J Clin Neurol.
2013 Oct;9(4):259-268. 10.3988/jcn.2013.9.4.259.
Early Diagnosis and Management of Cerebral Venous Flow Obstruction Secondary to Transsinus Fracture after Traumatic Brain Injury
- Affiliations
-
- 1Department of Neurosurgery, 175th Hospital of PLA, Affiliated Southeast Hospital of Xiamen University, Zhangzhou, Fujian, China. wenhao_wang0712@126.com
- KMID: 1980546
- DOI: http://doi.org/10.3988/jcn.2013.9.4.259
Abstract
- BACKGROUND AND PURPOSE
Cerebral venous flow obstruction (CVFO) is a fatal complication of traumatic brain injury. To compare the outcomes of patients with CVFO secondary to traumatic-brain-injury-induced transsinus fracture who were diagnosed early versus those diagnosed late in the therapeutic course.
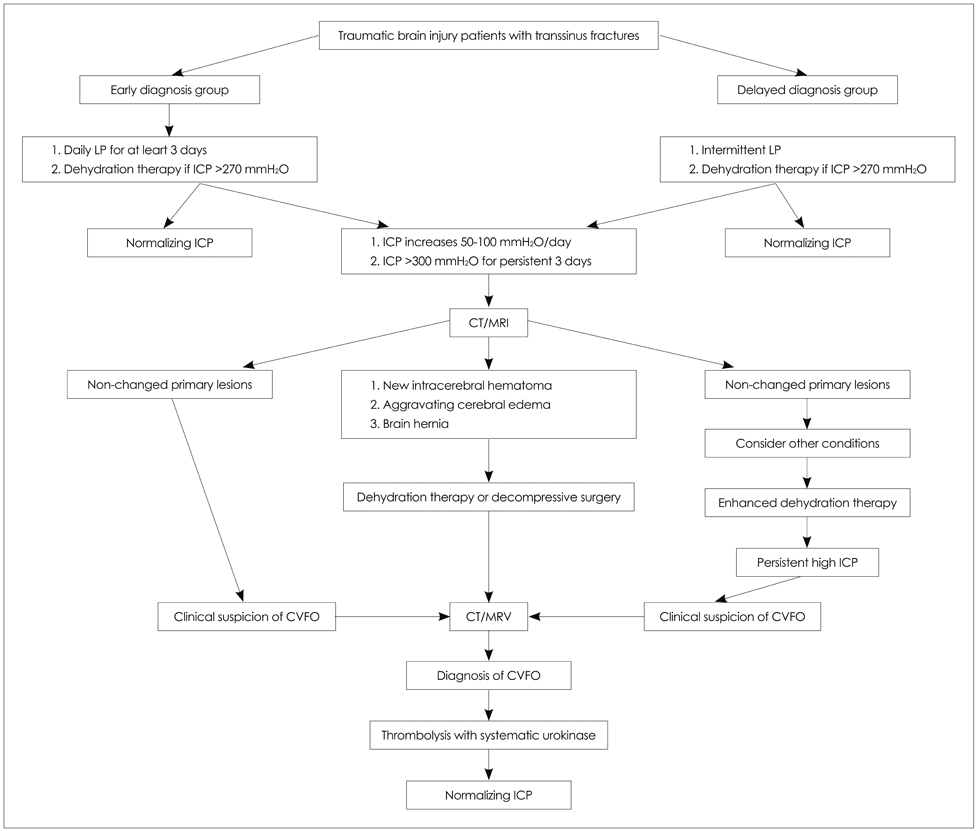
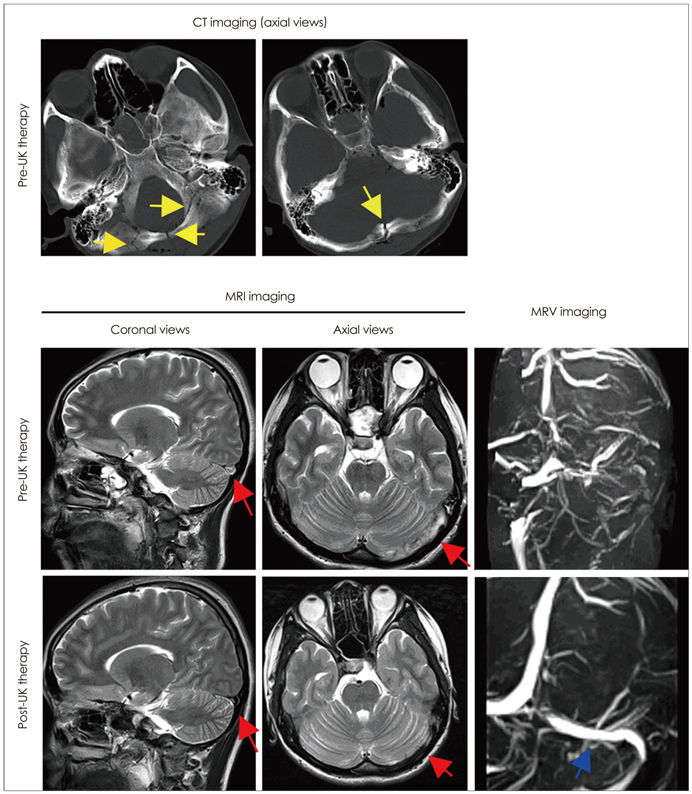
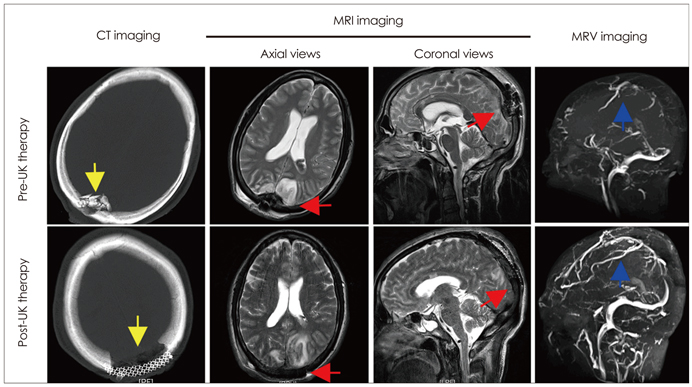
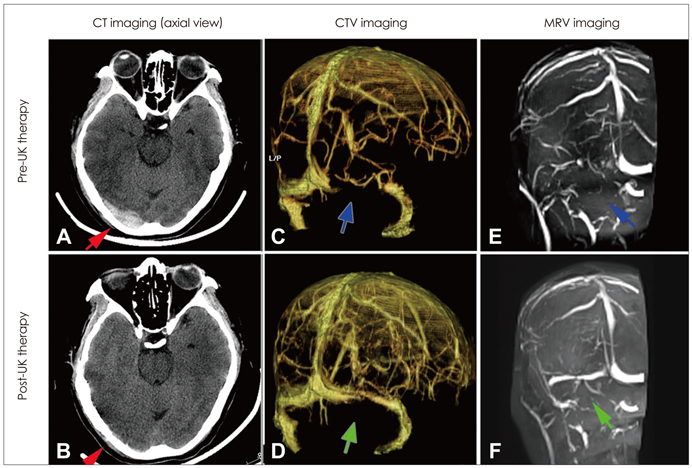
METHODS
In total, 403 patients with transsinus fracture were reviewed retrospectively. The patients were divided into an early-diagnosis group (n=338) and a delayed-diagnosis group (n=65). The patients submitted to 2D time-of-flight magnetic resonance venography (2D-TOF MRV) and/or CT venography (CTV), depending upon the findings of intracranial pressure monitoring, in order to identify potentially complicated CVFO. These examinations took place within 3 days of the onset of malignant intracranial hypertension symptoms in the early-diagnosis group, and after an average of 7 days in the delayed-diagnosis group. Once diagnosed, patients received intravenous thrombolytic therapy with low-dose urokinase. Patients with massive transsinus epidural hematoma, depressed fracture, or cerebral hernia were treated surgically to relieve the compression and repair any damage to the venous sinuses.
RESULTS
Cerebral venous flow obstruction was much more severe in the delayed-diagnosis group than in the early-diagnosis group (p<0.001), and hence patients in the former group were given a higher dose of urokinase (p<0.001) for thrombolytic therapy. They were also significantly more likely to need surgery (48.1% vs. 20.6%, p=0.003) and had a higher mortality rate (37.0% vs. 4.1%, p<0.001). However, patients in both groups experienced a similarly favorable prognosis, not only with regard to functional outcome but also with respect to neuroradiological improvement, as evaluated by 2D-TOF MRV/CTV at the final follow-up (p=0.218).
CONCLUSIONS
Delayed diagnosis can result in increased risk of surgery and death in the acute phase. Thrombolytic therapy with low-dose urokinase resulted in promising improvements in both functional and neuroradiological outcomes in all of the patients in this study, regardless of the time to diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Saadatnia M, Fatehi F, Basiri K, Mousavi SA, Mehr GK. Cerebral venous sinus thrombosis risk factors. Int J Stroke. 2009; 4:111–123.
Article2. Gosk-Bierska I, Wysokinski W, Brown RD Jr, Karnicki K, Grill D, Wiste H, et al. Cerebral venous sinus thrombosis: incidence of venous thrombosis recurrence and survival. Neurology. 2006; 67:814–819.
Article3. Borhani Haghighi A, Edgell RC, Cruz-Flores S, Feen E, Piriyawat P, Vora N, et al. Mortality of cerebral venous-sinus thrombosis in a large national sample. Stroke. 2012; 43:262–264.
Article4. Guenther G, Arauz A. Cerebral venous thrombosis: a diagnostic and treatment update. Neurologia. 2011; 26:488–498.
Article5. Bousser MG, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol. 2007; 6:162–170.
Article6. McBane RD 2nd, Tafur A, Wysokinski WE. Acquired and congenital risk factors associated with cerebral venous sinus thrombosis. Thromb Res. 2010; 126:81–87.
Article7. Elsankari S, Czosnyka M, Lehmann P, Meyer ME, Deramond H, Balédent O. Cerebral blood and CSF flow patterns in patients diagnosed for cerebral venous thrombosis - an observational study. J Clin Imaging Sci. 2012; 2:41.
Article8. Fuentes S, Metellus P, Levrier O, Adetchessi T, Dufour H, Grisoli F. Depressed skull fracture overlying the superior sagittal sinus causing benign intracranial hypertension. Description of two cases and review of the literature. Br J Neurosurg. 2005; 19:438–442.
Article9. Delgado Almandoz JE, Kelly HR, Schaefer PW, Lev MH, Gonzalez RG, Romero JM. Prevalence of traumatic dural venous sinus thrombosis in high-risk acute blunt head trauma patients evaluated with multidetector CT venography. Radiology. 2010; 255:570–577.
Article10. Yiğit H, Turan A, Ergün E, Koşar P, Koşar U. Time-resolved MR angiography of the intracranial venous system: an alternative MR venography technique. Eur Radiol. 2012; 22:980–989.
Article11. Widjaja E, Shroff M, Blaser S, Laughlin S, Raybaud C. 2D time-of-flight MR venography in neonates: anatomy and pitfalls. AJNR Am J Neuroradiol. 2006; 27:1913–1918.12. Lewin JS, Masaryk TJ, Smith AS, Ruggieri PM, Ross JS. Time-of-flight intracranial MR venography: evaluation of the sequential oblique section technique. AJNR Am J Neuroradiol. 1994; 15:1657–1664.13. Qu H, Yang M. Early imaging characteristics of 62 cases of cerebral venous sinus thrombosis. Exp Ther Med. 2013; 5:233–236.
Article14. Linn J, Pfefferkorn T, Ivanicova K, Müller-Schunk S, Hartz S, Wiesmann M, et al. Noncontrast CT in deep cerebral venous thrombosis and sinus thrombosis: comparison of its diagnostic value for both entities. AJNR Am J Neuroradiol. 2009; 30:728–735.
Article15. Grosman H, St Louis EL, Gray RR. The role of CT and DSA in cranial sino-venous occlusion. Can Assoc Radiol J. 1987; 38:183–189.16. Fukusumi A, Okudera T, Takahashi S, Taoka T, Sakamoto M, Nakagawa H, et al. Anatomical evaluation of the dural sinuses in the region of the torcular herophili using three dimensional CT venography. Acad Radiol. 2010; 17:1103–1111.
Article17. Alper F, Kantarci M, Dane S, Gumustekin K, Onbas O, Durur I. Importance of anatomical asymmetries of transverse sinuses: an MR venographic study. Cerebrovasc Dis. 2004; 18:236–239.
Article18. D'Alise MD, Fichtel F, Horowitz M. Sagittal sinus thrombosis following minor head injury treated with continuous urokinase infusion. Surg Neurol. 1998; 49:430–435.19. Novak Z, Coldwell DM, Brega KE. Selective infusion of urokinase and thrombectomy in the treatment of acute cerebral sinus thrombosis. AJNR Am J Neuroradiol. 2000; 21:143–145.20. Wasay M, Bakshi R, Kojan S, Bobustuc G, Dubey N, Unwin DH. Nonrandomized comparison of local urokinase thrombolysis versus systemic heparin anticoagulation for superior sagittal sinus thrombosis. Stroke. 2001; 32:2310–2317.
Article21. Nimjee SM, Powers CJ, Kolls BJ, Smith T, Britz GW, Zomorodi AR. Endovascular treatment of venous sinus thrombosis: a case report and review of the literature. J Neurointerv Surg. 2011; 3:30–33.
Article22. Zhao X, Rizzo A, Malek B, Fakhry S, Watson J. Basilar skull fracture: a risk factor for transverse/sigmoid venous sinus obstruction. J Neurotrauma. 2008; 25:104–111.
Article23. Dabscheck G, Mackay M, Coleman L, Lo P. Isolated intracranial hypertension as a late manifestation of sinus venous compression secondary to a depressed skull fracture. J Child Neurol. 2007; 22:344–347.
Article24. Yokota H, Eguchi T, Nobayashi M, Nishioka T, Nishimura F, Nikaido Y. Persistent intracranial hypertension caused by superior sagittal sinus stenosis following depressed skull fracture. Case report and review of the literature. J Neurosurg. 2006; 104:849–852.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Controversies in Acute Care of Patients with Severe Traumatic Brain Injury
- Traumatic Intracranial Aneurysms: Report of Six Cases
- Clinical Experiences of Traumatic Intracranial Aneurysms
- Management of Head Injury in the Emergency Department
- Anesthetic management of the traumatic brain injury patients undergoing non-neurosurgery