Imaging Sci Dent.
2015 Jun;45(2):123-131. 10.5624/isd.2015.45.2.123.
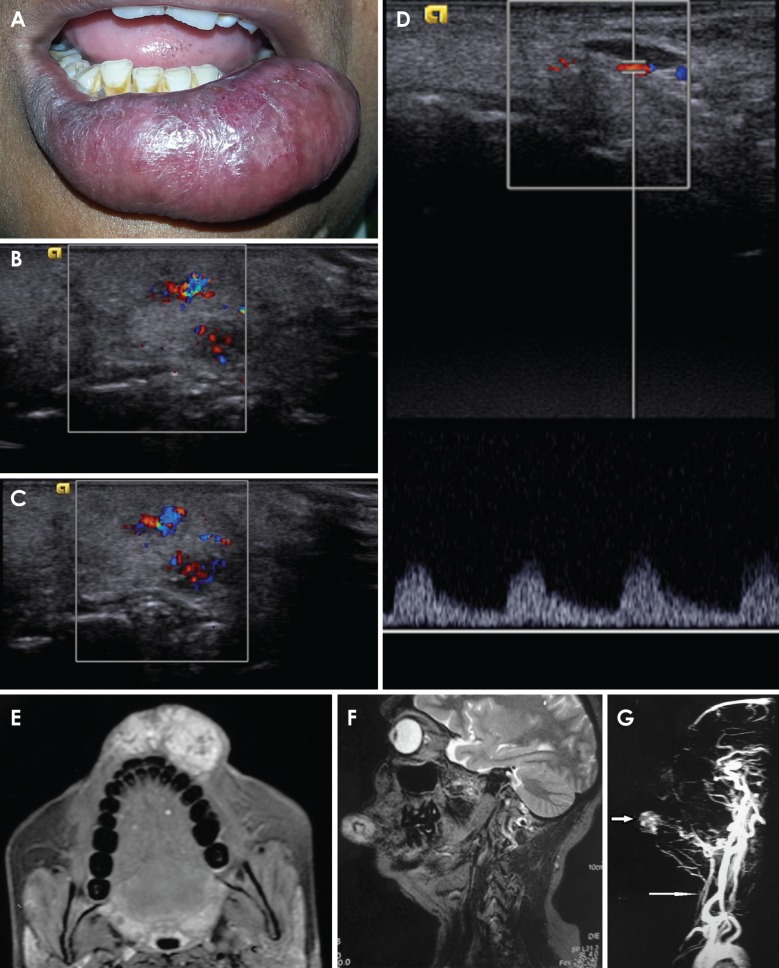
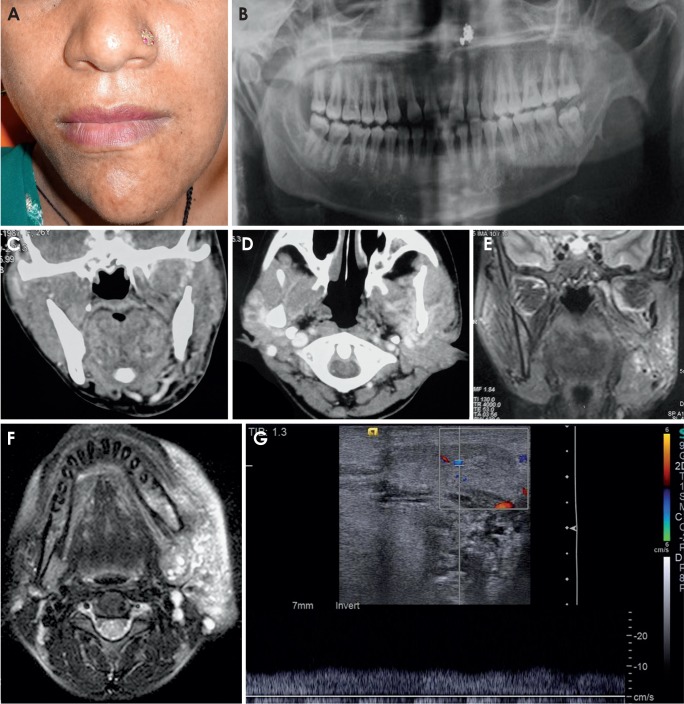
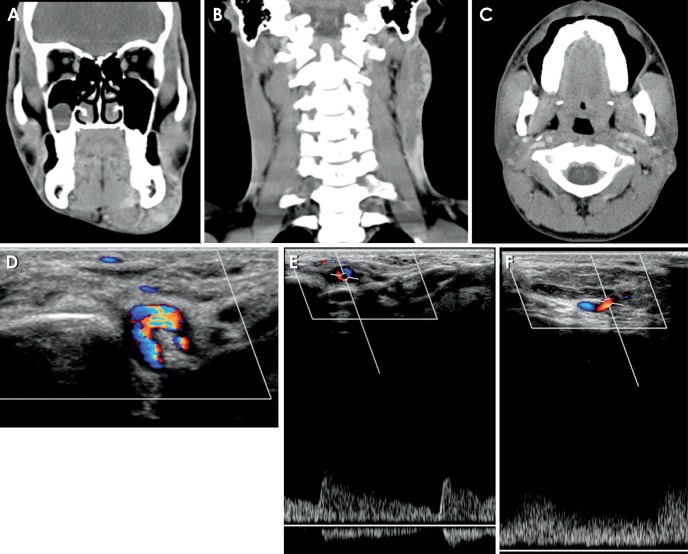
The current approach to the diagnosis of vascular anomalies of the head and neck: A pictorial essay
- Affiliations
-
- 1Department of Oral Medicine and Radiology, Maulana Azad Institute of Dental Sciences, Delhi, India. sgoeldoc@gmail.com
- 2Department of Radiodiagnosis, Lok Nayak Jaiprakash Hospital, Delhi, India.
- 3Department of Radiodiagnosis, Govind Ballabh Pant Hospital, Delhi, India.
- KMID: 2054215
- DOI: http://doi.org/10.5624/isd.2015.45.2.123
Abstract
- Throughout the years, various classifications have evolved for the diagnosis of vascular anomalies. However, it remains difficult to classify a number of such lesions. Because all hemangiomas were previously considered to involute, if a lesion with imaging and clinical characteristics of hemangioma does not involute, then there is no subclass in which to classify such a lesion, as reported in one of our cases. The recent classification proposed by the International Society for the Study of Vascular Anomalies (ISSVA, 2014) has solved this problem by including non-involuting and partially involuting hemangioma in the classification. We present here five cases of vascular anomalies and discuss their diagnosis in accordance with the ISSVA (2014) classification. A non-involuting lesion should not always be diagnosed as a vascular malformation. A non-involuting lesion can be either a hemangioma or a vascular malformation depending upon its clinicopathologic and imaging characteristics.
Keyword
Figure
Reference
-
1. Mulliken JB, Young AE. Vascular birthmarks: hemangiomas and malformations. Philadelphia: Saunders;1988.2. Persky MS, Yoo HJ, Berenstein A. Management of vascular malformations of the mandible and maxilla. Laryngoscope. 2003; 113:1885–1892. PMID: 14603041.
Article3. Mulliken JB, Glowacki J. Haemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982; 69:412–422. PMID: 7063565.4. International Society for the Study of Vascular Anomalies [Internet]. Little Rock (AR): ISSVA classification for vascular anomalies;assessed 2014 Apr; cited 2014 Oct 28. Available from: http://www.issva.org/content.aspx?page_id=22&club_id=298433&module_id=152904.5. Lam SM, Williams EF. Vascular anomalies: review and current therapy. Curr Opin Otolaryngol Head Neck Surg. 2002; 10:309–315.
Article6. Thakral A, Sharma SM. Cervicofacial hemangiomas: pattern, clinical management, and treatment outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:e457–e464. PMID: 22901655.
Article7. Li FP, Cassady JR, Barnett E. Cancer mortality following irradiation in infancy for hemangioma. Radiology. 1974; 113:177–178. PMID: 4479424.
Article8. Kohout MP, Hansen M, Pribaz JJ, Mulliken JB. Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg. 1998; 102:643–654. PMID: 9727427.
Article9. Takahashi K, Mulliken JB, Kozakewich HP, Rogers RA, Folkman J, Ezekowitz RA. Cellular markers that distinguish the phases of hemangioma during infancy and childhood. J Clin Invest. 1994; 93:2357–2364. PMID: 7911127.
Article10. Enjolras O, Riche MC, Merland JJ, Escande JP. Management of alarming hemangiomas in infancy: a review of 25 cases. Pediatrics. 1990; 85:491–498. PMID: 2097998.
Article11. Nasseri E, Piram M, McCuaig CC, Kokta V, Dubois J, Powell J. Partially involuting congenital hemangiomas: a report of 8 cases and review of the literature. J Am Acad Dermatol. 2014; 70:75–79. PMID: 24176519.
Article12. Chang E, Boyd A, Nelson CC, Crowley D, Law T, Keough KM, et al. Successful treatment of infantile hemangiomas with interferon-alpha-2b. J Pediatr Hematol Oncol. 1997; 19:237–244. PMID: 9201147.13. Donnelly LF, Adams DM, Bisset GS 3rd. Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol. 2000; 174:597–608. PMID: 10701595.14. Meyer JS, Hoffer FA, Barnes PD. Biological classification of soft-tissue vascular anomalies: MR correlation. AJR Am J Roentgenol. 1991; 157:559–564. PMID: 1872245.
Article15. Yakes WF, Rossi P, Odink H. How I do it. Arteriovenous malformation management. Cardiovasc Intervent Radiol. 1996; 19:65–71. PMID: 8729181.16. Yakes WF, Haas DK, Parker SH, Gibson MD, Hopper KD, Mulligan JS, et al. Symptomatic vascular malformations: ethanol embolotherapy. Radiology. 1989; 170:1059–1066. PMID: 2916057.
Article17. Gomes AS. Embolization therapy of congenital arteriovenous malformations: use of alternate approaches. Radiology. 1994; 190:191–198. PMID: 8259403.
Article18. Riche MC, Hadjean E, Tran-Ba-Huy P, Merland JJ. The treatment of capillary-venous malformations using a new fibrosing agent. Plast Reconstr Surg. 1983; 71:607–614. PMID: 6836059.
Article19. Dubois JM, Sebag GH, De Prost Y, Teillac D, Chretien B, Brunelle FO. Soft-tissue venous malformations in children: percutaneous sclerotherapy with Ethibloc. Radiology. 1991; 180:195–198. PMID: 2052693.
Article20. Ahuja AT, Richards P, Wong KT, Yuen EH, King AD. Accuracy of high-resolution sonography compared with magnetic resonance imaging in the diagnosis of head and neck venous vascular malformations. Clin Radiol. 2003; 58:869–875. PMID: 14581011.
Article21. Burrows PE, Laor T, Paltiel H, Robertson RL. Diagnostic imaging in the evaluation of vascular birthmarks. Dermatol Clin. 1998; 16:455–488. PMID: 9704205.
Article22. Baker LL, Dillon WP, Hieshima GB, Dowd CF, Frieden IJ. Hemangiomas and vascular malformations of the head and neck: MR characterization. AJNR Am J Neuroradiol. 1993; 14:307–314. PMID: 8456703.23. Gelbert F, Riche MC, Reizine D, Guichard JP, Assouline E, Hodes JE, et al. MR imaging of head and neck vascular malformations. J Magn Reson Imaging. 1991; 1:579–584. PMID: 1790383.
Article24. Chooi WK, Woodhouse N, Coley SC, Griffiths PD. Pediatric head and neck lesions: assessment of vascularity by MR digital subtraction angiography. AJNR Am J Neuroradiol. 2004; 25:1251–1255. PMID: 15313719.25. Burrows PF, Robertson RL, Barnes PD. Angiography and the evaluation of cerebrovascular disease in childhood. Neuroimaging Clin N Am. 1996; 6:561–588. PMID: 8873093.26. Loureiro CC, Falchet PC, Gavranich J, Lobo Leandro LF. Embolization as the treatment for a life-threatening mandibular arteriovenous malformation. J Craniofac Surg. 2010; 21:380–382. PMID: 20186078.
Article27. Kakimoto N, Tanimoto K, Nishiyama H, Murakami S, Furukawa S, Kreiborg S. CT and MR imaging features of oral and maxillofacial hemangioma and vascular malformation. Eur J Radiol. 2005; 55:108–112. PMID: 15950107.
Article28. Kondylidou-Sidira A, Dietrich EM, Koloutsos G, Sakkas L, Antoniades K. Intraosseous vascular malformation of the mandibular condyle: presentation of a case and differential diagnosis. Oral Radiol. 2012; 28:150–156.
Article29. Mossa-Basha M, Chen J, Gandhi D. Imaging of cerebral arteriovenous malformations and dural arteriovenous fistulas. Neurosurg Clin N Am. 2012; 23:27–42. PMID: 22107856.
Article30. Burrows PE, Mulliken JB, Fellows KE, Strand RD. Childhood hemangiomas and vascular malformations: angiographic differentiation. AJR Am J Roentgenol. 1983; 141:483–488. PMID: 6603756.
Article31. Gold L, Nazarian LN, Johar AS, Rao VM. Characterization of maxillofacial soft tissue vascular anomalies by ultrasound and color Doppler imaging: an adjuvant to computed tomography and magnetic resonance imaging. J Oral Maxillofac Surg. 2003; 61:19–31. PMID: 12524603.
Article32. Pribaz JJ, Morris DJ, Mulliken JB. Three-dimensional folded free-flap reconstruction of complex facial defects using intraoperative modeling. Plast Reconstr Surg. 1994; 93:285–293. PMID: 8310020.
Article33. Kademani D, Costello BJ, Ditty D, Quinn P. An alternative approach to maxillofacial arteriovenous malformations with transosseous direct puncture embolization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:701–706. PMID: 15184851.
Article34. Altuğ HA, Büyüksoy V, Okçu KM, Doğan N. Hemangiomas of the head and neck with phleboliths: clinical features, diagnostic imaging, and treatment of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:e60–e64. PMID: 17188913.
Article35. Konas E, Canter HI, Cil B, Peynircioglu B, Karabulut E, Tuncbilek G, et al. Volumetric assessment of results of treatment of vascular malformations of the head and neck regions treated with a minimally invasive surgical technique after embolization procedure. J Craniofac Surg. 2009; 20:402–405. PMID: 19258907.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vascular anomalies of the head and neck: current overview
- Pictorial Essay: Understanding of Persistent Left Superior Vena Cava and Its Differential Diagnosis
- Congenital Anomalies of the Coronary Sinus: A Pictorial Essay
- Basic principles and applications of 18F-FDG-PET/CT in oral and maxillofacial imaging: A pictorial essay
- The Utility of 64 Channel Multidetector CT Angiography for Evaluating the Renal Vascular Anatomy and Possible Variations: a Pictorial Essay