J Korean Neurosurg Soc.
2014 Nov;56(5):405-409. 10.3340/jkns.2014.56.5.405.
Outcome of Endoscopic Transsphenoidal Surgery in Combination with Somatostatin Analogues in Patients with Growth Hormone Producing Pituitary Adenoma
- Affiliations
-
- 1Department of Neurosurgery, General Hospital of People's Liberation Army, Beijing, China. bainanxu@126.com
- 2Department of Endocrinology, General Hospital of People's Liberation Army, Beijing, China.
- KMID: 2018099
- DOI: http://doi.org/10.3340/jkns.2014.56.5.405
Abstract
OBJECTIVE
To determine the efficacy of endoscopic surgery in combination with long-acting somatostatin analogues (SSAs) in treating patients with growth hormone (GH)-secreting pituitary tumor.
METHODS
We performed retrospective analysis of 133 patients with GH producing pituitary adenoma who underwent pure endoscopic transsphenoidal surgery in our center from January 2007 to July 2012. Patients were followed up for a range of 3-48 months. The radiological remission, biochemical remission and complication were evaluated.
RESULTS
A total of 110 (82.7%) patients achieved radiological complete resection, 11 (8.2%) subtotal resection, and 12 (9.0%) partial resection. Eighty-eight (66.2%) patients showed nadir GH level less than 1 ng/mL after oral glucose administration. No mortality or severe disability was observed during follow up. Preoperative long-acting SSA successfully improved left ventricle ejection fraction (LVEF) and blood glucose in three patients who subsequently underwent success operation. Long-acting SSA (20 mg every 30 days) achieved biochemical remission in 19 out 23 (82.6%) patients who showed persistent high GH level after surgery.
CONCLUSION
Endoscopic transsphenoidal surgery can biochemically cure the majority of GH producing pituitary adenoma. Post-operative use of SSA can improve biochemical remission.
MeSH Terms
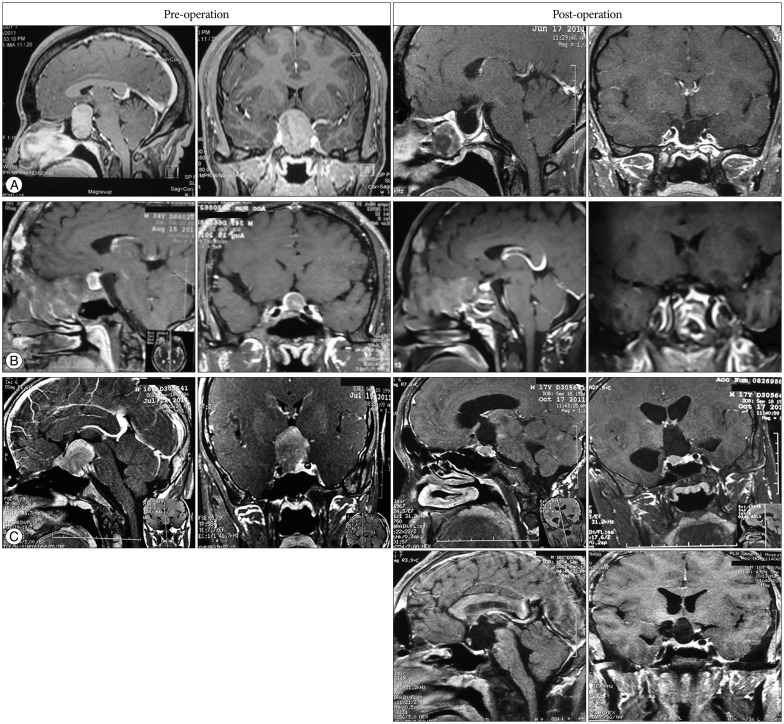
Figure
Cited by 1 articles
-
Parasellar Extension Grades and Surgical Extent in Endoscopic Endonasal Transsphenoidal Surgery for Pituitary Adenomas : A Single Surgeon's Consecutive Series with the Aspects of Reliability and Clinical Validity
Sang-Hyo Lee, Jae-Sung Park, Song Lee, Sung-Won Kim, Yong-Kil Hong
J Korean Neurosurg Soc. 2016;59(6):577-583. doi: 10.3340/jkns.2016.59.6.577.
Reference
-
1. Barker FG 2nd, Klibanski A, Swearingen B. Transsphenoidal surgery for pituitary tumors in the United States, 1996-2000 : mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab. 2003; 88:4709–4719. PMID: 14557445.
Article2. Colao A, Martino E, Cappabianca P, Cozzi R, Scanarini M, Ghigo E. A.L.I.C.E. Study Group. First-line therapy of acromegaly : a statement of the A.L.I.C.E. (Acromegaly primary medical treatment Learning and Improvement with Continuous Medical Education) Study Group. J Endocrinol Invest. 2006; 29:1017–1020. PMID: 17259801.
Article3. Gittoes NJ, Sheppard MC, Johnson AP, Stewart PM. Outcome of surgery for acromegaly--the experience of a dedicated pituitary surgeon. QJM. 1999; 92:741–745. PMID: 10581337.
Article4. Hlavica M, Bellut D, Lemm D, Schmid C, Bernays RL. Impact of ultra-low-field intraoperative magnetic resonance imaging on extent of resection and frequency of tumor recurrence in 104 surgically treated nonfunctioning pituitary adenomas. World Neurosurg. 2013; 79:99–109. PMID: 23043996.
Article5. Hofstetter CP, Mannaa RH, Mubita L, Anand VK, Kennedy JW, Dehdashti AR, et al. Endoscopic endonasal transsphenoidal surgery for growth hormone-secreting pituitary adenomas. Neurosurg Focus. 2010; 29:E6. PMID: 20887131.
Article6. Holdaway IM, Bolland MJ, Gamble GD. A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur J Endocrinol. 2008; 159:89–95. PMID: 18524797.
Article7. Jane JA Jr, Starke RM, Elzoghby MA, Reames DL, Payne SC, Thorner MO, et al. Endoscopic transsphenoidal surgery for acromegaly : remission using modern criteria, complications, and predictors of outcome. J Clin Endocrinol Metab. 2011; 96:2732–2740. PMID: 21715544.
Article8. Katznelson L, Atkinson JL, Cook DM, Ezzat SZ, Hamrahian AH, Miller KK. American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of acromegaly--2011 update. Endocr Pract. 2011; 17(Suppl):1–44. PMID: 21846616.
Article9. Maison P, Tropeano AI, Macquin-Mavier I, Giustina A, Chanson P. Impact of somatostatin analogs on the heart in acromegaly : a metaanalysis. J Clin Endocrinol Metab. 2007; 92:1743–1747. PMID: 17311857.
Article10. Melmed S, Colao A, Barkan A, Molitch M, Grossman AB, Kleinberg D, et al. Guidelines for acromegaly management : an update. J Clin Endocrinol Metab. 2009; 94:1509–1517. PMID: 19208732.11. Nomikos P, Buchfelder M, Fahlbusch R. The outcome of surgery in 668 patients with acromegaly using current criteria of biochemical 'cure'. Eur J Endocrinol. 2005; 152:379–387. PMID: 15757854.
Article12. Pita-Gutierrez F, Pertega-Diaz S, Pita-Fernandez S, Pena L, Lugo G, Sangiao-Alvarellos S, et al. Place of preoperative treatment of acromegaly with somatostatin analog on surgical outcome : a systematic review and meta-analysis. PLoS One. 2013; 8:e61523. PMID: 23634209.13. Plöckinger U, Quabbe HJ. Presurgical octreotide treatment in acromegaly : no improvement of final growth hormone (GH) concentration and pituitary function. A long-term case-control study. Acta Neurochir (Wien). 2005; 147:485–493. discussion 493. PMID: 15806331.
Article14. Rajasoorya C, Holdaway IM, Wrightson P, Scott DJ, Ibbertson HK. Determinants of clinical outcome and survival in acromegaly. Clin Endocrinol (Oxf). 1994; 41:95–102. PMID: 8050136.
Article15. Schwartz TH, Stieg PE, Anand VK. Endoscopic transsphenoidal pituitary surgery with intraoperative magnetic resonance imaging. Neurosurgery. 2006; 58(1 Suppl):ONS44–ONS51. discussion ONS44-ONS51. PMID: 16479628.
Article16. Shen M, Shou X, Wang Y, Zhang Z, Wu J, Mao Y, et al. Effect of presurgical long-acting octreotide treatment in acromegaly patients with invasive pituitary macroadenomas : a prospective randomized study. Endocr J. 2010; 57:1035–1044. PMID: 21099129.
Article17. Wu JS, Shou XF, Yao CJ, Wang YF, Zhuang DX, Mao Y, et al. Transsphenoidal pituitary macroadenomas resection guided by PoleStar N20 low-field intraoperative magnetic resonance imaging : comparison with early postoperative high-field magnetic resonance imaging. Neurosurgery. 2009; 65:63–70. discussion 70-71. PMID: 19574826.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endocrine Outcome of Endoscopic Endonasal Transsphenoidal Surgery in Functioning Pituitary Adenomas
- Clinical Characteristics and Treatments of Patients with TSH Secreting Pituitary Adenoma
- Gigantism caused by growth hormone secreting pituitary adenoma
- Deliberate Two-Staged Endoscopic Endonasal Transsphenoidal Surgery in Large Pituitary Adenomas
- The mechanism of Arginine-stimulated growth hormone secretion