J Cerebrovasc Endovasc Neurosurg.
2014 Sep;16(3):241-246. 10.7461/jcen.2014.16.3.241.
Clinicoepidemiological Features of Asymptomatic Moyamoya Disease in Adult Patients
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea. nsbang@snubh.org
- 2Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea.
- 3Department of Neurosurgery, Suseong Metro Hospital, Taegu, Korea.
- KMID: 1963162
- DOI: http://doi.org/10.7461/jcen.2014.16.3.241
Abstract
OBJECTIVE
The aim of this study was to document the natural course of asymptomatic adult moyamoya disease (MMD) and the factors related to disease progression to aid in treatment decisions.
MATERIALS AND METHODS
Among 459 adult MMD patients (aged > or = 20 years), 42 patients were included in this retrospective cohort study. Clinical records of adult asymptomatic MMD patients (n = 42) and follow-up data from September 2013 were reviewed to determine the factors related to disease progression.
RESULTS
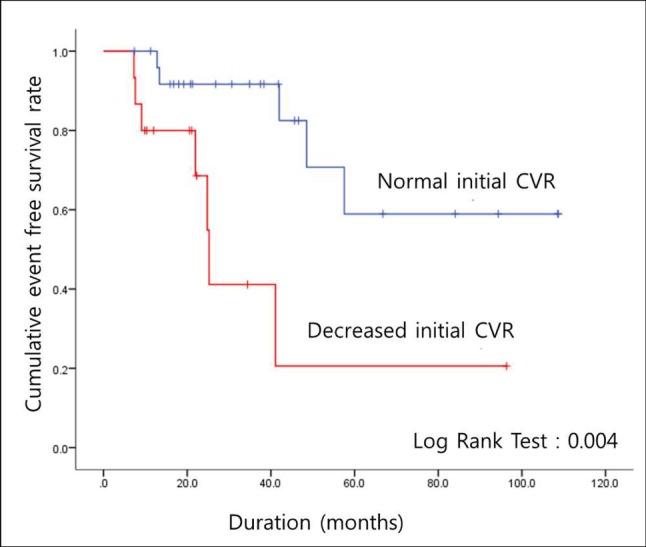
The mean age of patients at the time of diagnosis was 41.2 years (range, 23-64 years), and the mean follow-up period was 37.3 months (range, 7.4-108.7 months). Of the 42 patients and 75 hemispheres, there were 12 patients (28.6%) and 13 hemispheres (17.3%) with disease progression. There were four hemispheres (5.3%) with symptomatic progression (three hemorrhage, one transient ischemic attack) and nine hemispheres (12.0%) with asymptomatic radiographic progression. There were no relationships with sex, diabetes, hypertension, thyroid disease, family history of MMD, or family history of stroke. However, reduced initial cerebrovascular reserve capacity was observed in seven hemispheres (9.3%) in patients with disease progression. A relationship was found between disease progression and initial cerebrovascular reserve capacity (p = 0.05). None of the patients underwent bypass surgery during the follow-up period.
CONCLUSION
It appears that asymptomatic adult MMD is not a permanent stable disease. In particular, reduced cerebrovascular reserve capacity is an indication of MMD progression, so close regular observation is needed.
MeSH Terms
Figure
Reference
-
1. Fukui M. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ('moyamoya' disease). Research committee on spontaneous occlusion of the circle of Willis (Moyamoya disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S238–S240. PMID: 9409446.2. Fung LW, Thompson D, Ganesan V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Childs Nerv Syst. 2005; 5. 21(5):358–364. PMID: 15696334.
Article3. Han DH, Nam DH, Oh CW. Moyamoya disease in adults: characteristics of clinical presentation and outcome after encephalo-duro-arterio-synangiosis. Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S151–S155. PMID: 9409427.4. Horie N, Morikawa M, Nozaki A, Hayashi K, Suyama K, Nagata I. "Brush Sign" on susceptibility-weighted MR imaging indicates the severity of moyamoya disease. AJNR Am J Neuroradiol. 2011; 10. 32(9):1697–1702. PMID: 21799039.
Article5. Jea A, Smith ER, Robertson R, Scott RM. Moyamoya syndrome associated with Down syndrome: outcome after surgical revascularization. Pediatrics. 2005; 11. 116(5):e694–e701. PMID: 16263984.
Article6. Jo KI, Yeon JY, Hong SC, Kim JS. Clinical course of asymptomatic adult moyamoya disease. Cerebrovasc Dis. 2014; 37(2):94–101. PMID: 24435045.
Article7. Kim SK, Seol HJ, Cho BK, Hwang YS, Lee DS, Wang KC. Moyamoya disease among young patients: its aggressive clinical course and the role of active surgical treatment. Neurosurgery. 2004; 4. 54(4):840–844. discussion 844-6. PMID: 15046649.
Article8. Kuriyama S, Kusaka Y, Fujimura M, Wakai K, Tamakoshi A, Hashimoto S, et al. Prevalence and clinicoepidemiological features of moyamoya disease in Japan: findings from a nationwide epidemiological survey. Stroke. 2008; 1. 39(1):42–47. PMID: 18048855.9. Kuroda S, Hashimoto N, Yoshimoto T, Iwasaki Y. Research committee on moyamoya disease in Japan. Radiological findings, clinical course, and outcome in asymptomatic moyamoya disease: results of multicenter survey in Japan. Stroke. 2007; 5. 38(5):1430–1435. PMID: 17395863.10. Lin N, Baird L, Koss M, Kopecky KE, Gone E, Ullrich NJ, et al. Discovery of asymptomatic moyamoya arteriopathy in pediatric syndromic populations: radiographic and clinical progression. Neurosurg Focus. 2011; 12. 31(6):E6.
Article11. Nanba R, Kuroda S, Takeda M, Shichinohe H, Nakayama N, Ishikawa T, et al. [Clinical features and outcomes of 10 asymptomatic adult patients with moyamoya disease]. No Shinkei Geka. 2003; 12. 31(12):1291–1295. Japanese. PMID: 14719442.12. Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, et al. Management of stroke in infants and children: a scientific statement from a special writing group of the American Heart Association Stroke Council and the Council on cardiovascular disease in the young. Stroke. 2008; 9. 39(9):2644–2691. PMID: 18635845.13. Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009; 3. 360(12):1226–1237. PMID: 19297575.
Article14. Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg. 2004; 2. 100(2 Suppl Pediatrics):142–149. PMID: 14758941.
Article15. Suzuki J, Takaku A. Cerebrovascular "moyamoya" disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969; 3. 20(3):288–299. PMID: 5775283.