J Korean Foot Ankle Soc.
2015 Mar;19(1):23-26. 10.14193/jkfas.2015.19.1.23.
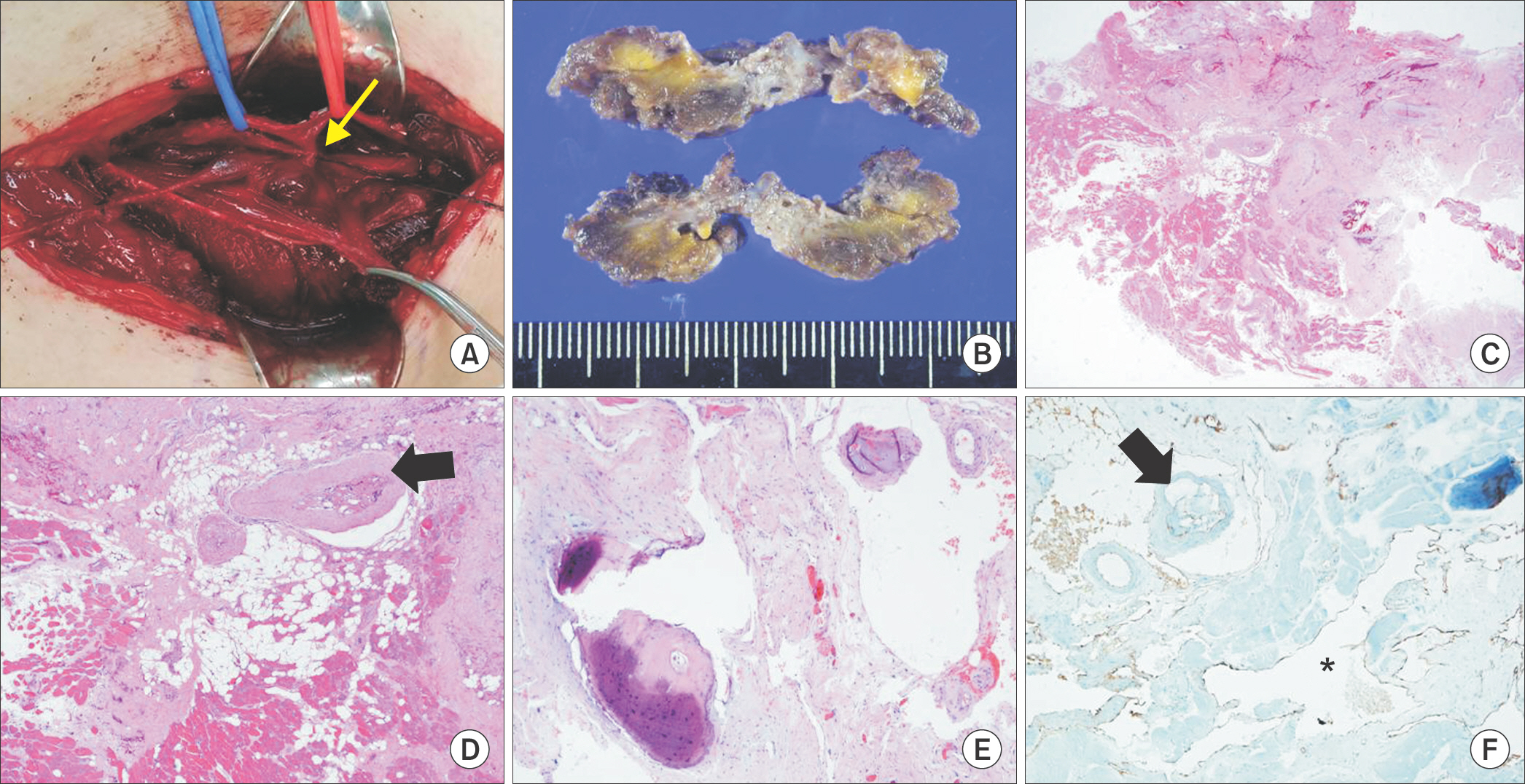
Hybrid Operation for Arteriovenous Malformation in Left Soleus Muscle with Embolization of Feeding Artery and En Bloc Resection: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 2Department of Surgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. ultravascsurg@gmail.com
- 3Department of Radiology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 4Department of Pathology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 1958701
- DOI: http://doi.org/10.14193/jkfas.2015.19.1.23
Abstract
- Arteriovenous malformations (AVMs) are characterized by the presence of abnormal connections between feeding arteries and draining veins. It is generally assumed that symptomatic lesions can preferably be treated. Due to high arterial blood flow, there is a risk of bleeding with surgical excision alone, which can be massive and life threatening during the operation. According to recent advances in interventional technique, a hybrid approach using embolization of the feeding artery with subsequent immediate excision of the AVM for successful management of vascular lesions could be applied to AVMs. Herein, we describe a case of successful excision of AVM in the left soleus muscle using a hybrid approach.
MeSH Terms
Figure
Reference
-
1.Kim JY., Kim DI., Do YS., Lee BB., Kim YW., Shin SW, et al. Surgical treatment for congenital arteriovenous malformation: 10 years’ experience. Eur J Vasc Endovasc Surg. 2006. 32:101–6.
Article2.Hristov N., Atanasov Z., Zafirovski G., Mitrev Z. Intramuscular cavernous hemangioma in the left soleus muscle: successful surgical treatment. Interact Cardiovasc Thorac Surg. 2011. 13:521–2.
Article3.Mendonca DA., McCafferty I., Nishikawa H., Lester R. Venous malformations of the limbs: the Birmingham experience, comparisons and classification in children. J Plast Reconstr Aesthet Surg. 2010. 63:383–9.
Article4.Nazzi V., Messina G., Dones I., Ferroli P., Broggi G. Surgical removal of intramuscular arteriovenous hemangioma of the upper left forearm compressing radial nerve branches. J Neurosurg. 2008. 108:808–11.
Article5.Kim DH., Hwang M., Kang YK., Kim IJ., Park YK. Intramuscular hemangioma mimicking myofascial pain syndrome: a case re-port. J Korean Med Sci. 2007. 22:580–2.
Article6.Belov S. Anatomopathological classification of congenital vascular defects. Semin Vasc Surg. 1993. 6:219–24.7.Lee BB. Critical issues in management of congenital vascular malformation. Ann Vasc Surg. 2004. 18:380–92.
Article8.Choke E., McCarthy M. Hybrid procedures in vascular surgery: converging technique to improve results. J Cardiovasc Surg (To-rino). 2010. 51:857–9.9.Rockman CB., Rosen RJ., Jacobowitz GR., Weiswasser J., Hofstee DJ., Fioole B, et al. Transcatheter embolization of extremity vascular malformations: the long-term success of multiple inter-ventions. Ann Vasc Surg. 2003. 17:417–23.
Article10.Richter GT., Suen JY. Clinical course of arteriovenous malformations of the head and neck: a case series. Otolaryngol Head Neck Surg. 2010. 142:184–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative embolization and en bloc resection of a metastatic pheochromocytoma of the cervical spine
- Embolization of a Bleeding Maxillary Arteriovenous Malformation via the Superficial Temporal Artery after External Carotid Artery Ligation
- A Case of Arteriovenous Malformation of the Nasal Tip
- A Case of Multiple Pulmonary Arteriovenous Malformation Treated with Coil Embolization
- Successful Treatment of a Large Pulmonary Arteriovenous Malformation by Repeated Coil Embolization