Hanyang Med Rev.
2009 Nov;29(4):315-326. 10.7599/hmr.2009.29.4.315.
Recent Advance in Management of Patent Ductus Arteriosus in Extremely Low Birth Weight Infants
- Affiliations
-
- 1Department of Pediatrics, College of Medicine Korea University, Seoul, Korea. cbmin@korea.ac.kr
- KMID: 2053718
- DOI: http://doi.org/10.7599/hmr.2009.29.4.315
Abstract
- Management of patent ductus arteriosus (PDA) in preterm infants has always been a challenge to the neonatologist and continues to be a controversial topic. There is no evidence that medical treatment with cyclooxygenase inhibitors for the prevention and treatment of PDA decreases mortality or serious morbidity, despite success in closure of the PDA. In practice, however, treatment decisions should be made for individual preterm infants in the absence of knowledge about benefits and risks of medical treatment should be made on the individual basis. This article attempts to review the current available, often conflicting data and to present the clinical guidelines for management of PDA in preterm infants, especially for extremely low birth weight (ELBW) infants. Prophylactic or early pre-symptomatic treatment may unnecessarily expose these infants, in whom the ductus might close spontaneously, to pharmacologic agents and their adverse effects. On the other hand, with advancing postnatal age, delayed treatment could potentially decrease successful medical closure thereby increasing the rate of surgical ligation and the complications associated with surgery. Therefore early symptomatic treatment in ELBW infants is preferred as the primary pharmacologic treatment for PDA. Conservative treatment with adjustment of ventilation and fluid restriction is beneficial as an alternative management to prophylactic pharmacologic treatment.
MeSH Terms
Figure
Reference
-
1. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.
Article2. Bhandari A, Bhandari V. Pitfalls, problems, and progress in bronchopulmonary dysplasia. Pediatrics. 2009; 123:1562–1573.
Article3. Attar MA, Donn SM. Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol. 2002; 7:353–360.
Article4. Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med. 1998; 157:294–323.5. Donn SM, Sinha SK. Minimising ventilator induced lung injury in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2006; 91:F226–F230.
Article6. De Paoli AG, Morley C, Davis PG. Nasal CPAP for neonates: what do we know in 2003? Arch Dis Child Fetal Neonatal Ed. 2003; 88:F168–F172.
Article7. Sharma A, Greenough A. Survey of neonatal respiratory support strategies. Acta Paediatr. 2007; 96:1115–1117.
Article8. Bancalari E, Claure N. Non-invasive ventilation of the preterm infant. Early Hum Dev. 2008; 84:815–819.
Article9. Owen LS, Morley CJ, Davis PG. Neonatal nasal intermittent positive pressure ventilation: what do we know in 2007? Arch Dis Child Fetal Neonatal Ed. 2007; 92:F414–F418.
Article10. Polin RA, Sahni R. Newer experience with CPAP. Semin Neonatol. 2002; 7:379–389.
Article11. Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. COIN Trial Investigators. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008; 358:700–708.
Article12. Davis PG, Morley CJ, Owen LS. Non-invasive respiratory support of preterm neonates with respiratory distress: continuous positive airway pressure and nasal intermittent positive pressure ventilation. Semin Fetal Neonatal Med. 2009; 14:14–20.
Article13. Friedlich P, Lecart C, Posen R, Ramicone E, Chan L, Ramanathan R. A randomized trial of nasopharyngeal-synchronized intermittent mandatory ventilation versus nasopharyngeal continuous positive airway pressure in very low birth weight infants after extubation. J Perinatol. 1999; 19:413–418.
Article14. Hutchison AA, Bignall S. Non-invasive positive pressure ventilation in the preterm neonate: reducing endotrauma and the incidence of bronchopulmonary dysplasia. Arch Dis Child Fetal Neonatal Ed. 2008; 93:F64–F68.
Article15. Barrington KJ, Bull D, Finer NN. Randomized trial of nasal synchronized intermittent mandatory ventilation compared with continuous positive airway pressure after extubation of very low birth weight infants. Pediatrics. 2001; 107:638–641.
Article16. Kugelman A, Feferkorn I, Riskin A, Chistyakov I, Kaufman B, Bader D. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure for respiratory distress syndrome: a randomized, controlled, prospective study. J Pediatr. 2007; 150:521–526.
Article17. Donn SM. Neonatal ventilators: how do they differ? J Perinatol. 2009; 29:Suppl 2. S73–S78.
Article18. Gupta S, Sinha SK. Newer modalities of mechanical ventilation in the extremely premature infants. Paediatr Child Health. 2007; 17:37–42.
Article19. Hummler H, Schulze A. New and alternative modes of mechanical ventilation in neonates. Semin Fetal Neonatal Med. 2009; 14:42–48.
Article20. Sinha SK, Donn SM. Volume-controlled ventilation: variations on a theme. Clin Perinatol. 2001; 28:547–560.21. Singh J, Sinha SK, Donn SM. Volume-targeted ventilation of newborns. Clin Perinatol. 2007; 34:93–105.
Article22. Patel DS, Sharma A, Prendergast M, Rafferty GF, Greenough A. Work of breathing and different levels of volume-targeted ventilation. Pediatrics. 2009; 123:e679–e684.
Article23. McCallion N, Lau R, Dargaville PA, Morley CJ. Volume guarantee ventilation, interrupted expiration, and expiratory braking. Arch Dis Child. 2005; 90:865–870.
Article24. Cheema IU, Ahluwalia JS. Feasibility of tidal volume-guided ventilation in newborn infants: a randomized crossover trial using the volume guarantee modality. Pediatrics. 2001; 107:1323–1328.
Article25. Herrera CM, Gerhardt T, Claure N, et al. Effects of volume-guaranteed synchronized intermittent mandatory ventilation in preterm infants recovering from respiratory failure. Pediatrics. 2002; 110:529–533.
Article26. Abubakar KM, Keszler M. Patient-ventilator interactions in new modes of patient-triggered ventilation. Pediatr Pulmonol. 2001; 32:71–75.
Article27. Sinha SK, Donn SM. Newer forms of conventional ventilation for preterm newborns. Acta Paediatr. 2008; 97:1338–1343.
Article28. Abubakar KM, Keszler M. Patient-ventilator interactions in new modes of patient-triggered ventilation. Pediatr Pulmonol. 2001; 32:71–75.
Article29. Sarkar S, Donn SM. In support of pressure support. Clin Perinatol. 2007; 34:117–128.
Article30. Donn SM, Becker MA. Baby in control: neonatal pressure support ventilation. Neonatal Intensive Care. 1998; 11:16–20.31. Osorio W, Claure N, D'Ugard C, Athavale K, Bancalari E. Effects of pressure support during an acute reduction of synchronized intermittent mandatory ventilation in preterm infants. J Perinatol. 2005; 25:412–416.
Article32. Schulze A, Bancalari E. Proportional assist ventilation in infants. Clin Perinatol. 2001; 28:561–578.
Article33. Schulze A, Gerhardt T, Musante G, Schaller P, Claure N, Everett R, Gomez-Marin O, Bancalari E. Proportional assist ventilation in low birth weight infants with acute respiratory disease. A comparison to assist/control and conventional mechanical ventilation. J Pediatr. 1999; 135:339–344.
Article34. Schulze A, Rieger-Fackeldey E, Gerhardt T, Claure N, Everett R, Bancalari E. Randomized crossover comparison of proportional assist ventilation and patient-triggered ventilation in extremely low birth weight infants with evolving chronic lung disease. Neonatology. 2007; 92:1–7.
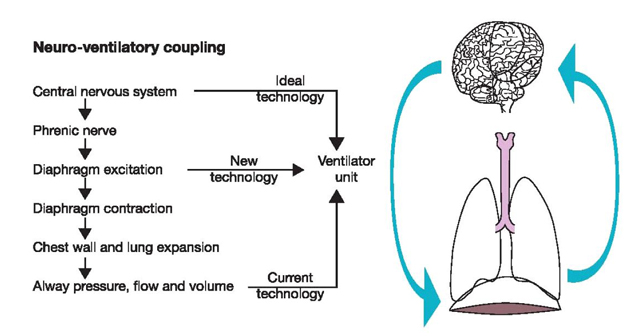
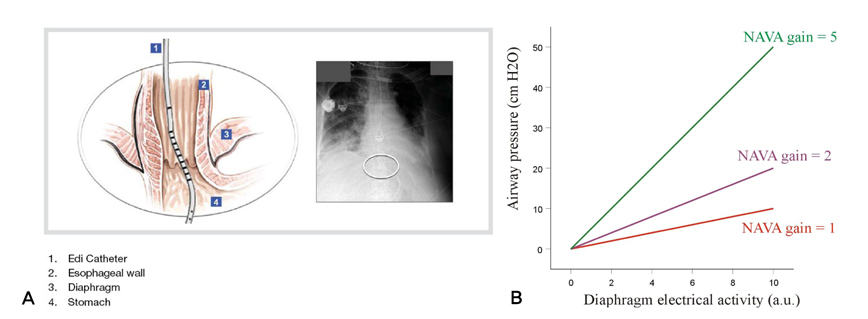
Article35. Sinderby C, Navalesi P, Beck J, et al. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999; 5:1433–1436.
Article36. Beck J, Brander L, Slutsky AS, Reilly MC, Dunn MS, Sinderby C. Non-invasive neurally adjusted ventilatory assist in rabbits with acute lung injury. Intensive Care Med. 2008; 34:316–323.
Article37. Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS, Sinderby C. Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res. 2009; 65:663–668.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspirin vs. Indomethacin in the Treatment of Patent Ductus Arteriosus in Very Low Birth Weight Infants
- Oral Ibuprofen versus Intravenous Indomethacin for the Treatment of Patent Ductus Arteriosus in Very Low Birth Weight Infants
- Therapeutic Strategies for PDA in Prematurity (How to treat PDA? When to treat PDA?)
- Indomethacin therapy in premature infants with patent ductus arteriosus
- PDA Clipping by Using 2mm Thoracoscope