J Korean Soc Spine Surg.
2009 Sep;16(3):202-209. 10.4184/jkss.2009.16.3.202.
Clinical Significance of the Radiolucent Zone Around the Pedicle Screws in the Lumbar Degenerative Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@dau.ac.kr
- KMID: 2003115
- DOI: http://doi.org/10.4184/jkss.2009.16.3.202
Abstract
- STUDY DESIGN: A retrospective study.
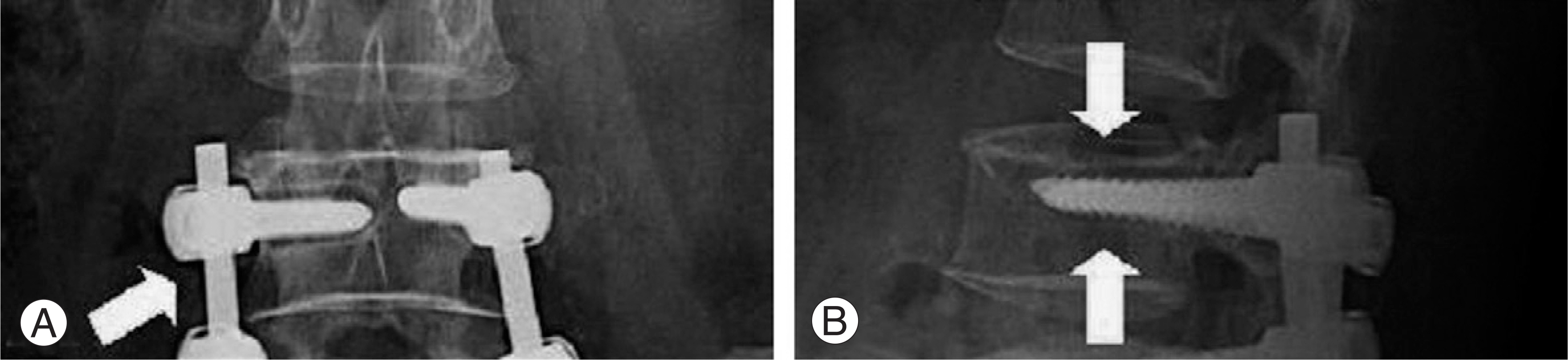
OBJECTIVE
To analyze the clinical significance of the radiolucent zones surrounding pedicle screws. SUMMARY OF LITERATURE REVIEW: Clear zones have been suggested in pseudoarthrosis and a loss of fixation. However, few reports have clearly described the long-term course and clinical significance of clear zones. MATERIALS AND METHODS: The clear zones were evaluated in 399 patients with pedicle screw fixation after 6 months, 1 year, 2 years and 3 years. The patient was considered to be clear zone positive when 1 mm or greater circumferential lucency was confirmed around a screw on film from 2 or more directions. The time-course of the clear zones was examined with regard to age, number of levels fused, bone union, fusion method and reoperation.
RESULTS
After 6 months, clear zones were observed in 124 patients (31.1%) but the clear zone-positive rate decreased with time. Clear zones were observed in 89 patients(22.3%), 44 patients(11.0%) and 41 patients(10.3%) after 1 year, 2 years and 3 years, respectively. No new clear zones had developed after 6 months. At the final follow-up, pseudoarthrosis was observed in 12 patients(3.0%). Among them, 11 were clear zone-positive and 1 was clear zone-negative. There was a statistically significant relationship between the clear zone-positive rate and multi-levels, older age and nonunion during following up. In addition, there was a relatively lower clear zone-positive rate in posterolateral fusion combined with posterior lumbar interbody fusion than only posterolateral fusion. However, the difference between them was not statistically significant.
CONCLUSION
The presence of clear zones does not always mean pseudoarthrosis but clear zones persisting for more than 2 years after surgery have a higher rate of pseudoarthrosis.
Figure
Reference
-
1). Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008; 33:903–908.
Article2). Fischgrund JS, Mackay M, Herkowitz HN, et al. .:. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997; 22:2807–2812.3). Tokuhashi Y, Nishimura T, Matsuzaki Y. Clinical results of more than 10 years after posterolateral fusion with pedicle screw fixation for degenerative lumbar spondylolisthesis. Spine. 2004; 17:185–192.4). Bae SW, Kwak HY, Song BY, Yoo JC, An YJ. Radiolucent Zones Surrounding Transpedicular Screws After Lumbar Spinal Instrumented Fusion. J Korean Soc Spine Surg. 2005; 12:115–122.
Article5). Alanay A, Vyas R, Shamie AN, Sciocia T, Randolph G, Wang JC. Safety and efficacy of implant removal for patients with recurrent back pain after a failed degenerative lumbar spine surgery. J Spinal Disord Tech. 2007; 20:271–277.
Article6). Sande′n B, Olerud C, Petren-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrouding pedicle screws. Definition of screw loosenins in spinal instrumentation. J Bone Joint Surg Br. 2004; 86:457–461.7). Slone RM, MacMillan M, Montgomery WJ. Spinal fixation. Part3. Complications of spinal instrumentation. Radiographics. 1993; 13:797–816.8). Ozawa T, Takahashi K, Yamagata M, et al. .:. Insertional torque of the lumbar pedicle screw during surgery. J Orthop Sci. 2005; 10:133–136.
Article9). Steinmann JC, Herkowitz HN. Pseudoarthrosis of the spine. Clin Orthop Relat Res. 1992; 284:80–90.10). Jang EC, Hwan SJ, Song KS, Ryu HS. A Biomechanical Study of Two Kinds of Tapered Pedicle Screws in Osteoporotic Lumber Spine. J Korean Orthop Assoc. 1999; 34:955–962.
Article11). Kant AP, Daum WJ, Dean SM, Uchida T. Evaluation of lumbar spine fusion. Plain radiographs versus direct surgical exploration and observation. Spine. 1995; 21:2313–2317.12). Foley MJ, Calenoff L, Hendrix RW, Schafer MF. Thoracic and lumbar spine fusion: postoperative radiologic evaluation. Am J Roentgenol. 1983; 141:373–380.
Article13). C Lee, J Dorcil, TE Radomisli. Nonunion of the spine: A Review. Clin Orthop Relat Res. 2004; 419:71–75.14). Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K. A 10-year followup evaluation of lumbar spine fusion with pedicle screw fixation. Spine. 2003; 28:1390–1395.
Article15). Kim NH, Lee HM, Lee WS. The effect of bone mineral density on instrumented spine fusion. J Kor Spine Surg. 1994; 1:133–139.16). Pihlajamaki H, Myllynen P, Bostman O. Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Joint Surg Br. 1997; 79:183–189.17). Cook SD, Barbera J, Rubi M, Salkeld SL, Whitecloud TS 3rd. Lumbosacral fixation using expandable pedicle screws. an alternative in reoperation and osteoporosis. Spine J. 2001; 1:109–114.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does a Radiolucent Zone Surrounding the Pedicle Screws mean Nonunion?
- Pseudarthrosis at L5-S1 after Posterolateral Lumbar Fusion
- Radiolucent Zones Surrounding Transpedicular Screws After Lumbar Spinal Instrumented Fusion
- Cotrel - Dubousset Pedicle Screw Fixation After Posterior Decompression of Lumbar Spinal Stenosis
- Does the Addition of a Dynamic Pedicle Screw to a Fusion Segment Prevent Adjacent Segment Pathology in the Lumbar Spine?