Electrolyte Blood Press.
2007 Dec;5(2):62-67. 10.5049/EBP.2007.5.2.62.
Effects of Increased Uric Acid Intake on the Abundance of Urate-anion exchanger and Organic Anion Transporter Proteins in the Rat Kidney
- Affiliations
-
- 1Institute of Biomedical Sciences, Hanyang University, Hanyang University, Seoul, Korea. kimgh@hanyang.ac.kr
- 2Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2052287
- DOI: http://doi.org/10.5049/EBP.2007.5.2.62
Abstract
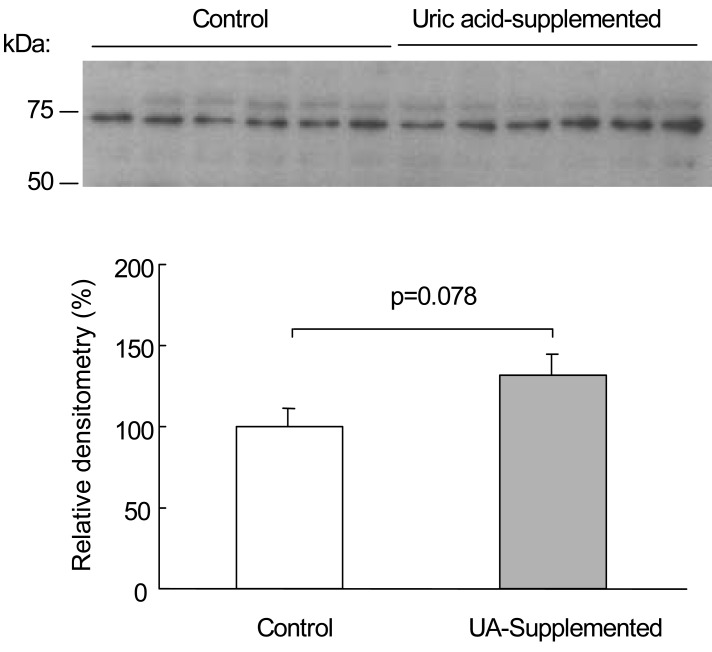
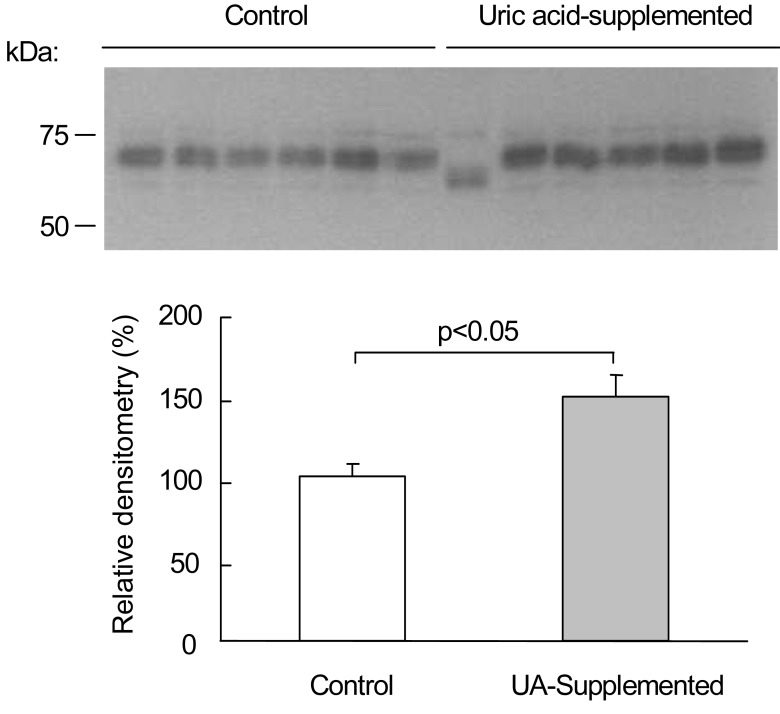
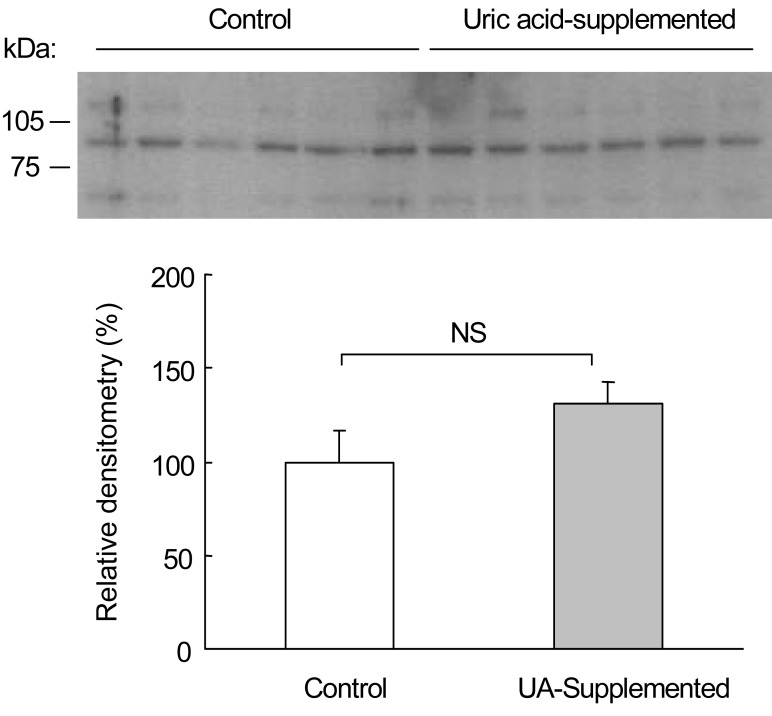
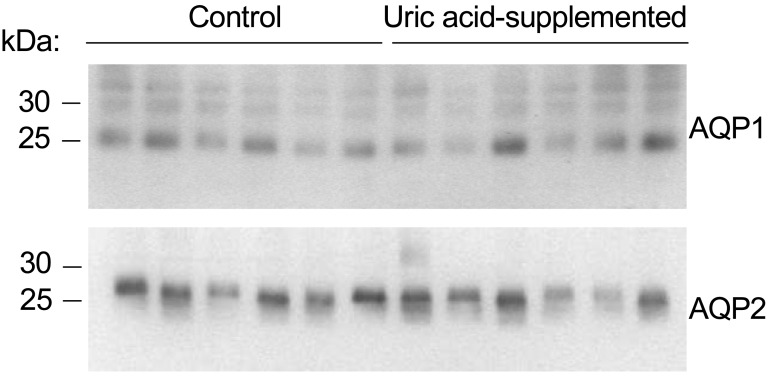
- Renal handling of uric acid mainly occurs in the proximal tubule, and bidirectional transport of urate may involve apical absorption via the urate-anion exchanger (URAT1) and basolateral uptake via organic anion transporters (OAT1 and OAT3). In rat kidneys, we investigated whether the protein abundance of URAT1, OAT1, and OAT3 is affected by the increase in uric acid intake. Male Sprague-Dawley rats were randomly divided into control and uric acid-supplemented groups, and uric acid-supplemented rats were given 0.75 g of uric acid per 180 g body weight per day for 8 days. After the animal experiment, kidneys were harvested and semi-quantitative immunoblotting was carried out from cortical homogenates using polyclonal peptide-derived antibodies to URAT1, OAT1, and OAT3. Serum uric acid level showed an increasing tendency (p=0.055) in the uric acid-supplemented rats (2.60+/- 0.27 mg/dL) compared with control rats (1.97+/-0.29 mg/dL), whereas urinary uric acid excretion was not significantly different between the uric acid-supplemented rats (3.27+/-0.40 mg/d) and control rats (2.61+/-0.34 mg/d). URAT1 protein abundance in cortical homogenates was not significantly different between the uric acid-supplemented rats (132+/-14%) and control rats (100+/-7%). However, OAT1 protein abundance was significantly (p<0.05) increased in the uric acid-supplemented rats (148+/-13%) compared with the control rats (100+/-8%). OAT3 protein abundance was not significantly different between the uric acid-supplemented rats (131+/-12%) and control rats (100+/-17%). In conclusion, OAT1 may have a regulatory role in response to the increase in uric acid intake in the rat kidney. The up-regulation of OAT1 would exert stimulation of urinary uric acid excretion and might contribute to protection from hyperuricemia.
MeSH Terms
Figure
Reference
-
1. Sica DA, Schoolwerth AC. Brenner BM, editor. Renal handling of organic anions and cation: excretion of uric acid. The Kidney. 2000. 6th ed. Philadelphia: WB Saunders;p. 680–700.2. Anzai N, Kanai Y, Endou H. New insights into renal transport of urate. Curr Opin Rheumatol. 2007; 19:151–157. PMID: 17278930.
Article3. Tojo A, Sekine T, Nakajima N, Hosoyamada M, Kanai Y, Kimura K, Endou H. Immunohistochemical localization of multispecific renal organic anion transporter 1 in rat kidney. J Am Soc Nephrol. 1999; 10:464–471. PMID: 10073596.
Article4. Lee S, Kang KP, Kang SK. Renal Transport of Urate. Electrolyte Blood Press. 2005; 3:79–81.
Article5. Ljubojevic M, Herak-Kramberger CM, Hagos Y, Bahn A, Endou H, Burckhardt G, Sabolic I. Rat renal cortical OAT1 and OAT3 exhibit gender differences determined by both androgen stimulation and estrogen inhibition. Am J Physiol Renal Physiol. 2004; 287:F124–F138. PMID: 15010355.6. Bakhiya A, Bahn A, Burckhardt G, Wolff N. Human organic anion transporter 3 (hOAT3) can operate as an exchanger and mediate secretory urate flux. Cell Physiol Biochem. 2003; 13:249–256. PMID: 14586168.
Article7. Enomoto A, Kimura H, Chairoungdua A, Shigeta Y, Jutabha P, Cha SH, Hosoyamada M, Takeda M, Sekine T, Igarashi T, Matsuo H, Kikuchi Y, Oda T, Ichida K, Hosoya T, Shimokata K, Niwa T, Kanai Y, Endou H. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature. 2002; 417:447–452. PMID: 12024214.8. Maesaka JK, Fishbane S. Regulation of renal urate excretion: a critical review. Am J Kidney Dis. 1998; 32:917–933. PMID: 9856507.
Article9. Choi HK, Mount DB, Reginato AM. American College of Physicians. American Physiological Society. Pathogenesis of gout. Ann Intern Med. 2005; 143:499–516. PMID: 16204163.
Article10. Kojima R, Sekine T, Kawachi M, Cha SH, Suzuki Y, Endou H. Immunolocalization of multispecific organic anion transporters, OAT1, OAT2, and OAT3, in rat kidney. J Am Soc Nephrol. 2002; 13:848–857. PMID: 11912243.
Article11. Hosoyamada M, Ichida K, Enomoto A, Hosoya T, Endou H. Function and localization of urate transporter 1 in mouse kidney. J Am Soc Nephrol. 2004; 15:261–268. PMID: 14747372.12. Ames BN, Cathcart R, Schwiers E, Hochstein P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc Natl Acad Sci U S A. 1981; 78:6858–6862. PMID: 6947260.
Article13. Becker BF. Towards the physiological function of uric acid. Free Radic Biol Med. 1993; 14:615–631. PMID: 8325534.
Article14. Johnson RJ, Rideout BA. Uric acid and diet-insights into the epidemic of cardiovascular disease. N Engl J Med. 2004; 350:1071–1073. PMID: 15014177.15. Wu XW, Muzny DM, Lee CC, Caskey CT. Two independent mutational events in the loss of urate oxidase during hominoid evolution. J Mol Evol. 1992; 34:78–84. PMID: 1556746.
Article16. Oparil S, Zaman MA, Calhoun DA. Pathogenesis of hypertension. Ann Intern Med. 2003; 139:761–776. PMID: 14597461.
Article17. Enomoto A, Endou H. Roles of organic anion transporters (OATs) and a urate transporter (URAT1) in the pathophysiology of human disease. Clin Exp Nephrol. 2005; 9:195–205. PMID: 16189627.
Article18. Abramson RG, Levitt MF. Micropuncture study of uric acid transport in rat kidney. Am J Physiol. 1975; 228:1597–1605. PMID: 1130564.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Losartan Administration on Uric acid Transporters in Rat Kidney
- Renal Transport of Urate
- Molecular aspects of organic ion transporters in the kidney
- A Case of Idiopathic Renal Hypouricemia with SLC22A12 Gene Mutation Showing General Weakness and Incidental Renal Stone
- Introduction of Organic Anion Transporters (SLC22A) and a Regulatory Mechanism by Caveolins