J Korean Neurosurg Soc.
2012 Mar;51(3):173-176. 10.3340/jkns.2012.51.3.173.
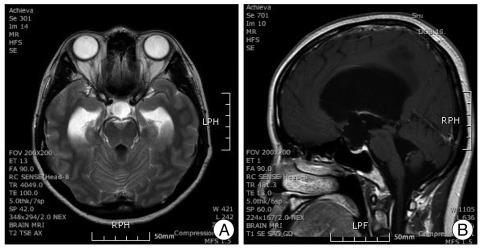
An Acute Postoperative Intractable Hyperventilation after an Endoscopic Third Ventriculostomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Yeungnam University, Daegu, Korea. adjee@med.yu.ac.kr
- 2Department of Neurosurgery, School of Medicine, Yeungnam University, Daegu, Korea.
- KMID: 2018195
- DOI: http://doi.org/10.3340/jkns.2012.51.3.173
Abstract
- This report describes a rare case of postoperative hyperventilation attack after an endoscopic third ventriculostomy in a 46-year-old woman. About 60 min after the termination of the operation, an intractable hyperventilation started with respiratory rate of 65 breaths/min and EtCO2, 16.3 mm Hg. Sedation with benzodiazepine, thiopental sodium, fentanyl, and propofol/remifentanil infusion was tried under a rebreathing mask at a 4 L/min of oxygen. With aggressive sedative challenges, ventilation pattern was gradually returned to normal during the 22 hrs of time after the surgery. A central neurogenic hyperventilation was suspected due to the stimulating central respiratory center by cold acidic irrigation solution during the neuroendoscopic procedure.
MeSH Terms
Figure
Reference
-
1. Adachi YU, Sano H, Doi M, Sato S. Central neurogenic hyperventilation treated with intravenous fentanyl followed by transdermal application. J Anesth. 2007; 21:417–419. PMID: 17680198.
Article2. Fàbregas N, LÓpez A, Valero R, Carrero E, Caral L, Ferrer E. Anesthetic management of surgical neuroendoscopies : usefulness of monitoring the pressure inside the neuroendoscope. J Neurosurg Anesthesiol. 2000; 12:21–28. PMID: 10636616.3. Folgering H. The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis. 1999; 54:365–372. PMID: 10546483.4. Foster GT, Vaziri ND, Sassoon CS. Respiratory alkalosis. Respir Care. 2001; 46:384–391. PMID: 11262557.5. Hales RE, Yudofsky SC. Textbook of clinical psychiatry. 2003. ed 4. Washington D.C.: American Psychiatric Publishing Inc;p. 543–565.6. Hansen NB, Nowicki PT, Miller RR, Malone T, Bickers RG, Menke JA. Alterations in cerebral blood flow and oxygen consumption during prolonged hypocarbia. Pediatr Res. 1986; 20:147–150. PMID: 3080728.
Article7. Jaeckle KA, Digre KB, Jones CR, Bailey PL, McMahill PC. Central neurogenic hyperventilation : pharmacologic intervention with morphine sulfate and correlative analysis of respiratory, sleep, and ocular motor dysfunction. Neurology. 1990; 40:1715–1720. PMID: 2234427.8. Kim G, Bae JH, Lim SW. Hyperventilation attack during recovery from general anesthesia : a case report. Korean J Anesthesiol. 2005; 49:735–738.
Article9. Liebowitz MR, Fyer AJ, Gorman JM, Dillon D, Appleby IL, Levy G, et al. Lactate provocation of panic attacks. I. Clinical and behavioral findings. Arch Gen Psychiatry. 1984; 41:764–770. PMID: 6742978.10. Mason RJ, Broaddus VC, Martin TR, King TE Jr, Schraufnagel DE, Murray JF, et al. Murray & Nadel's textbook of respiratory medicine. 2010. ed 5. Philadelphia: Saunders Elsevier;p. 1842–1847.11. Mizuno J, Morita S, Itou Y, Honda M, Momoeda K, Hanaoka K. [Hyperventilation syndrome before induction of and after awakening from general anesthesia]. Masui. 2009; 58:768–771. PMID: 19522275.12. Plum F, Swanson AG. Central neurogenic hyperventilation in man. AMA Arch Neurol Psychiatry. 1959; 81:535–549.
Article13. Reivich M, Cohen PJ, Greenbaum L. Alterations in the electroencephalogram of awake man produced by hyperventilation : effects of 100% oxygen at 3 atmospheres absolute pressure. Neurology. 1966; 16:304.14. Sung HJ, Sohn JT, Kim JG, Shin IW, Ok SH, Lee HK, et al. Acute respiratory alkalosis occurring after endoscopic third ventriculostomy : a case report. Korean J Anesthesiol. 2010; 59:S194–S196. PMID: 21286439.15. Tomioka S, Takechi M, Ohshita N, Nakajo N. Propofol is not effective for hyperventilation syndrome. Anesth Analg. 2001; 92:781–782. PMID: 11226118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central hyperventilation syndrome due to massive pneumocephalus after endoscopic third ventriculostomy: a case report
- Acute respiratory alkalosis occurring after endoscopic third ventriculostomy: A case report
- Endoscopic Third Ventriculostomy: Success and Failure
- Endoscopic Third Ventriculostomy
- Endoscopic Third Ventriculostomy for Adult Aqueduct Stenosis: Double Fenestration: A Case Report and Technical Note