J Korean Endocr Soc.
2007 Aug;22(4):282-286. 10.3803/jkes.2007.22.4.282.
A Case of Neutropenic Enterocolitis Complicating Methimazole-induced Agranulocytosis
- Affiliations
-
- 1Department of Internal Medicine, Eulji University School of Medicine.
- KMID: 2063539
- DOI: http://doi.org/10.3803/jkes.2007.22.4.282
Abstract
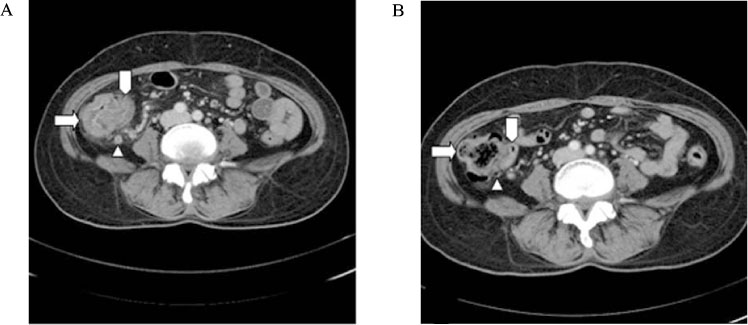
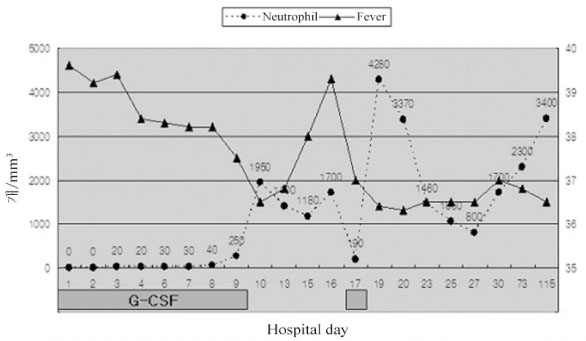
- Agranulocytosis is a rare complication of antithyroid drug therapy. Neutropenic enterocolitis is characterized by neutropenia plus cecal and ascending colon inflammation, and this is the most feared side effect of agranulocytosis. This is a rare complication of chemotherapy for treating hematological malignancies and less commonly, of the medication used for treating other diseases (e.g., hyperthyroidism). The mortality rate varies from 50 to 100%, with most deaths being due to bowel perforation and sepsis. Therefore, early recognition and proper medical management of neutropenic enterocolitis is important. Recently, early recognition and progress in the management have probably reduced the mortality of this malady, yet there have been no prospective randomized trials or high-quality retrospective studies on the treatment of neutropenic enterocolitis. Therefore, standardized recommendations concerning the indications for surgery cannot be made, but most of these patients are probably not candidates for surgical intervention. Non-surgical management may be a reasonable initial approach for those patients presenting without significant complications such as peritonitis, perforation or bleeding. We report here on a case that was treated with successful medical management for neutropenic enterocolitis that occurred when administering methimazole therapy as an antithyroid drug.
MeSH Terms
Figure
Reference
-
1. Cooper DS. The side effects of antithyroid drugs. Endocrinologist. 1999. 9:457–476.2. Tajiri J, Noguchi S. Antithyroid drug-induced agranulocytosis: special reference to normal white blood cell count agranulocytosis. Thyroid. 2004. 14:459–462.3. Pearce SH. Spontaneous reporting of adverse reactions to carbimazole and propylthiouracil in the UK. Clin Endocrinol (Oxf). 2004. 61:589–594.4. Toth EL, Mant MJ, Shivji S, Ginsberg J. Propylthiouracil-induced agranulocytosis: an unusual presentation and a possible mechanism. Am J Med. 1988. 85:725–727.5. Berkman EM, Orlin JB, Wolfsdorf J. An anti-neutrophil antibody associated with a propylthiouracil-induced lupus-like syndrome. Transfusion. 1983. 23:135–138.6. Akamizu T, Ozaki S, Hiratani H, Uesugi H, Sobajima J, Hataya Y, Kanamoto N, Saijo M, Hattori Y, Moriyama K, Ohmori K, Nakao K. Drug-induced neutropenia associated with anti-neutrophil cytoplasmic antibodies(ANCA): possible involvement of complement in granulocyte cytotoxicity. Clin Exp Immunol. 2002. 127:92–98.7. Cooper DS. Antithyroid drugs for the treatment of hyperthyroidism caused by Graves' disease. Endocrinol Metab Clin North Am. 1998. 27:225–247.8. Vanderpump MP, Ahlquist JA, Franklyn JA, Clayton RN. Consensus statement for good practice and audit measures in the management of hypothyroidism and hyperthyroidism: the Research Unit of the Royal College of Physicians of London, the Endocrinology and Diabetes Committee of the Royal College of Physicians of London, and the Society for Endocrinology. BMJ. 1996. 313:539–544.9. Nakamura S, Isaji M, Ishimori M. Morning granulocytopenia in a case of Graves' disease. Endocr J. 2001. 48:181–184.10. Sheng WH, Hung CC, Chen YC, Fang CT, Hsieh SM, Chang SC, Hsieh WC. Antithyroid-drug-induced agranulocytosis complicated by life-threatening infections. QJM. 1999. 92:455–461.11. Fukata S, Kuma K, Sugawara M. Granulocyte colony-stimulating factor (G-CSF) does not improve recovery from antithyroid drug-induced agranulocytosis: a prospective study. Thyroid. 1999. 9:29–31.12. Andres E, Kurtz JE, Perrin AE, Dufour P, Schlienger JL, Maloisel F. Haematopoietic growth factor in antithyroid-drug-induced agranulocytosis. QJM. 2001. 94:423–428.13. Tajiri J, Noguchi S, Okamura S, Morita M, Tamaru M, Murakami N, Niho Y. Granulocyte colony-stimulating factor treatment of antithyroid drug-induced granulocytopenia. . Arch Intern Med. 1993. 153:509–514.14. Ryan ME, Morrissey JF. Typhlitis complicating methimazole-induced agranulocytosis. Gastrointest Endosc. 1983. 29:299–302.15. Chen DF, Chao IM, Huang SH. Neutropenic colitis with cecal perforation during antithyroid therapy. J Formos Med Assoc. 2003. 102:644–646.16. Urbach DR, Rotstein OD. Typhlitis. Can J Surg. 1999. 42:415–419.17. Katz JA, Wagner ML, Gresik MV, Mahoney DH Jr, Fernbach DJ. Typhlitis. An 18-year experience and postmortem review. Cancer. 1990. 65:1041–1047.18. Gorschluter M, Mey U, Strehl J, Ziske C, Schepke M, Schmidt-Wolf IG, Sauerbruch T, Glasmacher A. Neutropenic enterocolitis in adults: systematic analysis of evidence quality. Eur J Haematol. 2005. 75:1–13.19. Wade DS, Nava HR, Douglass HO. Neutropenic enterocolitis. Clinical diagnosis and treatment. Cancer. 1992. 69:17–23.20. Cartoni C, Dragoni F, Micozzi A, Pescarmona E, Mecarocci S, Chirletti P, Petti MC, Meloni G, Mandelli F. Neutropenic enterocolitis in patients with acute leukemia: prognostic significance of bowel wall thickening detected by ultrasonography. J Clin Oncol. 2001. 19:756–761.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Methimazole-Induced Cholestatic Jaundice With Agranulocytosis
- A Case of Antithyroid Drug-Induced Agranulocytosis Treated with Granulocyte Colony-Stimulating Factor (G-CSF) and Methylprednisolone
- A Case of Methimazole-induced Agranulocytosis and Kikuchi's Disease in a Patient with Graves' Disease
- A case of propylthiouracil-induced hepatitis with agranulocytosis
- A Case of Acute Appendicitis in a Patient with Methimazole-Induced Agranulocytosis