Korean Circ J.
2011 Apr;41(4):203-208. 10.4070/kcj.2011.41.4.203.
Change in Blood Pressure and Pulse Pressure in Preterm Infants After Treatment of Patent Ductus Arteriosus With Indomethacin
- Affiliations
-
- 1Department of Pediatrics, Chonnam National University Medical School, Gwangju, Korea. cardiol@jnu.ac.kr
- KMID: 2028945
- DOI: http://doi.org/10.4070/kcj.2011.41.4.203
Abstract
- BACKGROUND AND OBJECTIVES
Patent ductus arteriosus (PDA) is associated with increased morbidity and mortality in premature infants. Therefore, an early diagnosis and treatment of a hemodynamically significant PDA are very important. A widened pulse pressure is considered to be a well known clinical sign of a PDA in older infants and children; however, whether this is also applicable in the case of preterm infants remains to be confirmed. The aims of this study were to investigate the change in blood pressure (BP) before and after medical treatment of a PDA with indomethacin and to evaluate if the change in the pulse pressure in preterm infants with a medically treated PDA could be used as a reliable clinical predictor of a hemodynamically significant PDA.
SUBJECTS AND METHODS
Between January 2005 and June 2009, a retrospective analysis was performed in preterm infants with a hemodynamically significant PDA (PDA group, n=72) and preterm infants without a PDA (control group, n=72) at the Chonnam National University Hospital Neonatal Intensive Care Unit. The PDA was closed by treatment with indomethacin. The BP was compared between the two groups over the seven days after the first dose of indomethacin.
RESULTS
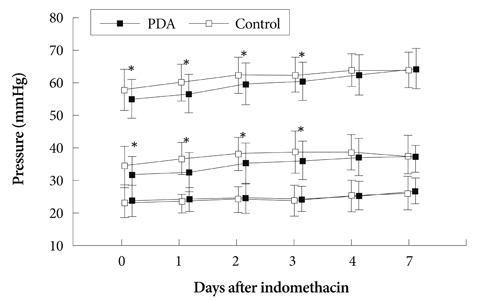
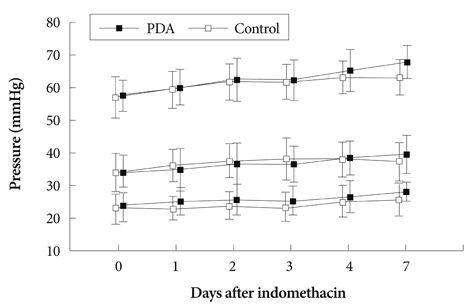
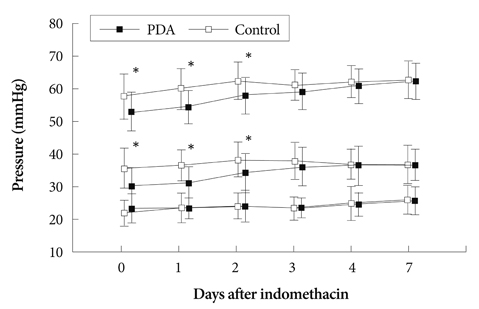
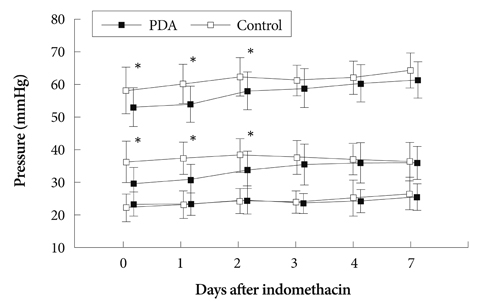
In preterm infants with a hemodynamically significant PDA, the mean systolic (55.1+/-6.0 mmHg) and diastolic BPs (31.4+/-6.2 mmHg) were lower than those in the controls (mean systolic BP 58.0+/-6.4 mmHg, mean diastolic BP 34.7+/-6.0 mmHg) before indomethacin treatment. When the ductus arteriosus was successfully closed by indomethacin treatment, there was a gradual increase in both the systolic and diastolic BPs without any change in the pulse pressure.
CONCLUSION
The results of this study show that a widened pulse pressure is not a useful clinical sign of a hemodynamically significant PDA in preterm infants. However, low systolic and diastolic BPs may be useful clinical signs of a hemodynamically significant PDA in preterm infants. If the systolic and diastolic BP is low, a PDA should be considered and echocardiography should be performed for early diagnosis and treatment.
MeSH Terms
Figure
Reference
-
1. Wyllie J. Treatment of patent ductus arteriosus. Semin Neonatol. 2003. 8:425–432.2. Knight DB. The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Semin Neonatol. 2001. 6:63–73.3. Rakza T, Magnenant E, Klosowski S, Tourneux P, Bachiri A, Storme L. Early hemodynamic consequences of patent ductus arteriosus in preterm infants with intra-uterine growth restriction. J Pediatr. 2007. 151:624–628.4. Evans N, Moor Craft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992. 67:1169–1173.5. Kluckow M, Evans N. Ductal shunting, high pulmonary blood flow, and pulmonary hemorrhage. J Pediatr. 2000. 137:68–72.6. Kim HS, Lee K. A study on patent ductus arteriosus in premature infants. Korean Circ J. 1985. 15:483–496.7. Shimada S, Kasai T, Konishi M, Fujiwara T. Effects of patent ductus arteriosus on left ventricular output and organ blood flows in preterm infants with respiratory distress syndrome treated with surfactant. J Pediatr. 1994. 125:270–277.8. Bernstein D. Behrman RE, Kliegman RM, Jenson HB, editors. A cyanotic congenital heart diseases: the left-to right shunt lesions. Nelson Textbook of Pediatrics. 2007. 18th ed. Philadelphia: W.B. Saunders Company;1891–1893.9. Lubetzky R, Mendel D, Mimouni FB, et al. Indomethacin induced early patent ductus arteriosus closure cannot be predicted by a decrease in pulse pressure. Am J Perinatol. 2004. 21:257–261.10. Hoffman TM, Welty SE. Emmanouilides GC, Riemenschneider TA, editors. Patent ductus arteriosus. Moss and Adams' Heart Disease in Infants, Children, and Adolescents. 2008. 7th ed. Philadelphia: Williams & Wilkins;440–441.11. Evans N, Iyer P. Change in blood pressure after treatment of patent ductus arteriosus with indomethacin. Arch Dis Child. 1993. 68:584–587.12. Perlman JM, Hill A, Volpe JJ. The effect of patent ductus arteriosus on flow velocity in the anterior cerebral arteries: ductal steal in the premature newborn infant. J Pediatr. 1981. 99:767–771.13. Rudolph AM, Scarpelli EM, Golinto RJ, Gootman NL. Hemodynamic basis for clinical manifestations of patent ductus arteriosus. Am Heart J. 1964. 68:447–458.14. Ratner I, Perelmuter B, Toews W, Whitfield J. Association of low systolic and diastolic blood pressure with significant patent ductus arteriosus in very low birth weight infants. Crit Care Med. 1985. 13:497–500.15. Choi SK. Problems in measuring blood pressure. Korean Circ J. 1997. 27:485–487.16. Lee J, Rajadurai VS, Tan KW. Blood pressure standards for low birth weight infants during the first day of life. Arch Dis Child Fetal Neonatal Ed. 1999. 81:F168–F170.17. Skinner J. Diagnosis of patent ductus arteriosus. Semin Neonatol. 2001. 6:49–61.18. Hirsimaki H, Kero P, Wanne O. Doppler ultrasound and clinical evaluation in detection and grading of patent ductus arteriosus in neonates. Crit Care Med. 1990. 18:490–493.19. Valdes-Cruz LM, Dudell GG. Specificity and accuracy of echocardiographic diagnosis and clinical criteria for diagnosis of patent ductus arteriosus in fluid-restricted infants. J Pediatr. 1981. 98:298–305.20. Davis P, Turner-Gomes S, Cunningham K, Way C, Roberts R, Schmidt B. Precision and accuracy of clinical and radiological signs in premature infants at risk of patent ductus arteriosus. Arch Pediatr Adolesc Med. 1995. 149:1136–1141.21. Hegyi T, Anwar M, Carbone MT, et al. Blood pressure ranges in premature infants: part II. the first week of life. Pediatrics. 1996. 97:336–342.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indomethacin therapy in premature infants with patent ductus arteriosus
- The effects of ibuprofen and indomethacin therapy for patent ductus arteriosus in preterm infants
- Recent Advance in Management of Patent Ductus Arteriosus in Extremely Low Birth Weight Infants
- Spontaneous Closing Time of PDA in Term and Preterm Infants Without Respiratory Distress Syndrome
- Oral Ibuprofen versus Intravenous Indomethacin for the Treatment of Patent Ductus Arteriosus in Very Low Birth Weight Infants