Ann Pediatr Endocrinol Metab.
2014 Jun;19(2):96-99. 10.6065/apem.2014.19.2.96.
Gigantism caused by growth hormone secreting pituitary adenoma
- Affiliations
-
- 1Department of Pediatrics, Chonnam National University Hospital & Medical School, Gwangju, Korea. cjkim@jnu.ac.kr
- KMID: 1803861
- DOI: http://doi.org/10.6065/apem.2014.19.2.96
Abstract
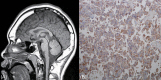
- Gigantism indicates excessive secretion of growth hormones (GH) during childhood when open epiphyseal growth plates allow for excessive linear growth. Case one involved a 14.7-year-old boy presented with extreme tall stature. His random serum GH level was 38.4 ng/mL, and failure of GH suppression was noted during an oral glucose tolerance test (OGTT; nadir serum GH, 22.7 ng/mL). Magnetic resonance imaging (MRI) of the brain revealed a 12-mm-sized pituitary adenoma. Transsphenoidal surgery was performed and a pituitary adenoma displaying positive immunohistochemical staining for GH was reported. Pituitary MRI scan was performed 4 months after surgery and showed recurrence/residual tumor. Medical treatment with a long-acting somatostatin analogue for six months was unsuccessful. As a result, secondary surgery was performed. Three months after reoperation, the GH level was 0.2 ng/mL and insulin-like growth factor 1 was 205 ng/mL. Case two involved a 14.9-year-old boy, who was referred to our department for his tall stature. His basal GH level was 9.3 ng/mL, and failure of GH suppression was reported during OGTT (nadir GH, 9.0 ng/mL). Pituitary MRI showed a 6-mm-sized pituitary adenoma. Surgery was done and histopathological examination demonstrated a pituitary adenoma with positive staining for GH. Three months after surgery, the GH level was 0.2 ng/mL and nadir GH during OGTT was less than 0.1 ng/mL. Pituitary MRI scans showed no residual tumor. We present two cases of gigantism caused by a GH-secreting pituitary adenoma with clinical and microscopic findings.
Keyword
MeSH Terms
Figure
Reference
-
1. Eugster EA, Pescovitz OH. Gigantism. J Clin Endocrinol Metab. 1999; 84:4379–4384. PMID: 10599691.
Article2. Whitehead EM, Shalet SM, Davies D, Enoch BA, Price DA, Beardwell CG. Pituitary gigantism: a disabling condition. Clin Endocrinol (Oxf). 1982; 17:271–277. PMID: 7165969.
Article3. Kane LA, Leinung MC, Scheithauer BW, Bergstralh EJ, Laws ER Jr, Groover RV, et al. Pituitary adenomas in childhood and adolescence. J Clin Endocrinol Metab. 1994; 79:1135–1140. PMID: 7525627.
Article4. Artese R, D'Osvaldo DH, Molocznik I, Benencia H, Oviedo J, Burdman JA, et al. Pituitary tumors in adolescent patients. Neurol Res. 1998; 20:415–417. PMID: 9664587.5. Abe T, Tara LA, Ludecke DK. Growth hormone-secreting pituitary adenomas in childhood and adolescence: features and results of transnasal surgery. Neurosurgery. 1999; 45:1–10. PMID: 10414559.
Article6. Melmed S, Ho K, Klibanski A, Reichlin S, Thorner M. Clinical review 75: recent advances in pathogenesis, diagnosis, and management of acromegaly. J Clin Endocrinol Metab. 1995; 80:3395–3402. PMID: 8530571.
Article7. Dyer EH, Civit T, Visot A, Delalande O, Derome P. Transsphenoidal surgery for pituitary adenomas in children. Neurosurgery. 1994; 34:207–212. PMID: 8177379.
Article8. Rix M, Laurberg P, Hoejberg AS, Brock-Jacobsen B. Pegvisomant therapy in pituitary gigantism: successful treatment in a 12-year-old girl. Eur J Endocrinol. 2005; 153:195–201. PMID: 16061823.
Article9. Greulich WW, Pyle SI. Radiographic skeletal development of the hand and wrist. 2nd ed. Stanford: Stanford University Press;1959.10. Pandey P, Ojha BK, Mahapatra AK. Pediatric pituitary adenoma: a series of 42 patients. J Clin Neurosci. 2005; 12:124–127. PMID: 15749410.
Article11. Gelber SJ, Heffez DS, Donohoue PA. Pituitary gigantism caused by growth hormone excess from infancy. J Pediatr. 1992; 120:931–934. PMID: 1593354.
Article12. Kim HY, Jung HW, Lee J, Yoon JY, Lee YA, Shin CH, et al. Childhood onset pituitary adenoma: clinical presentations and outcomes of 24 cases. Ann Pediatr Endocrinol Metab. 2012; 17:82–91.
Article13. Kim EY, Choi JU, Chung SS, Lee KC, Kim DH. Pituitary adenomas in childhood and adolescence. J Korean Neurosurg Soc. 1995; 24:864–875.14. Melmed S. Medical progress: acromegaly. N Engl J Med. 2006; 355:2558–2573. PMID: 17167139.15. Sata A, Ho KK. Growth hormone measurements in the diagnosis and monitoring of acromegaly. Pituitary. 2007; 10:165–172. PMID: 17458702.
Article16. Schoof E, Dorr HG, Kiess W, Ludecke DK, Freitag E, Zindel V, et al. Five-year follow-up of a 13-year-old boy with a pituitary adenoma causing gigantism: effect of octreotide therapy. Horm Res. 2004; 61:184–189. PMID: 14739526.
Article17. Barrande G, Pittino-Lungo M, Coste J, Ponvert D, Bertagna X, Luton JP, et al. Hormonal and metabolic effects of radiotherapy in acromegaly: long-term results in 128 patients followed in a single center. J Clin Endocrinol Metab. 2000; 85:3779–3785. PMID: 11061538.
Article18. Ayuk J, Stewart SE, Stewart PM, Sheppard MC. European Sandostatin LAR Group. Efficacy of Sandostatin LAR (long-acting somatostatin analogue) is similar in patients with untreated acromegaly and in those previously treated with surgery and/or radiotherapy. Clin Endocrinol (Oxf). 2004; 60:375–381. PMID: 15009004.
Article19. Bevan JS, Atkin SL, Atkinson AB, Bouloux PM, Hanna F, Harris PE, et al. Primary medical therapy for acromegaly: an open, prospective, multicenter study of the effects of subcutaneous and intramuscular slow-release octreotide on growth hormone, insulin-like growth factor-I, and tumor size. J Clin Endocrinol Metab. 2002; 87:4554–4563. PMID: 12364434.
Article