Meftah M, Jhurani A, Bhat JA, Ranawat AS, Ranawat CS. The effect of patellar replacement technique on patellofemoral complications and anterior knee pain. J Arthroplasty. 2012; 27(6):1075–1080.e1.
Article14. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961; 43-B:752–757.
Article15. Grelsamer RP, Bazos AN, Proctor CS. Radiographic analysis of patellar tilt. J Bone Joint Surg Br. 1993; 75(5):822–824.
Article16. Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty: a prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994; 76(6):930–937.
Article17. Harwin SF. Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty. 1998; 13(7):753–762.
Article18. Yau WP, Wong JW, Chiu KY, Ng TP, Tang WM. Patellar clunk syndrome after posterior stabilized total knee arthroplasty. J Arthroplasty. 2003; 18(8):1023–1028.
Article19. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958; 53(282):457–481.
Article20. Ip D, Wu WC, Tsang WL. Comparison of two total knee prostheses on the incidence of patella clunk syndrome. Int Orthop. 2002; 26(1):48–51.
Article21. Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002; 84-A(2):187–193.22. Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003; 85-A(2):212–217.23. Burnett RS, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. Instr Course Lect. 2004; 53:167–186.
Article24. Campbell DG, Duncan WW, Ashworth M, et al. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006; 88(6):734–739.25. Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix total knee system. J Bone Joint Surg Br. 2008; 90(1):43–49.26. Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty: a concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009; 91(11):2562–2567.
Article27. Li S, Chen Y, Su W, Zhao J, He S, Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011; 35(3):305–316.
Article28. Garneti N, Mahadeva D, Khalil A, McLaren CA. Patellar resurfacing versus no resurfacing in Scorpio total knee arthroplasty. J Knee Surg. 2008; 21(2):97–100.
Article29. Liu ZT, Fu PL, Wu HS, Zhu Y. Patellar reshaping versus resurfacing in total knee arthroplasty: results of a randomized prospective trial at a minimum of 7 years' follow-up. Knee. 2012; 19(3):198–202.
Article30. Rasquinha VJ, Ranawat CS, Cervieri CL, Rodriguez JA. The press-fit condylar modular total knee system with a posterior cruciate-substituting design: a concise follow-up of a previous report. J Bone Joint Surg Am. 2006; 88(5):1006–1010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Knee Arthroplasty without Patellar Resurfacing in Moderate to Severe Patellofemoral Arthritis
- Total Knee Replacement Arthroplasty Without Patellar Resurfacing
- Patellar Nonresurfacing in Total Knee Arthroplasty
- Effectiveness of Patellar Replacementin Total Knee Arthroplasty : Randomized, Prospective Study using Simultaneous Bilateral Total Knee Arthroplasty
- Functional Results of the TKA with Non-resurfaced Patella according to Articular Degeneration of the Patella